Elderly care
Elderly care, or simply eldercare (also known in parts of the English speaking world as aged care), is the fulfillment of the special needs and requirements that are unique to senior citizens. This broad term encompasses such services as assisted living, adult day care, long term care, nursing homes (often referred to as residential care), hospice care, and home care. Because of the wide variety of elderly care found nationally, as well as differentiating cultural perspectives on elderly citizens, cannot to be limited to any one practice. For example, many countries in Asia use government-established elderly care quite infrequently, preferring the traditional methods of being cared for by younger generations of family members.
Elderly care emphasizes the social and personal requirements of senior citizens who need some assistance with daily activities and health care, but who desire to age with dignity. It is an important distinction, in that the design of housing, services, activities, employee training and such should be truly customer-centered. It is also noteworthy that a large amount of global elderly care falls under the unpaid market sector.[1]
Cultural and geographic differences
The form of elderly care provided varies greatly among countries and is changing rapidly.[2] Even within the same country, regional differences exist with respect to the care for the elderly.[3] However, it has been observed that the global elderly consume the most health expenditures out of any other age group,[4] observation that shows comprehensive eldercare may be very similar. One must also account for an increasingly large proportion of global elderly, especially in developing nations, as continued pressure is put on limiting fertility and decreasing family size.[5]
Traditionally, elderly care has been the responsibility of family members and was provided within the extended family home.[6] Increasingly in modern societies, elderly care is now being provided by state or charitable institutions.[6] The reasons for this change include decreasing family size, the greater life expectancy of elderly people, the geographical dispersion of families, and the tendency for women to be educated and work outside the home.[6] Although these changes have affected European and North American countries first, they are now increasingly affecting Asian countries as well.[7]
In most western countries, elderly care facilities are residential family care homes, freestanding assisted living facilities, nursing homes, and Continuing care retirement communities (CCRCs).[8] A family care home is a residential home with support and supervisory personnel by an agency, organization, or individual that provides room and board, personal care and habilitation services in a family environment for at least two and no more than six persons.[9]
Gender discrepancies in caregivers
According to Family Caregiver Alliance, the majority of family caregivers are women:[10]
“Many studies have looked at the role of women and family caregiving. Although not all have addressed gender issues and caregiving specifically, the results are still generalizable [sic] to
- Estimates of the age of family or informal caregivers who are women range from 59% to 75%.
- The average caregiver is age 46, female, married and worked outside the home earning an annual income of $35,000.
- Although men also provide assistance, female caregivers may spend as much as 50% more time providing care than male caregivers."[10]
In developed nations
United States
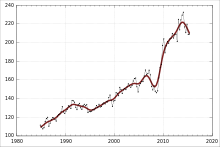
According to the United States Department of Health and Human Services the older population—persons 65 years or older—numbered 39.6 million in 2009.[11] They represented 12.9% of the U.S. population, about one in every eight Americans.[11] By 2030, there will be about 72.1 million older persons, more than twice their number in 2000.[11] People 65-plus years old represented 12.4% of the population in the year 2000, but that is expected to grow to be 19% of the population by 2030.[11] This will mean more demand for elderly care facilities in the coming years. There were more than 36,000 assisted living facilities in the United States in 2009, according to the Assisted Living Federation of America [12] in 2009. More than 1 million senior citizens are served by these assisted living facilities.[12]
Last-year-of-life expenses represent 22% of all medical spending in the United States, 26% of all Medicare spending, 18% of all non-Medicare spending, and 25 percent of all Medicaid spending for the poor.[13]
In the United States, most of the large multi-facility providers are publicly owned and managed as for-profit businesses.[10] There are exceptions; the largest operator in the US is the Evangelical Lutheran Good Samaritan Society, a not-for-profit organization that manages 6,531 beds in 22 states, according to a 1995 study by the American Health Care Association.[14]
Given the choice, most elders would prefer to continue to live in their homes (aging in place).[15] Many elderly people gradually lose functioning ability and require either additional assistance in the home or a move to an eldercare facility.[15] The adult children of these elders often face a difficult challenge in helping their parents make the right choices.[16] Assisted living is one option for the elderly who need assistance with everyday tasks. It costs less than nursing home care but is still considered expensive for most people.[17] Home care services may allow seniors to live in their own home for a longer period of time.
