HIV/AIDS in the United States
The United States was the epicenter of the AIDS epidemic [1] of the 1980s, first noticed by doctors in young gay men in Los Angeles, New York City, and San Francisco in 1981. In the United States, 1.2 million people live with HIV, about 1/8th of whom are unaware of their infection.[1]
Public perception
One of the best known works on the history of HIV is 1987's book And the Band Played On, by Randy Shilts. Shilts contends that Ronald Reagan's administration dragged its feet in dealing with the crisis due to homophobia, while the gay community viewed early reports and public health measures with corresponding distrust, thus allowing the disease to spread and hundreds of thousands of people to needlessly die. This resulted in the formation of ACT-UP, the AIDS Coalition to Unleash Power by Larry Kramer.
This work popularized the misconception that the disease was introduced by a gay flight attendant named Gaëtan Dugas, referred to as "Patient Zero," although Shilts did not actually make this claim in the book. However, subsequent research has revealed that there were cases of AIDS much earlier than initially known. HIV-infected blood samples have been found from as early as 1959 in Africa (see HIV main entry), and HIV has been shown to have caused the death of Robert Rayford, a 16-year-old St. Louis male, in 1969, who could have contracted it as early as 7 years old due to sexual abuse, suggesting that HIV had been present, at very low prevalence, in the US since before the 1970s.
An early theory asserted that a series of inoculations against hepatitis B that were performed in the gay community of San Francisco were tainted with HIV. Although there was a high correlation between recipients of that vaccination and initial cases of AIDS, this theory has long been discredited. HIV, hepatitis B, and hepatitis C are bloodborne diseases with very similar modes of transmission, and those at risk for one are at risk for the others.[2]
Activists and critics of current AIDS policies allege that another preventable impediment to stemming the spread of the disease and/or finding a treatment was the vanity of "celebrity" scientists. Robert Gallo, an American scientist involved in the search for a new virus in the people affected by the disease, became embroiled in a legal battle with French scientist Luc Montagnier, who had first discovered such a virus in tissue cultures derived from a patient suffering from enlargement of the lymphnodes (an early sign of AIDS); Montagnier had named the new virus LAV (Lymphoadenopathy-Associated Virus). Gallo, who appeared to question the primacy of the French scientist's discovery, refused to recognize the "French virus" as the cause of AIDS, and tried instead to claim the disease was caused by a new member of a retrovirus family, HTLV, which he had discovered. Critics claim that because some scientists were more interested in trying to win a Nobel prize than in helping patients, research progress was delayed and more people needlessly died. After a number of meetings and high-level political intervention, the French scientists and Gallo agreed to "share" the discovery of HIV, although eventually Montagnier and his group were recognized as the true discoverers, and won the 2008 Nobel Prize for it.
Publicity campaigns were started in attempts to counter the often vitriolic and homophobic perception of AIDS as a "gay plague". These included the Ryan White case, red ribbon campaigns, celebrity dinners, the 1993 film version of And the Band Played On, sex education programs in schools, and television advertisements. Announcements by various celebrities that they had contracted HIV (including actor Rock Hudson, basketball star Magic Johnson, tennis player Arthur Ashe and singer Freddie Mercury) were significant in arousing media attention and making the general public aware of the dangers of the disease to people of all sexual orientations.
By Race/Ethnicity
Blacks/African Americans continue to experience the most severe burden of HIV, compared with other races and ethnicity. Blacks represent approximately 12% of the U.S. population, but accounted for an estimated 44% of new HIV infections in 2010. They also accounted for 41% of people living with HIV infection in 2011. Since the epidemic began, an estimated 270,726 blacks with AIDS have died, including an estimated 6,540 in 2012.[1]
Hispanics/Latinos are also disproportionately affected by HIV. Hispanics/Latinos represented 16% of the population but accounted for 21% of new HIV infections in 2010. Hispanics/Latinos accounted for 20% of people living with HIV infection in 2011. Disparities persist in the estimated rate of new HIV infections in Hispanics/Latinos. In 2010, the rate of new HIV infections for Latino males was 2.9 times that for white males, and the rate of new infections for Latinas was 4.2 times that for white females. Since the epidemic began, more than 100,888 Hispanics/Latinos with an AIDS diagnosis have died, including 2,155 in 2012.[1]
Containment
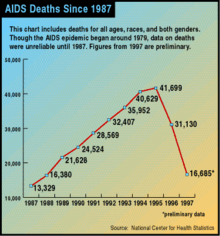

Great progress was made in the U.S. following the introduction of three-drug anti-HIV treatments ("cocktails") that included protease inhibitors. David Ho, a pioneer of this approach, was honored as Time Magazine Man of the Year for 1996. Deaths were rapidly reduced by more than half, with a small but welcome reduction in the yearly rate of new HIV infections. Since this time, AIDS deaths have continued to decline, but much more slowly, and not as completely in black Americans as in other population segments.[3][4]
Travel restrictions
The second prong of the American approach to containment has been to maintain strict entry controls to the country for people with HIV or AIDS. Under legislation enacted by the United States Congress in 1993, patients found importing anti-HIV medication into the country were arrested and placed on flights back to their country of origin.
