Bayliss effect
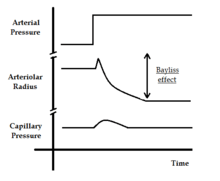
Bayliss effect or Bayliss myogenic response is a special manifestation of the myogenic tone in the vasculature. The Bayliss effect in vascular smooth muscles cells is a response to stretch. This is especially relevant in arterioles of the body. When blood pressure is increased in the blood vessels and the blood vessels distend, they react with a constriction; this is the Bayliss effect. Stretch of the muscle membrane opens a stretch-activated ion channel. The cells then become depolarized and this results in a Ca2+ signal and triggers muscle contraction. It is important to understand that no action potential is necessary here; the level of entered calcium affects the level of contraction proportionally and causes tonic contraction. The contracted state of the smooth muscle depends on the grade of stretch and plays an important part in the regulation of blood flow.
Increased contraction increases the total peripheral resistance (TPR) and this further increases the mean arterial pressure (MAP). This is explained by the following equation: where CO is the cardiac output which is the volume of blood pumped by the heart in one minute.
This effect is independent of nervous mechanisms and that is how we differentiate it from the myogenic tone, which is controlled by the sympathetic nervous system.
The overall effect of the myogenic response (Bayliss effect) is to decrease blood flow across a vessel after an increase in blood pressure.
History
The Bayliss effect was discovered by physiologist Sir William Bayliss in 1902.
Proposed mechanism
When the endothelial cell in the tunica intima of an artery is stretched it is likely that the endothelial cell may signal constriction to the muscle cell layer in a paracrine fashion. Increase in blood pressure may cause depolarisation of the affected myocytes as well or endothelial cells alone. The mechanism is not yet completely understood, but studies have shown that volume regulated chloride channels and stretch sensitive non-selective cation channels lead to an increased probability in opening of L-type (voltage-dependent) Ca2+ channels, thus raising the cytosolic concentration of Ca2+ leading to a contraction of the myocyte, and this may involve other channels in the endothelia.
References
- J. R. Levick. An introduction to cardiac physiology. ISBN 0-340-76376-0.
- A. FONYO. Principals of medical physiology. ISBN 963-242-726-2.