Sebaceous adenitis
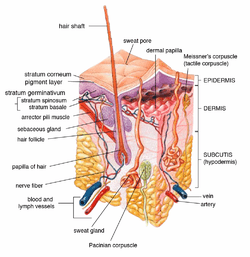
In canines, sebaceous adenitis, or SA, refers to the autoimmune disease found in some breeds of dog and more rarely in cats, rabbits and horses. It is an uncommon, idiopathic skin disease,[1] characterised by an immune response against the dog's sebaceous glands (glands found in the hair follicles in the skin dermis), which can lead to the destruction of the gland. It was first described in veterinary literature in the 1980s.[2]
Description

Sebaceous adenitis is an autoimmune, inflammatory, skin disease of currently unknown cause. Research is currently underway to find if there is a genetic predisposition for SA, and the exact mode of inheritance remains unknown.[3] However, it is postulated that it is an autosomal recessive acquired condition.[4] It has no sex-predisposition.[1] There are two expressions of this condition, one for long or double coated breeds and one for short coated breeds, both with differing presentations.[4]
For long- or double-coated breeds such as Poodles, Akitas and Samoyeds, the condition often presents itself with silvery dandruff which adheres to the coat, hair loss (not to be confused with moulting or "blowing coat"), a dull and brittle coat, and later on skin lesions along the back and ears[4] as well as thickened skin and a musty or rancid odour.[5] For short-coated breeds such as Vizslas, the condition causes facial swellings, nodular skin lesions, fine dandruff which does not adhere to the coat, and a general "moth-eaten" appearance to the coat.[4]
Etymology
Sebaceous refers to the gland which is targeted by the immune system of affected animals. Adenitis is a general term referring to the inflammation of a gland.
Susceptibility of certain breeds of dog
While the condition has been seen in over 60 breeds of dog (including cross breeds),[6] certain breeds have been found to be more susceptible than others to sebaceous adenitis:
- American Akita and Akita Inu[7][8]
- Standard Poodle[7][8]
- Vizsla[7][8]
- English Springer Spaniel[9]
- Chow Chow[10][11]
- Samoyed[1][8]
- Weimaraner[8]
- Havanese[12]
Breeds also mentioned in scientific literature as having some susceptibility include:
- German Shepherd Dog[10]
- Dachshund[1]
- Old English Sheepdog[10]
- Lhasa Apso[10]
- Boxer[10]
- Collie[10]
- Toy Poodle[10]
- Mixed-breeds[4]
There has also been mention of the condition in cats,[8] rabbits[4][13] and horses.[14]
Diagnosis
In general, SA in canines is underdiagnosed.[1] It has however been described in more than 60 breeds of dog as well as mixed breeds.[11] Diagnosis confirmation requires multiple punch biopsies analysed by a dermopathologist who will comment on the condition of the sebaceous glands, revealing granulomatous or pyogranulomatous inflammation surrounding the sebaceous glands or even complete destruction of sebaceous glands.[8]
Other conditions with similar presentations include: bacterial folliculitis and demodicosis, dermatophytosis, endocrinopathy, pemphigus foliaceus, Zinc responsive dermatosis, vitamin A-responsive dermatosis, ichthyosis, and nutritional deficiencies.[11] As well as, superficial pyoderma, primary idiopathic seborrhea and other endocrine diseases.[8]
Treatment
There is no cure for this condition. Treatment is generally lifelong[4] and takes the form of bathing and soaking in mineral oils and washing with antibiotic shampoos to try to alleviate symptoms and slow the condition's progression.[15] Antiseptic and antibiotic shampoos (chlorhexidine or benzoyl peroxide) are used to manage further secondary bacterial infection.[11] For some breeds, cyclosporine or corticosteroids and immunosuppressant drugs may be effective,[4] and it is postulated, through some studies, that large doses of vitamin A given orally may result in some improvement.[4]
It has been suggested in the paper by Angus (2009) that the more aggressively one applies the topical methods of treatment, the less aggressively one needs to employ the immunosuppressant therapy. The suggestion is that this phenomenon may be due to a cyclic feedback whereby secondary infection, when not aggressively treated with topical therapy, increases and contributes to further sebaceous gland inflammation.[11]
Topical Therapy
This forms a major and critical part in the disease treatment and the shampoo treatment can need to be applied as often as 3 to 4 times per week.[11] An antiseborrheic shampoo removes the scale blocking theolr follicles. The mineral oil soak, whereby the oil remains on the affected animal for at least 2 hours, is needed to replace epidemal lipids as well as to restore normal epidermal barrier function. The oil is then removed through the process of many baths. This oil treatment needs to be repeated at least once a week for 4 to 7 weeks until new hair growth is observed.[11] Once new hair growth is observed, topical treatment can be decreased to every 2 to 4 weeks.
