Bronchial thermoplasty
Bronchial Thermoplasty, delivered by the Alair™ System, is a treatment for severe asthma approved by the FDA in 2010 involving the delivery of controlled, therapeutic radiofrequency energy to the airway wall, thus heating the tissue and reducing the amount of smooth muscle present in the airway wall.[1] This treatment has been shown to result in acute epithelial destruction with regeneration observed in the epithelium, blood vessels, mucosa and nerves. However, airway smooth muscle has demonstrated almost no capacity for regeneration, instead being replaced by connective tissue.[2] The treatment has been shown to be safe and effective over at least five years.[3]
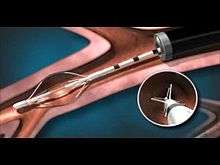
The Procedure
A full course of bronchial thermoplasty treatment[4] includes three separate bronchoscopic procedures: one for the each lower lobe of the lung and another for both upper lobes. Each outpatient procedure is performed approximately three weeks apart.
Under sedation, a catheter inside a bronchoscope—a thin, flexible tube-like instrument introduced through the patient’s nose or mouth, and into their lungs—delivers thermal energy into the airways. The patient is monitored after the procedure and usually returns home that day or early the next day. The catheter delivers a series of 10-second temperature controlled bursts of radio frequency energy which heat the lining of the lungs to 65 degrees Celsius. It is this heat that destroys some of the muscle tissue which constricts during an asthma attack, reducing the number and severity of exacerbations.
Benefits
In a double-blind, randomized, sham-controlled clinical study of bronchial thermoplasty,[5] adults with severe asthma that were treated with bronchial thermoplasty had improved asthma-related quality of life out to a year compared to the control (sham-treated) patients. Additionally, when compared to control patients, patients treated with bronchial thermoplasty also experienced the following significant benefits:
- 32% reduction in asthma attacks
- 84% reduction in emergency room visits for respiratory symptoms
- 66% reduction in days lost from work, school, or other daily activities due to asthma symptoms
- 73% reduction in hospitalizations for respiratory symptoms
Reduction in asthma attacks, ER visits, and hospitalizations for respiratory symptoms are maintained to at least 5 years.[3] These benefits were observed during clinical studies where patients continued to take their standard maintenance asthma medications which included combinations of inhaled corticosteroids and long-acting bronchodilators.
Risks of Procedure
In the period immediately following the bronchial thermoplasty procedure, there was an expected transient increase in the frequency and worsening of respiratory-related symptoms.
Procedure Availability
Bronchial thermoplasty was first approved by FDA in April 2010.[6] and is available at various Hospitals in the United States.[7]
Bronchial thermoplasty is now being used as a treatment in many countries outside of the United States including countries in Europe, South America, Asia, and Australia.[8]
Bronchial thermoplasty is now being used as a treatment in the United Kingdom.[9]
References
- ↑ Cox G., M. D., McWilliams A., FitzGerald J.M., and Lam S. (2006). "Bronchial Thermoplasty for Asthma." American Journal of Respiratory Critical Care Medicine 173: 965 - 969.
- ↑ Mitzner, W. (2006). "Bronchial Thermoplasty in Asthma." Allergology International 55(3): 225 - 234.
- 1 2 "DEFINE_ME_WA". jacionline.org.
- ↑ "Clinical Pearls for Bronchial Thermoplasty : Journal of Bronchology & Interventional Pulmonology". LWW.
- ↑ "An Error Occurred Setting Your User Cookie". atsjournals.org.
- ↑ "Asthmatx, Inc. Alair Bronchial Thermoplasty System - P080032". U.S. Food and Drug Administration. 2010-05-19.
- ↑ "Bronchial Thermoplasty – Find A Clinic". btforasthma.com.
- ↑ "Bronchial Thermoplasty – Find A Clinic". btforasthma.com.
- ↑ Nick Ravenscroft (8 June 2011). "UK doctors begin pioneering asthma treatment". BBC News.