One relatively new service in the United States that can help keep the elderly in their homes longer is respite care.[18] This type of care allows caregivers the opportunity to go on vacation or a business trip and know that their elder has good quality temporary care, for without this help the elder might have to move permanently to an outside facility. Another unique type of care cropping in U.S. hospitals is called acute care of elder units, or ACE units, which provide "a homelike setting" within a medical center specifically for the elderly.[19]
Information about long-term care options in the United States can be found by contacting the local Area Agency on Aging[20] or elder referral agencies such as Silver Living, or A Place for Mom. Furthermore, the U.S. government recommends evaluation of health care facilities through websites using data collected from sources such as Medicare records.[21]
Canada
In Canada, such privately run for-profit and not-for-profit facilities also exist. Because of cost factors, some provinces operate government-funded public facilities run by each province's or territory's Ministry of Health, or the government may subsidize the cost of the facility. In these care homes, elderly Canadians may pay for their care on a sliding scale based on annual income. The scale that they are charged on depends on whether they are considered “Long Term Care” or “Assisted Living.” For example, commencing in January 2010 seniors living in British Columbia’s government subsidized “Long Term Care” (also called “Residential Care”) will pay 80% of their after-tax income unless their After Tax Income is less than $16,500. The “Assisted Living” tariff is calculated more simply as 70% of the After-Tax Income.[22]
Australia
Aged care in Australia is designed to make sure that every Australian can contribute as much as possible toward their cost of care, depending on their individual income and assets.[23] This means that residents pay only what they can afford, and the Commonwealth government pays what a resident cannot. An Australian statutory authority, the Productivity Commission, conducted a review of aged care commencing in 2010 and reporting in 2011. That review concluded that approximately 80% of care for older Australians is informal care provided by family, friends and neighbours. Around a million people received government-subsidised aged care services, most of these receiving low-level community care support, with 160 000 people in permanent residential care. Expenditure on aged care by all governments in 2009-10 was approximately $11 billion.[24]
The need for increasing amounts of care, and known weaknesses in the care system (such as skilled workforce shortages and rationing of available care places), led several reviews in the 2000s to conclude that Australia's aged care system needs reform. This culminated in the 2011 Productivity Commission report and subsequent reform proposals.[25] In accordance with the Living Longer, Living Better amendments of 2013, assistance is provided in accordance with assessed care needs, with additional supplements available for people experiencing homelessness, dementia and veterans.[26]
Australian Aged Care is often considered complicated due to various state and federal funding. Furthermore, there are many acronyms that customers need to be aware of, including ACAT, ACAR, NRCP, HACC, CACP, EACH, EACH-D and CDC (Consumer Directed Care) to name a few.[25]
England
Care for the elderly in England is increasingly rationed according to a joint report by the King's Fund and Nuffield Trust. People are left to struggle without support on their own. Larger numbers of old people need help due to an aging population but less is being paid out to help them. A million people who need care get neither formal nor informal help.[27]
In developing nations
Nepal
Due to health and economic benefits, the life expectancy in Nepal jumped from 27 years in 1951 to 65 in 2008.[28] Most elderly Nepali citizens, roughly 85%, live in rural areas.[28] Because of this, there is a significant lack of government sponsored programs or homes for the elderly. Traditionally, parents live with their children, and today, it is estimated that 90% of the elderly do live in the homes of their family.[28] This number is changing as more children leave home for work or school, leading to loneliness and mental problems in Nepali elderly.[28]
The Ninth Five-Year Plan included policies in an attempt to care for the elderly left without children as caretakers.[28] A Senior Health Facilities Fund has been established in each district.[28] The Senior Citizens Health Facilities Program Implementation Guideline, 2061BS provides medical facilities to the elderly, and to those that are poverty stricken, free medicine and health care in all districts.[28] In its yearly budget, the government has planned to fund free health care to all heart and kidney patients older than 75.[28] Unfortunately, many of these plans are overly ambitious, which has been recognized by the Nepali government.[28] Nepal is a developing nation and may not be able to fund all of these programs after the development of an Old Age Allowance, or OAA. OAA provides a monthly stipend to all citizens over 70 and widows over 60.[28]
There are a handful of private day care facilities for elderly, but it is limited to the capital city. These day care services are very expensive and out of reach for the general public.