Some HIV-positive travellers took to sending anti-HIV medication through the post to friends or contacts in advocacy groups in advance. This meant that the traveller would not be discovered with any medication. However, the security clampdown following the September 11 attacks in 2001 meant this was no longer an option.
The only legal alternative to this was to apply for a special visa beforehand, which entailed interview at an American Embassy, confiscation of the passport during the lengthy application process, and then, if permission were granted, a permanent attachment being made to the applicant's passport.
This process was condemned as intrusive and invasive by a number of advocacy groups, on the grounds that any time the passport was later used for travel elsewhere or for identification purposes, the holder's HIV status would become known. It was also felt that this rule was unfair because it applied even if the traveller was covered for HIV-related conditions under their own travel insurance.
In early December 2006, President George W. Bush indicated that he would issue an executive order allowing HIV-positive people to enter the United States on standard visas. It is unclear whether applicants will still have to declare their HIV status.[5] However, the ban remained in effect throughout Bush's Presidency. In August 2007, Congressperson Barbara Lee of California introduced H
On October 30, 2009 President Barack Obama reauthorized the Ryan White HIV/AIDS Bill which expanded care and treatment through federal funding to nearly half a million.[7] He also announced that the Department of Health and Human Services crafted regulation that would end the HIV Travel and Immigration Ban effective in January 2010;[7] on January 4, 2010, the United States Department of Health and Human Services, Centers for Disease Control and Prevention removed HIV status as a factor to be considered in the granting of travel visas.[8]
Medicine disbursement
Previously in the U.S., HIV drugs were only given to those who had T-cell counts of under 200, but that had been boosted in the mid 2000s to 350 on advice from the Journal of the American Medical Association (JAMA) guidelines which recommend therapy for all patients at 350 or certain patients higher. For the uninsured, there are generally two funding sources, Medicaid and AIDS Drug Assistance Programs (ADAP), both administered differently in each state but still consistent with federal requirements established by the Ryan White Care Act.
According to a recent large scale study, asymptomatic HIV positive patients who started on medication with T-cell counts 350 to 500 had a 70 percent higher survival rate than those who waited. The results from this shows that waiting even until the cell count reaches 350 (current JAMA recommendation) increases the risk of death, let alone the Medicaid eligible 200.[9] As many patients can't afford medicines without Medicaid help, HIV annual death counts have failed to decline significantly since 2002 despite great advances made before that date. The number of new cases in children has dropped significantly as a result of better screening of infected mothers as well as having established uniform testing and screening of blood products. This is not the same for places outside the United States, especially developing countries where the number of children affected by HIV continue to rise exponentially each year.[10]
Mortality and morbidity
Invariably, HIV is a silent disease when first acquired, though this latency varies in length. The progression from HIV infection to AIDS varies from 5–12 years. In the past, most individuals succumbed to the disease in 1–2 years after being diagnosed with AIDS. However, since the introduction of potent anti retroviral drug therapy and better prophylaxis against opportunistic infections, death rates have significantly declined.[11]
The overall death rate among persons diagnosed with HIV/AIDS in New York City decreased by 62% from 2001 to 2012.
Current status

CDC estimates that 1,218,400 persons aged 13 years and older are living with HIV infection, including 156,300 (12.8%) who are unaware of their infection. Over the past decade, the number of people living with HIV has increased, while the annual number of new HIV infections has remained relatively stable. Still, the pace of new infections continues at far too high a level—particularly among certain groups.
