Cerebral circulation
| Cerebral circulation | |
|---|---|
 Ares of the brain are supplied by different arteries. The major systems are divided into an anterior circulation (the anterior cerebral artery and middle cerebral artery) and a posterior circulation | |
 Schematic of veins and venous spaces that drain deoxygenated blood from the brain | |
Cerebral circulation is the movement of blood through the network of blood vessels supplying the brain. The rate of the cerebral blood flow in the adult, is typically 750 milliliters per minute, representing 15% of the cardiac output. The arteries deliver oxygenated blood, glucose and other nutrients to the brain and the veins carry deoxygenated blood back to the heart, removing carbon dioxide, lactic acid, and other metabolic products. Since the brain is very vulnerable to compromises in its blood supply, the cerebral circulatory system has many safeguards. Failure of these safeguards results in cerebrovascular accidents, commonly known as strokes. The amount of blood that the cerebral circulation carries is known as cerebral blood flow. The presence of gravitational fields or accelerations also determine variations in the movement and distribution of blood in the brain, such as when suspended upside-down.
The following description is based on idealized human cerebral circulation. The pattern of circulation and its nomenclature vary between organisms.
Anatomy

Blood supply

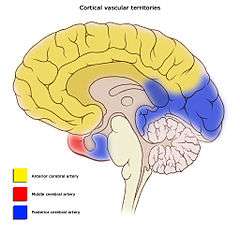
Blood supply to the brain is normally divided into anterior and posterior segments, relating to the different arteries that supply the brain. The two main pairs of arteries are the Internal carotid arteries (supply the anterior brain) and vertebral arteries (supplying the brainstem and posterior brain).
The anterior and posterior cerebral circulations are interconnected via bilateral posterior communicating arteries. They are part of the Circle of Willis, which provides backup circulation to the brain. In case one of the supply arteries is occluded, the Circle of Willis provides interconnections between the anterior and the posterior cerebral circulation along the floor of the cerebral vault, providing blood to tissues that would otherwise become ischemic.
Anterior cerebral circulation
The anterior cerebral circulation is the blood supply to the anterior portion of the brain. It is supplied by the following arteries:
- Internal carotid arteries: These large arteries are the left and right branches of the common carotid arteries in the neck which enter the skull, as opposed to the external carotid branches which supply the facial tissues. The internal carotid artery branches into the anterior cerebral artery and continues to form the middle cerebral artery
- Anterior cerebral artery (ACA)
- Anterior communicating artery: Connects both anterior cerebral arteries, within and along the floor of the cerebral vault.
- Middle cerebral artery (MCA)
Posterior cerebral circulation
The posterior cerebral circulation is the blood supply to the posterior portion of the brain, including the occipital lobes, cerebellum and brainstem. It is supplied by the following arteries:
- Vertebral arteries: These smaller arteries branch from the subclavian arteries which primarily supply the shoulders, lateral chest and arms. Within the cranium the two vertebral arteries fuse into the basilar artery.
- Basilar artery: Supplies the midbrain, cerebellum, and usually branches into the posterior cerebral artery
- Posterior cerebral artery (PCA)
- Posterior communicating artery
-
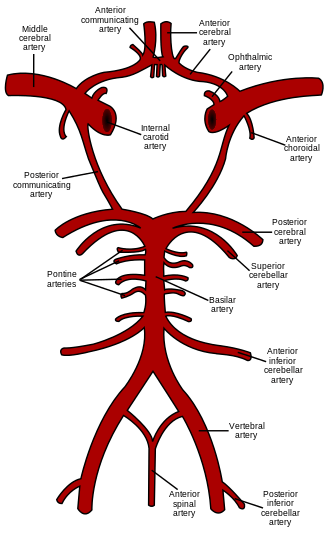
The anterior and posterior circulations meet at the Circle of Willis, pictured here, which rests at the top of the brainstem.
Venous drainage
The venous drainage of the cerebrum can be separated into two subdivisions: superficial and deep.
The superficial system is composed of dural venous sinuses, which have wall composed of dura mater as opposed to a traditional vein. The dural sinuses are, therefore located on the surface of the cerebrum. The most prominent of these sinuses is the superior sagittal sinus which flows in the sagittal plane under the midline of the cerebral vault, posteriorly and inferiorly to the torcula, forming the confluence of sinuses, where the superficial drainage joins with the sinus that primarily drains the deep venous system. From here, two transverse sinuses bifurcate and travel laterally and inferiorly in an S-shaped curve that form the sigmoid sinuses which go on to form the two jugular veins. In the neck, the jugular veins parallel the upward course of the carotid arteries and drain blood into the superior vena cava.
The deep venous drainage is primarily composed of traditional veins inside the deep structures of the brain, which join behind the midbrain to form the vein of Galen. This vein merges with the inferior sagittal sinus to form the straight sinus which then joins the superficial venous system mentioned above at the confluence of sinuses.