Thailand
Thailand has observed global patterns of an enlarging elderly class: as fertility control is encouraged and medical advances are made, births shrink and lives age.[5] The Thai government is noticing and concerned about this trend, but tends to let families care for their elderly members rather than create extraneous policies for them.[29] As of 2011, there are only 25 state sponsored homes for the elderly, with no more than a few thousand members of each home.[29] Such programs are largely run by volunteers and are questionable by quality of care, considering there is not always a guarantee care will be available. Private care is tough to follow, often based on assumptions. Because children are less likely to care for their parents, private caretakers are in demand.[29] Volunteer NGOs are available but in very limited quantities.[29]
While there are certainly programs available for use by the elderly in Thailand, questions of equity have risen since their introduction.[30] The rich elderly in Thailand are much more likely to have access to care resources, while the poor elderly are more likely to actually use their acquired health care, as observed in a study by Bhumisuk Khananurak.[30] However, over 96% of the nation has health insurance with varying degrees of care available.[30]
India
India's cultural view of elderly care is similar to that of Nepal's. Parents are typically cared for by their children into old age, most commonly by their sons.[31] It should be noted that in these countries, elderly citizens, especially men, are viewed in very high regard. Traditional values demand honor and respect for older, wiser people.[32] India is facing the same problem as many developing nations in that its elderly population is increasing tremendously, with a current estimate of 90 million over the age of 60.[33] Using data on health and living conditions from the India's 60th National Sample Survey, a study found that almost a quarter of the elderly reported poor health. Reports of poor health were clustered among the poor, single, lower-educated and economically inactive groups.[34]
Under its eleventh Five-Year plan, the Indian government has made many strides similar to that of Nepal. Article 41 of the Indian Constitution states that elderly citizens will be guaranteed Social Security support for health care and welfare.[33] A section of the 1973 Criminal Procedure Code, alluding to its traditional background, mandates that children support their parents if they no longer can themselves.[33] NGOs, however, are prevalent in Indian elderly care, providing homes and volunteer care, but governmental policies and organizations are accessible.[33]
Medical (skilled care) versus non-medical (social care)
A distinction is generally made between medical and non-medical care, care provided by people who are not medical professionals. The latter is much less likely to be covered by insurance or public funds. In the US, 67% of the one million or so residents in assisted living facilities pay for care out of their own funds.[35] The rest get help from family and friends and from state agencies. Medicare does not pay unless skilled-nursing care is needed and given in certified skilled nursing facilities or by a skilled nursing agency in the home. Assisted living facilities usually do not meet Medicare's requirements. However, Medicare does pay for some skilled care if the elderly person meets the requirements for the Medicare home health benefit. [36]
Thirty-two U.S. states pay for care in assisted living facilities through their Medicaid waiver programs. Similarly, in the United Kingdom the National Health Service provides medical care for the elderly, as for all, free at the point of use, but social care is only paid for by the state in Scotland; England, Wales and Northern Ireland are yet to introduce any legislation on the matter, so currently social care is only funded by public authorities when a person has exhausted their private resources, for example, by selling their home. Money provided for supporting elderly people in the UK has fallen by 20% per person during the ten years from 2005 to 2015 and in real terms the fall was greater. Experts claim that vulnerable UK people do not get what they need.[37]
However, elderly care is focused on satisfying the expectations of two tiers of customers: the resident customer and the purchasing customer, who are often not identical, since relatives or public authorities rather than the resident may be providing the cost of care. Where residents are confused or have communication difficulties, it may be very difficult for relatives or other concerned parties to be sure of the standard of care being given, and the possibility of elder abuse is a continuing source of concern. The Adult Protective Services Agency — a component of the human service agency in most states — is typically responsible for investigating reports of domestic elder abuse and providing families with help and guidance. Other professionals who may be able to help include doctors or nurses, police officers, lawyers, and social workers.[38]