HIV Incidence (new infections): The estimated incidence of HIV has remained stable overall in recent years, at about 50,000 new HIV infections per year. Within the overall estimates, however, some groups are affected more than others. MSM continue to bear the greatest burden of HIV infection, and among races/ethnicities, African Americans continue to be disproportionately affected.
HIV Diagnoses (new diagnoses, regardless of when infection occurred or stage of disease at diagnosis): In 2013, an estimated 47,352 people were diagnosed with HIV infection in the United States. In that same year, an estimated 26,688 people were diagnosed with AIDS. Overall, an estimated 1,194,039 people in the United States have been diagnosed with AIDS.
Deaths: An estimated 13,712 people with an AIDS diagnosis died in 2012, and approximately 658,507 people in the United States with an AIDS diagnosis have died overall. The deaths of persons with an AIDS diagnosis can be due to any cause—that is, the death may or may not be related to AIDS. [13]
UNAIDS estimates that there are a total of about 1,200,000 people in the U.S. living with HIV as of 2009, and that 310,000 of these are women (female 15+ years of age).[14]
In California alone, 184,429 cases (including children) have reported to have contracted HIV by December 2008. Of those, 85,958 have died, with 31,076 in Los Angeles County, 18,838 in San Francisco, and 7,135 in San Diego County.[15]
In 2007, 119,929 people were living with HIV in the state of New York, with 92,669 in New York City alone.[16]
Washington DC has a particularly high incidence of HIV/AIDS, 177 new cases annually per 100,000 people, more than nine times higher than any state.[17]
In the United States, men who have sex with men (MSM)[18] make up about 57% of the total HIV-positive population (2011 data), and 63% of new HIV cases (2010 data).[19] A review of four studies in which trans women in the United States were tested for HIV found that 27.7% tested positive.[20]
In a 2008 study, the Center for Disease Control found that, of the study participants who were men who had sex with men ("MSM"), almost one in five (19%) had HIV and "among those who were infected, nearly half (44 percent) were unaware of their HIV status." The research found that those who are white MSM "represent a greater number of new HIV infections than any other population, followed closely by black MSM — who are one of the most disproportionately affected subgroups in the U.S." and that most new infections among white MSM occurred among those aged 30–39 followed closely by those aged 40–49, while most new infections among black MSM have occurred among young black MSM (aged 13–29).[21][22]
In 2015, a major HIV outbreak, Indiana's largest-ever, occurred in two largely rural, economically depressed and poor counties in the southern portion of the state, due to the injection of a relatively new opioid-type drug called Opana (oxymorphone), which should be taken in pill form but is ground up and injected intravenously using needles. Because of the lack of HIV cases in that area beforehand and the youth of many but not all of those affected, the relative unavailability in the local area of safe needle exchange programs and of treatment centers capable of dealing with long-term health needs, HIV care, and drug addiction during the initial phases of the outbreak, it was not initially adequately contained and dealt with until those were set up by the government, and acute awareness of the issue spread. Such centers have now been opened, and short-term care is beginning to be provided; despite some initial reservations, the Governor, once the scope of the outbreak became clear, approved a legislative measure to allow safe, clean needle exchange programs and treatment for those affected, which could end up being instituted statewide.[23]
See also
- Criminal transmission of HIV in the United States
- HIV/AIDS in American prisons
- Adult Industry Medical Health Care Foundation
- AIDS Education and Training Centers (AETCs)
- AIDS pandemic
- People With AIDS Self-Empowerment Movement
- HIV/AIDS in North America
- HIV/AIDS in New York City
References
- 1 2 3 4 "HIV in the United States | Statistics Overview | Statistics Center | HIV/AIDS | CDC". www.cdc.gov. Retrieved 2015-11-22.
- ↑ "Bloodborne Infectious Diseases HIV/AIDS, Hepatitis B Virus, and Hepatitis C Virus". US National Institute for Occupational Safety and Health. March 10, 2010. Retrieved March 21, 2010.
- ↑ Wilson, Phill; Wright, Kai; Isbell, Michael T. (August 2008). "Left Behind: Black America: a Neglected Priority in the Global AIDS Epidemic" (PDF). Black AIDS Institute. Archived from the original (PDF) on August 21, 2010. Retrieved March 20, 2010.