Physiology
Cerebral blood flow (CBF) is the blood supply to the brain in a given period of time.[1] In an adult, CBF is typically 750 millilitres per minute or 15% of the cardiac output. This equates to an average perfusion of 50 to 54 millilitres of blood per 100 grams of brain tissue per minute.[2][3][4] CBF is tightly regulated to meet the brain's metabolic demands.[2][5] Too much blood (a condition known as hyperemia) can raise intracranial pressure (ICP), which can compress and damage delicate brain tissue. Too little blood flow (ischemia) results if blood flow to the brain is below 18 to 20 ml per 100 g per minute, and tissue death occurs if flow dips below 8 to 10 ml per 100 g per minute. In brain tissue, a biochemical cascade known as the ischemic cascade is triggered when the tissue becomes ischemic, potentially resulting in damage to and the death of brain cells. Medical professionals must take steps to maintain proper CBF in patients who have conditions like shock, stroke, cerebral edema, and traumatic brain injury.
Cerebral blood flow is determined by a number of factors, such as viscosity of blood, how dilated blood vessels are, and the net pressure of the flow of blood into the brain, known as cerebral perfusion pressure, which is determined by the body's blood pressure. Cerebral blood vessels are able to change the flow of blood through them by altering their diameters in a process called autoregulation; they constrict when systemic blood pressure is raised and dilate when it is lowered.[6] Arterioles also constrict and dilate in response to different chemical concentrations. For example, they dilate in response to higher levels of carbon dioxide in the blood and constrict to lower levels of carbon dioxide.[6]
For example, assuming a person with an arterial partial pressure of carbon dioxide (PaCO2) of 40 mmHg (normal range of 38 - 42 mmHg)[7] and a CBF of 50 ml per 100g per min. If the PaCO2 dips to 30 mmHg, this represents a 10 mmHg decrease from the initial value of PaCO2. Consequently, the CBF decreases by 1ml per 100g per min for each 1mmHg decrease in PaCO2, resulting in a new CBF of 40ml per 100g of brain tissue per minute. In fact, for each 1 mmHg increase or decrease in PaCO2, between the range of 20–60 mmHg, there is a corresponding CBF change in the same direction of approximately 1–2 ml/100g/min, or 2–5% of the CBF value.[8] This is why small alterations in respiration pattern can cause significant changes in global CBF, specially through PaCO2 variations.[8]
CBF is equal to the cerebral perfusion pressure (CPP) divided by the cerebrovascular resistance (CVR):[9]
- CBF = CPP / CVR
Control of CBF is considered in terms of the factors affecting CPP and the factors affecting CVR. CVR is controlled by four major mechanisms:
- Metabolic control (or 'metabolic autoregulation')
- Pressure autoregulation
- Chemical control (by arterial pCO2 and pO2)
- Neural control
Role of intracranial pressure
Increased intracranial pressure (ICP) causes decreased blood perfusion of brain cells by mainly two mechanisms:
- Increased ICP constitutes an increased interstitial hydrostatic pressure that, in turn, causes a decreased driving force for capillary filtration from intracerebral blood vessels.
- Increased ICP compresses cerebral arteries, causing increased cerebrovascular resistance (CVR).
Cerebral perfusion pressure
Cerebral perfusion pressure, or CPP, is the net pressure gradient causing cerebral blood flow to the brain (brain perfusion). It must be maintained within narrow limits because too little pressure could cause brain tissue to become ischemic (having inadequate blood flow), and too much could raise intracranial pressure (ICP).
Imaging
Functional magnetic resonance imaging and positron emission tomography are neuroimaging techniques that can be used to measure CBF. These techniques are also used to measure regional CBF (rCBF) within a specific brain region. rCBF at one location can be measured over time by thermal diffusion[10]
References
- ↑ Tolias C and Sgouros S. 2006. "Initial Evaluation and Management of CNS Injury." Archived March 2, 2007, at the Wayback Machine. Emedicine.com. Accessed January 4, 2007.
- 1 2 Orlando Regional Healthcare, Education and Development. 2004. "Overview of Adult Traumatic Brain Injuries." Archived February 27, 2008, at the Wayback Machine. Accessed 2008-01-16.
- ↑ Shepherd S. 2004. "Head Trauma." Emedicine.com. Shepherd S. 2004. "Head Trauma." Emedicine.com. Accessed January 4, 2007.
- ↑ Walters, FJM. 1998. "Intracranial Pressure and Cerebral Blood Flow." Archived May 14, 2011, at the Wayback Machine. Physiology. Issue 8, Article 4. Accessed January 4, 2007.
- ↑ Singh J and Stock A. 2006. "Head Trauma." Emedicine.com. Accessed January 4, 2007.
- 1 2 Kandel E.R., Schwartz, J.H., Jessell, T.M. 2000. Principles of Neural Science, 4th ed., McGraw-Hill, New York. p.1305
- ↑ Hadjiliadis D, Zieve D, Ogilvie I. Blood Gases. Medline Plus. 06/06/2015.
- 1 2 Giardino ND, Friedman SD, Dager SR. Anxiety, respiration, and cerebral blood flow: implications for functional brain imaging. Compr Psychiatry 2007;48:103–112. Accessed 6/6/2015.
- ↑ AnaesthesiaUK. 2007. Cerebral Blood Flow (CBF) Archived September 18, 2010, at the Wayback Machine.. Accessed 2007-10-16.
- ↑ P. Vajkoczy, H. Roth, P. Horn, T. Lucke, C. Thome, U. Hubner, G. T. Martin, C. Zappletal, E. Klar, L. Schilling, and P. Schmiedek, “Continuous monitoring of regional cerebral blood flow: experimental and clinical validation of a novel thermal diffusion microprobe,” J. Neurosurg., vol. 93, no. 2, pp. 265–274, Aug. 2000.