Promoting independence
Promoting independence in self-care can provide older adults with the capability to maintain independence longer and can leave them with a sense of achievement when they complete a task unaided. Older adults that require assistance with activities of daily living are at a greater risk of losing their independence with self-care tasks as dependent personal behaviours are often met with reinforcement from caregivers.[39] It is important for caregivers to ensure that measures are put into place to preserve and promote function rather than contribute to a decline in status in an older adult that has physical limitations. Caregivers need to be conscious of actions and behaviors that cause older adults to become dependent on them and need to allow older patients to maintain as much independence as possible. Providing information to the older patient on why it is important to perform self-care may allow them to see the benefit in performing self-care independently. If the older adult is able to complete self-care activities on their own, or even if they need supervision, encourage them in their efforts as maintaining independence can provide them with a sense of accomplishment and the ability to maintain independence longer.[40]
Improving mobility
Impaired mobility is a major health concern for older adults, affecting 50% of people over 85 and at least a quarter of those over 75. As adults lose the ability to walk, to climb stairs, and to rise from a chair, they become completely disabled. The problem cannot be ignored because people over 65 constitute the fastest growing segment of the U.S. population.
Therapy designed to improve mobility in elderly patients is usually built around diagnosing and treating specific impairments, such as reduced strength or poor balance. It is appropriate to compare older adults seeking to improve their mobility to athletes seeking to improve their split times. People in both groups perform best when they measure their progress and work toward specific goals related to strength, aerobic capacity, and other physical qualities. Someone attempting to improve an older adult’s mobility must decide what impairments to focus on, and in many cases, there is little scientific evidence to justify any of the options. Today, many caregivers choose to focus on leg strength and balance. New research suggests that limb velocity and core strength may also be important factors in mobility.[41]
The family is one of the most important providers for the elderly. In fact, the majority of caregivers for the elderly are often members of their own family, most often a daughter or a granddaughter. Family and friends can provide a home (i.e. have elderly relatives live with them), help with money and meet social needs by visiting, taking them out on trips, etc.
One of the major causes of elderly falls is hyponatremia, an electrolyte disturbance when the level of sodium in a person's serum drops below 135 mEq/L. Hyponatremia is the most common electrolyte disorder encountered in the elderly patient population. Studies have shown that older patients are more prone to hyponatremia as a result of multiple factors including physiologic changes associated with aging such as decreases in glomerular filtration rate, a tendency for defective sodium conservation, and increased vasopressin activity. Mild hyponatremia ups the risk of fracture in elderly patients because hyponatremia has been shown to cause subtle neurologic impairment that affects gait and attention, similar to that of moderate alcohol intake.[42]
Legal issues about incapacity
Legal incapacity is an invasive and sometimes, difficult legal procedure. It requires that a person file a petition with the local courts, stating the elderly person lacks the capacity to carry out activities that include making medical decisions, voting, making gifts, seeking public benefits, marrying, managing property and financial affairs, choosing where to live and who they socialize with. Most states' laws require that a minimum of two doctors or other health professionals, provide reports as evidence of such incompetence and the person must be represented by an attorney. Only then can the individual's legal rights be removed and legal supervision by a guardian or conservator be initiated. The legal guardian or conservator is the person to whom the court delegates the responsibility of acting on the incapacitated person's behalf and must report regularly his or her activities to the court.