- ↑ "Deaths in New York City Reached Historic Low in 2002" (Press release). New York City Department of Health and Mental Hygiene. January 30, 2004. Retrieved March 20, 2010.
- ↑ Russell, Sabin (December 2, 2006). "Bush to ease rule limiting HIV-positive foreign visitors". San Francisco Chronicle. Hearst Communications. Retrieved March 21, 2010.
- ↑ | url =http://news.bbc.co.uk/2/hi/uk_news/8136456.stm | title = Activist helps US HIV law change | publisher = BBC News | accessdate = January 9, 2012
- 1 2 Crowley, Jeffrey (October 30, 2009). "Honoring the Legacy of Ryan White". WhiteHouse.gov. Office of the President of the United States. Retrieved March 21, 2010.
- ↑ "HIV Final Rule". United States Department of State. 2010-01-04. Retrieved 2010-04-30.
- ↑ Smith, Michael (October 27, 2008). "ICAAC-IDSA: HIV Treatment Started Sooner than Later Lessens Early Death Risk". MedPage Today, LLC. Retrieved March 21, 2010.
- ↑ "Epidemiology Research, HIV/AIDS". National Institute of Allergy and Infectious Diseases. November 12, 2009. Retrieved March 20, 2010.
- ↑ "2008 HIV/AIDS Epidemiology Annual Report" (PDF). San Francisco Department of Public Health. July 9, 2009. Retrieved March 21, 2010.
- ↑ "HIV/AIDS Basic Statistics". US Centers for Disease Control. February 26, 2009. Retrieved March 21, 2010.
- ↑ "HIV in the United States". Center for Disease Control. September 29, 2015. Retrieved June 29, 2016.
- ↑ "United States". HIV/AIDS Knowledge Base. University of California, San Francisco. Retrieved November 25, 2011.
- ↑ "December 2008 Monthly HIV/AIDS Statistics" (PDF). California Department of Public Health Office of AIDS. July 9, 2009. Retrieved March 21, 2010.
- ↑ "New York State HIV/AIDS Surveillance Annual Report For Cases Diagnosed Through December 2007" (PDF). New York State Department of Public Health. May 2009. Retrieved March 21, 2010.
- ↑ "The HIV/AIDS Epidemic in the United States". Kaiser Family Foundation. March 22, 2013. Retrieved June 2, 2012.
- ↑ http://www.cdc.gov/hiv/risk/gender/msm/facts/index.html
- ↑ UNAIDS Report on the Global AIDS Epidemic 2010 (p 50)
- ↑ "Estimating HIV Prevalence and Risk Behaviors of Transgender Persons in the United States: A Systematic Review". AIDS Behav. 12 (1): 1–17. Jan 2008. doi:10.1007/s10461-007-9299-3. PMID 17694429.
- ↑ CDC Fact Sheet - HIV and AIDS among Gay and Bisexual Men - Sept 2010
- ↑ CDC: One In Five Gay Men HIV-Positive
- ↑ Block, Melissa; Adams, Jerome (24 April 2015). "HIV Outbreak In Indiana Grows With Nearly 140 Confirmed Cases". NPR. Retrieved 4 May 2015.
Bibliography
- Cante, Richard C. (March 2008). Gay Men and the Forms of Contemporary US Culture. London: Ashgate Publishing. ISBN 0-7546-7230-1.
- Bogart, Laura; Thorburn, Sheryl (February 2005). "Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans?". J. Acquir. Immune Defic. Syndr. 38 (2): 213–8. doi:10.1097/00126334-200502010-00014. PMID 15671808.
- Walker, Robert Searles (1994). AIDS: Today, Tomorrow : an Introduction to the HIV Epidemic in America (2nd ed.). Atlantic Highlands, New Jersey: Humanities Press Intl. ISBN 0-391-03859-1. OCLC 30399464.
- Siplon, Patricia (2002). AIDS and the policy struggle in the United States. Washington D.C.: Georgetown University Press. ISBN 978-0-87840-378-3. OCLC 48964730.
External links
- AIDS.gov – The U.S. Federal Domestic HIV/AIDS Resource
- AIDSVu.org - Interactive Map Illustrating HIV Prevalence in the United States