Epidemiological transition

In demography and medical geography, epidemiological transition is a phase of development witnessed by a sudden and stark increase in population growth rates brought about by medical innovation in disease or sickness therapy and treatment, followed by a re-leveling of population growth from subsequent declines in fertility rates. "Epidemiological transition" accounts for the replacement of infectious diseases by chronic diseases over time due to expanded public health and sanitation.[1][2] This theory was originally posited by Abdel Omran in 1971.[3]
Theory
Omran divided the epidemiological transition of mortality into three phases, in the last of which chronic diseases replace infection as the primary cause of death.[4] These phases are:
- The Age of Pestilence and Famine: Where mortality is high and fluctuating, precluding sustained population growth, with low and variable life expectancy, vacillating between 20 and 40 years.
- The Age of Receding Pandemics: Where mortality progressively declines, with the rate of decline accelerating as epidemic peaks decrease in frequency. Average life expectancy increases steadily from about 30 to 50 years. Population growth is sustained and begins to be exponential.
- The Age of Degenerative and Man-Made Diseases: Mortality continues to decline and eventually approaches stability at a relatively low level.
The epidemiological transition occurs as a country undergoes the process of modernization from developing nation to developed nation status. The developments of modern healthcare, and medicine like antibiotics, drastically reduces infant mortality rates and extends average life expectancy which, coupled with subsequent declines in fertility rates, reflects a transition to chronic and degenerative diseases which were more important causes of death.
History
In general human history, Omran's first phase occurs when human population sustains cyclic, low-growth, and mostly linear, up-and-down patterns associated with wars, famine, epidemic outbreaks, as well as small golden ages, and localized periods of "prosperity". In early pre-agricultural history, infant mortality rates were high and average life expectancy low. Today, life expectancy in third world countries remains relatively low, as in many Sub-Saharan African nations where it typically doesn't exceed 60 years of age.[5]
The second phase involves advancements in medicine and the development of a healthcare system. Half of the deaths prevented during the 19th century may be due to clean water provided by public utilities with a particular benefit for children.[6][7] One treatment breakthrough of note was the discovery of penicillin in the mid 20th century which led to widespread and dramatic declines in death rates from previously serious diseases such as syphilis. Population growth rates surged in the 1950s, 1960s and 1970s, to 1.8% per year and higher, with the world gaining 2 billion people between 1950 and the 1980s alone.
Omran's third phase occurs when human birth rates drastically decline from highly positive replacement numbers to stable replacement rates. In several European nations replacement rates have even become negative.[8] As this transition generally represents the net effect of individual choices on family size (and the ability to implement those choices), it is more complicated. Omran gives three possible factors tending to encourage reduced fertility rates:[3]
- Bio-physiologic factors, associated with reduced infant mortality and the expectation of longer life in parents;
- Socioeconomic factors, associated with childhood survival and the economic perceptions of large family size; and
- Psychologic or emotional factors, where society as a whole changes its rationale and opinion on family size and parental energies are redirected to qualitative aspects of child-raising.
This transition may also be associated with the sociological adaptations associated with demographic movements to urban areas, and a shift from agriculture and labor based production output to technological and service-sector-based economies.
Regardless, Chronic and degenerative diseases, and accidents and injuries, became more important causes of death. This shift in demographic and disease profiles is currently under way in most developing nations, however every country is unique in its transition speed based on a myriad of geographical and socio-political factors.
Models of transition
Omran developed three models to explain the epidemiological transition.[9]
- Classical/Western model (England, Wales, and Sweden)
- Accelerated model (Japan)
- Contemporary/Delayed model (Chile, Ceylon)
Determinants of disease
- Ecobiological
- Socioeconomic
- Medical/Public health
Other Perspectives
McMichael, Preston, and Murray offer a more nuanced view of the epidemiological transition, highlighting macro trends and emphasizing that there is a change from infectious to non-communicable disease, but arguing that it happens differently in different contexts.