A less restrictive alternative to legal incapacity is the use of "Advance Directives"; powers of attorney, trusts, living wills and health care directives. The person who has these documents in place, should have prepared them with their attorney when that person had capacity. So, if the time comes when that person lacks capacity to carry out those tasks laid out in the documents, the person they named (their agent) can step in to make decisions on their behalf. The agent has a duty to act as that person would have and in their best interest.
See also
- Food preferences in older adults and seniors
- Gerontology
- Home automation for the elderly and disabled
- Transgenerational design
References
![]() This article incorporates public domain material from the United States Government document "A Profile of Older Americans: 2010, Department of Health & Human Services".
This article incorporates public domain material from the United States Government document "A Profile of Older Americans: 2010, Department of Health & Human Services".
- ↑ Kijong Kim; Rania Antonopoulos (2011). Unpaid and Paid Care: The Effects of Child Care and Elder Care on the Standard of Living (PDF). Levy Economics Institute.
- ↑ Sundström, Gerdt (1982). "The Elderly, Women's Work and Social Security Costs". Acta Sociologica. 25 (1): 21–38. doi:10.1177/000169938202500102. JSTOR 4194376.
- ↑ A Senior Companion, LLC 2009. aseniorcompanionllc.com
- ↑ "Health and Elderly Care Expenditure in an Aging World," 2000
- 1 2 World Population Aging: "World Population Aging, 2010"
- 1 2 3 Elder Care: "Elder care: is legislation of family responsibility the solution?" Ting et al. 2009
- ↑ Huang, Shirlena; Thang, Leng Leng; Toyota, Mika (2012). "Transnational mobilities for care: Rethinking the dynamics of care in Asia". Global Networks. 12 (2): 129. doi:10.1111/j.1471-0374.2012.00343.x.
- ↑ Kane, Robert L. (1986). "Medical Care for the Elderly in Other Western Countries". Home Health Care Services Quarterly. 7 (3–4): 307. doi:10.1300/J027v07n03_37.
- ↑ "Family Care Homes," Piedmont Triad Council of Governments
- 1 2 3 FCA: Family Caregiver Alliance
- 1 2 3 4 Aging Statistics, U.S Department of Health and Human Services, June 2010
- 1 2 ALFA: Assisted Living Federation of America
- ↑ Donald R Hoover; Stephen Crystal; Rizie Kumar; Usha Sambamoorthi; Joel C Cantor (December 1, 2002). "Medical Expenditures during the Last Year of Life: Findings from the 1992–1996 Medicare Current Beneficiary Survey". Health Service Research. 37 (6): 1625–1642. doi:10.1111/1475-6773.01113. PMC 1464043
 . PMID 12546289.
. PMID 12546289. Last-year-of-life expenses constituted 22 percent of all medical, 26 percent of Medicare, 18 percent of all non-Medicare expenditures, and 25 percent of Medicaid expenditures.
- ↑ The Moran Company (December 2011). "Assessing the Financial Implications of Alternative Reimbursement Policies for Nursing Facilities" (PDF). American Health Care Association.
- 1 2 "What Is Aging In Place?". AgeInPlace.com.
- ↑ Gross, Jane (July 2008). "Faced with Caregiving, Even the Experts Struggle". New York Times. Retrieved 2008-07-26.
- ↑ "Assisted Living". MedLine Plus. Retrieved 26 September 2012.
- ↑ "Caregivers Catch a Break with Respite Care". BestAssistedLiving.com. September 2008. Retrieved 2008-10-01.
- ↑ Acute Care for Elders Project, 2011
- ↑ Area Agency on Aging Retrieved 15 May 2013.