Immunosuppressant Therapy
Immunosuppressant and anti-inflammatory therapy serves to stop on-going destruction of the sebaceous glands. Like other immune-mediated diseases, most animals receive an initial course to stop the inflammation and treatment is tapered off to the lowest dose that keeps the disease in remission.[11] Initially, oral cyclosporine is given in doses of 5 mg/kg twice daily and then gradually decreased in frequency.[11]
Corticosteroids (e.g. Prednisone) are used only if pruritus is a major clinical feature, and is given at 2 mg/kg/day for 2 to 4 weeks and then tapered to withdrawal.[11]
Dietary Supplementation
These are commonly included in treatments of SA and include:
- Omega 6 Fatty Acids (e.g. Safflower or sunflower oil)
- Omega 3 Fatty Acids (e.g. Fish olis)
- Vitamin A at 8,000 to 10,000 IU twice daily and up to 20,000 to 30,000IU twice daily, not exceeding 1000IU/kg/day, if no improvement is seen within 3 months.[11]
References
- 1 2 3 4 5 Craig, Mark (2006). "Clinical refresher: Canine sebaceous adenitis". Companion Animal. 11 (5): 62–8. doi:10.1111/j.2044-3862.2006.tb00066.x.
- ↑ Spaterna, A.; Antognoni, M.T.; Cappuccini, S.; Tesei, B. (2003). "Sebaceous Adenitis in the Dog: Three Cases". Veterinary Research Communications. 27: 441–443. doi:10.1023/B:VERC.0000014199.39879.bb. PMID 14535449.
- ↑ Koch, Sandra N. (June 1, 2009 – November 30, 2010). "01346-A: Genetic Basis of Sebaceous Adenitis in Dogs". University of Minnesota. Retrieved 7 April 2011.
- 1 2 3 4 5 6 7 8 9 Linek, Monika (2008). "Sebaceous adenitis in the dog" (PDF). Veterinary Focus. 18 (1): 12–16. Retrieved 10 April 2011.
- ↑ "Sebaceous Adenitis". Canine Inherited Disorders Database. 1998. Archived from the original on June 5, 2011. Retrieved 10 April 2011.
- ↑ Mr Charlie Walker BVetMed CertVD MRCVS (2010). "Skin: idiopathic/granulomatous sebaceous adenitis". Cambridge CB21 4EN, UK: VetStream. Retrieved 19 July 2011.
- 1 2 3 Pfeiffer, Ina (April 1 – June 30, 2006). "577-AT: Sebaceous Adenitis in the Akita". Retrieved 7 April 2011.
- 1 2 3 4 5 6 7 8 Hall, Jan A. (2005). "Congenital and Hereditary Defects in Skin Disease". Ontario Veterinary College, University of Guelph, Canada: Omnibooks Online. Retrieved 2 June 2011.
- ↑ Hernblad Tevell, E; Bergvall, K; Egenvall, A (2008). "Sebaceous adenitis in Swedish dogs, a retrospective study of 104 cases". Acta veterinaria Scandinavica. 50: 11. doi:10.1186/1751-0147-50-11. PMC 2412885
 . PMID 18501018.
. PMID 18501018. - 1 2 3 4 5 6 7 Gross, Thelma Lee; Peter J. Ihrke; Emily J. Walder; Verena K. Affolter (2005). Skin diseases of the dog and cat: clinical and histopathologic diagnosis (second ed.). Wiley-Blackwell. pp. 186–8. ISBN 978-0-632-06452-6.
- 1 2 3 4 5 6 7 8 9 10 11 Angus, DVM, DACVD, John C. (2009). "How I Treat Sebaceous Adenitis". Animal Dermatology Clinic, Pasadena, CA, USA: Omnibooks Online. p. 1. Retrieved 2 June 2011.
- ↑ Frazer, Megan; Anthea E. Schick; Thomas P. Lewis; Edward Jazic (June 2011). "Sebaceous adenitis in Havanese dogs: a retrospective study of the clinical presentation and incidence". Veterinary Dermatology. 22 (3): 267–274. doi:10.1111/j.1365-3164.2010.00942.x.
- ↑ Anna Meredith; Stephen White (2010). "Sebaceous adenitis". Cambridge CB21 4EN, UK: VetStream. Retrieved 19 July 2011.
- ↑ Osborne, Christina (2006). "Sebaceous adenitis in a 7-year-old Arabian gelding". The Canadian veterinary journal. La revue veterinaire canadienne. 47 (6): 583–6. PMC 1461412
 . PMID 16808233.
. PMID 16808233. - ↑ "Inflammatory Skin Disease in Dogs". Retrieved 10 April 2011.
External links
Not used in Article
- http://www.vin.com/VINDBPub/SearchPB/Proceedings/PR05000/PR00094.htm General clinical introduction. Accessed 08/April 2011
- http://www.petmd.com/dog/conditions/skin/c_dg_sebaceous_adenitis?page=2 For an introduction to the topic. Accessed 08/April 2011
- http://www.upei.ca/~cidd/Diseases/dermatology/sebaceous%20adenitis.htm General FAQ. Accessed 08/April 2011
- http://www.edliny.com/Encyclopedy/Veterinary%20Focus/181/2.pdf More advanced introduction, diagnosis and treatments. Accessed 08/April 2011
- Reichler, Iris M.; Hauser, Beat; Schiller, Irene; Dunstan, Robert W.; Credille, Kelly M.; Binder, Heinrich; Glaus, Toni; Arnold, Susi (2001). "Sebaceous adenitis in the Akita: clinical observations, histopathology and heredity". Veterinary Dermatology. 12 (5): 243–53. doi:10.1046/j.0959-4493.2001.00251.x. PMID 11906649.
- http://www.vetwest.com.au/skin-deep-issue-so-whats-difference-between-canine-and-human-skin Explanation of the differences between Human and Canine skin. Accessed 12/April/2011