One of the first to refine the idea of the epidemiological transition was Preston, who in 1976 proposed the first comprehensive statistical model relating mortality and cause-specific mortality. Preston used life tables from 43 national populations, including both developed countries such as United States and England and developing countries such as Chile, Colombia, Costa Rica, Guatemala, México, Panama, Taiwan, Trinidad and Tobago, and Venezuela. He used multiple linear regression to analyze the cause-specific-age-standardized death rates by sex. The estimated slopes represented the proportional contribution of each cause to a unit change in the total mortality rate. With the exception of neoplasms in both sexes and cardiovascular disease in males, all of the estimated slopes were positive and statistically significant. This demonstrated that the mortality rates of each from each specific cause were expected to decline as total mortality declined. The major causes accounting for the decline were all infectious and parasitic diseases.[10]
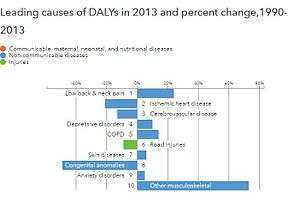
McMichael et al argue (2004) that the epidemiological transition has not taken place homogeneously in all countries. Countries have varied in the speed with which they go through the transition as well as what stage of the transition they are in. The global burden of disease website provides visual comparisons of the disease burdens of countries and the changes over time. The epidemiological transition correlates with changes in life expectancy. Worldwide, mortality rates have decreased as both technological and medical advancements have led to a tremendous decrease in infectious diseases. With fewer people dying from infectious diseases, there is a rising prevalence of chronic and/or degenerative diseases in the older surviving population.
McMichael et al describe life expectancy trends as grouped into three categories as suggested by Casselli et al:
1. Rapid gains – among countries such as Chile, Mexico and Tunisia that have achieved rapid gains converging on developed countries (forexample, Chile)
2. Slower plateauing gains – mostly among developed countries such as France with slower increases in life expectancy (for example, France)
3. Frank reversals – occurring mostly in developing countries such as Zimbabwe and Botswana where the HIV epidemic led to significant decline in life expectancy and countries in the former Soviet union from social upheavals, heaving alcohol consumption and institutional inadequacy (forexample, Zimbabwe) [11]

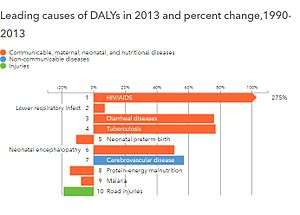
Murray and Lopez (1996) offered one of the most important cause-of-death models as part of the 1990 Global Burden of Disease Study. Their “cause of death” patterns sought to describe the fraction of deaths attributed to a set of mutually exclusive and collectively exhaustive causes. They divided diseases into three cause groups: 1) communicable, maternal, perinatal, and nutritional; 2) non-communicable disease; and 3) injuries. Murray and Lopez made several important observations:
- Group 1 causes of death decline much faster than overall mortality and comprise a small fraction of deaths in wealthier countries.
- Group 2 causes of death are a major challenge for countries that have completed or nearly completed the epidemiologic transition..
- Group 3 causes of death are most variable within and across different countries and are less predictive of all-cause mortality.
The regression approach underlying the Global Burden of Disease received some critique in light of real-world violations of the model’s “mutually exclusive and collectively exhaustive” cause attribution.[12]
Building on the existing body of evidence, Salomon and Murray (2002), further add nuances to the traditional theory of epidemiologic transition by disaggregating it based on disease categories and different age-sex groups, positing that the epidemiologic transition entails a real transition in the cause composition of age-specific mortality, as opposed to just a transition in the age structure. Using Global Burden of Disease data from 1990, they disaggregate the transition across three cause groups: communicable diseases, non-communicable diseases and injuries, seeking to explain the variation in all-cause mortality as a function of cause-specific mortality in 58 countries from 1950 to 1998. This analysis validates the underlying premise of the classic epidemiologic transition theory: as total mortality declines and income rises, communicable diseases cause less and less mortality compared to non-communicable diseases and injuries. Decomposing this overall impact by age-sex groups, they find that for males, when overall mortality decreases, the importance of non-communicable diseases (NCDs) increases relative to the other causes with an age-specific impact on the role of injuries, whereas for women, both NCDs and injuries gain a more significant share with mortality decreases. For children over one year, they find that there is a gradual transition from communicable to non-communicable diseases, with injuries remaining significant in males. For young adults, the epidemiologic transition is particularly different: for males, there is a shift from injuries to NCDs in lower income settings, and the opposite in higher-income settings; for females, rising income also signifies a shift from NCDs to injuries, but the role of injuries becomes more significant over time compared to males. Finally, for both males and females over 50, there is no epidemiologic transition impact on the cause composition of mortality.[12]
Current Evidence

The majority of the literature on the epidemiological transition that was published since these seminal papers confirms the context-specific nature of the epidemiologic transition: while there is an overall all-cause mortality decline, the nature of cause-specific mortality declines differs across contexts. Increasing obesity rates in high-income countries are further confirming the epidemiological transition theory as the epidemic leads to an increase in NCDs. The picture is more nuanced in low- and middle-income countries, where there are signs of a protracted transition with the double burden of communicable and noncommunicable disease. A recent review of cause-specific mortality rates from 12 low- and middle-income countries in Asia and sub-Saharan Africa by Santosa and Byass (2016) shows that broadly, low- and middle-income countries are rapidly transitioning to lower total mortality and lower infectious disease mortality.[12] A more macro-level analysis from the Global Burden of Disease data conducted by Murray and others (2015) finds that while there is a global trend towards decreasing mortality and increasing NCD prevalence, this global trend is being driven by country-specific effects as opposed to a broader transition; further, there are varying patterns within and between countries, which makes it difficult to have a single unified theory of epidemiological transition. [13]
See also
Further reading
- Caselli, Graziella; Mesle, France; Vallin, Jacques (2002), "Epidemiologic transition theory exceptions" (PDF), Genus: Journal of Population Sciences, 9: 9–51, retrieved 3 June 2010
- Fetter, Bruce; Coelho, Phillip R. P.; Rogers, John; Nelson, Marie C. (1997), "Forum: The Epidemiological Transition", Forum: The Health Transition Review, Health Transition Centre, National Centre for Epidemiology and Population Health, The Australian National University, 7, archived from the original (PDF) on March 2004, retrieved 3 June 2010. Contains three articles by four authors.