- ↑ "Tips for Choosing a Health Care Facility". USA.gov. Retrieved 26 September 2012.
- ↑ Elder Care BC, "Assisted Living Vs Long Term Care", ElderCareBC.com
- ↑ "Aged care Australia". Department of Health and Ageing. Archived from the original on May 13, 2013.
- ↑ Productivity Commission (2011). Caring for Older Australians: Overview (PDF). Canberra: Productivity Commission.
- 1 2 Bethanie. "Aged Care Glossarys". Bethanie. Retrieved 16 August 2013.
- ↑ Government, Australia. "Living Longer, Living Better - legislative changes". Department of Health and Ageing. Australian Government. Retrieved 12 July 2013.
- ↑ Care for elderly 'increasingly rationed' in England BBC
- 1 2 3 4 5 6 7 8 9 10 "Status Report on Elderly People in Nepal," Geriatric Center Nepal, 2010
- 1 2 3 4 Thailand: Intergenerational Family Care for and by Older People in Thailand, 2011
- 1 2 3 Khananurak, Bhumisuk (2009) Health Equity in Thai Ageing
- ↑ Desai, Sonalde, Amaresh Dubey, B.L. Joshi, Mitali Sen, Abusaleh Shariff and Reeve Vanneman (2010). India Human Development in India: Challenges for a Society in Transition. New Delhi: Oxford University Press. ISBN 0198065124.
- ↑ Sivamurthy, M. and Wadakannavar, A.R. (2001) Care and support for the elderly population in India: Results of a survey rural North Karnataka (India)
- 1 2 3 4 HelpAge: HelpAge India, 2009
- ↑ Sumit, Mazumdar; Ulf-Goran Gerdtham (13 September 2011). "Heterogeneity in Self-Assessed Health Status Among the Elderly in India". Asia-Pacific Journal of Public Health. 25 (3): 271–83. doi:10.1177/1010539511416109. PMID 21914712. Retrieved 18 May 2012.
- ↑ AARP Assisted Living in the US, 2000
- ↑ "How to Pay for Senior Care". VidaSeniorResource.com. August 2008. Retrieved 2009-03-30.
- ↑ Care spend 'cut by fifth in decade'
- ↑ Meyer, Maria M. and Derr, Paul (December 2008) "What to Do When You Suspect Elder Abuse," Caring.com, Senior Care and Elder Care
- ↑ Barton, E. M.; Baltes, M. M. & Orzech, M. J. (1980). "Etiology of dependence in older nursing home residents during morning care: The role of staff behavior". Journal of Personality and Social Psychology. 38 (3): 423–431. doi:10.1037/0022-3514.38.3.423. PMID 7373517.
- ↑ Secker, J.; Hill, R.; Villeneau, L. & Parkman, S. (2003). "Promoting independence: But promoting what and how?". Ageing and Society. 23 (3): 375–391<. doi:10.1017/S0144686X03001193.
- ↑ Bean, Jonathan. "Three Big Risks For Older Adults: Walking, Climbing Stairs and Rising from a Chair - Evidence-based Rehabilitative Care for Older Adults." CIMIT Forum. November 6, 2007.
- ↑ Sandhu, HS; Gilles, E; Devita, MV; Panagopoulos, G; Michelis, MF (2009). "Hyponatremia associated with large-bone fracture in elderly patients". International urology and nephrology. 41 (3): 733–7. doi:10.1007/s11255-009-9585-2. PMID 19472069.
Further reading
- Eliminating Barriers to Mental Health Treatment: A Guide for Massachusetts Elders, Families and Caregivers", Massachusetts Association of Older Americans, 3rd Edition, 2008.
- Vieillissement et enjeux d'aménagement: regards à différentes échelles (ed. by Paula Negron-Poblete and Anne-Marie Séguin), Presses de l'Université du Québec, 2012. ISBN 978-2-7605-3428-5