- Gribble, James N., & Preston, Samuel H (editors) (1993), The Epidemiological Transition: Policy and Planning Implications for Developing Countries, Washington, DC: National Academy Press, ISBN 0-309-04839-7, retrieved 3 June 2010
- Xiaoyan Lei; Nina Yin; Yaohui Zhao (April 2010), SES Health Gradients During the Epidemiological Transition: The Case of China (PDF), Discussion paper No. 4914, retrieved 3 June 2010
- C. G. N. Mascie-Taylor, Jean Peters, Stephen T. McGarvey (editors) (2004), The changing face of disease: implications for society, Florida: CRC Press, ISBN 0-415-32280-4, retrieved 3 June 2010
- McMichael, Anthony J; McKee, Martin; Shkolnikov, Vladimir; Valkonen, Tapani (2004), "Mortality trends and setbacks: Global convergence or divergence?" (PDF), Lancet, 363: 1155–59, doi:10.1016/s0140-6736(04)15902-3, retrieved 3 June 2010
- Mercer, Alexander (2014), Infections, Chronic Disease, and the Epidemiological Transition. A New Perspective. Rochester, NY: University of Rochester Press/Rochester Studies in Medical History, ISBN 978-1-58046-508-3
Notes
- ↑ Mauck, Aaron Pascal. "Managing Care: History of Diabetes in the Twentieth Century". UMI Dissertations. Retrieved 2013-05-05.
- ↑ Miquel Porta (2014) "A dictionary of epidemiology", 6th edn, New York: Oxford University Press. ISBN 9780199976737.
- 1 2 Omran, A.R (2005. First published 1971), "The epidemiological transition: A theory of the epidemiology of population change" (PDF), The Milbank Quarterly, 83 (4): 731–57, doi:10.1111/j.1468-0009.2005.00398.x Check date values in:
|date=(help). Reprinted from The Milbank Memorial Fund Quarterly 49 (No.4, Pt.1), 1971, pp.509–538 - ↑ Corruccini, Robert S. & Kaul, Samvit S (1983), "The epidemiological transition and the anthropology of minor chronic non-infectious diseases", Medical Anthropology, 7: 36–50, doi:10.1080/01459740.1983.9987039
- ↑ CIA - The World Factbook -- Rank Order - Life expectancy at birth
- ↑ The Effect of Infrastructure on Water-Related Diseases in Rural African Communities
- ↑ Cutler, D; Miller, G (February 2005). "The role of public health improvements in health advances: the twentieth-century United States.". Demography. 42 (1): 1–22. doi:10.1353/dem.2005.0002. PMID 15782893.
- ↑ Negative Population Growth About.com
- ↑ Omran, Abdel R. "The Epidemiological Transition: A Theory of the Epidemiology of Population Change." The Milbank Memorial Fund Quarterly 49.4.1 (1971): 509-38. Print
- ↑ Preston, S.H. (1976). Mortality patterns in national populations: With special reference to recorded causes of death. New York: Academic Press.
- ↑ McMichael, A; McKee, M; Shkolnikov, V; Valkonen, T. (2004). "Mortality trends and setbacks: global convergence or divergence?". The Lancet. 363 (9415): 1155–1159.
- 1 2 3 Salomon, Joshua A. & Murray, Christopher J.L (2000), The Epidemiological Transition Revisited: New Compositional Models for Causes of Death by Age and Sex (PDF), The Global Burden of Disease 2000 in Aging Populations, Research paper No.01.17, retrieved 3 June 2010
- ↑ Murray, CJL (2015). "Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition.". The Lancet. 286 (10009): 2145–2191.