Abetalipoproteinemia
| Abetalipoproteinemia | |
|---|---|
|
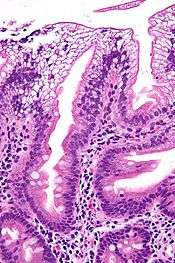
Micrograph showing enterocytes with a clear cytoplasm (due to lipid accumulation) characteristic of abetalipoproteinemia. Duodenal biopsy. H&E stain. | |
| Classification and external resources | |
| Specialty | endocrinology |
| ICD-10 | E78.6 |
| ICD-9-CM | 272.5 |
| OMIM | 200100 |
| DiseasesDB | 17 |
| MedlinePlus | 001666 |
| eMedicine | med/1117 |
| MeSH | D000012 |
Abetalipoproteinemia, or Bassen-Kornzweig syndrome,[1] is a rare autosomal recessive[2] disorder that interferes with the normal absorption of fat and fat-soluble vitamins from food. It is caused by a mutation in microsomal triglyceride transfer protein resulting in deficiencies in the apolipoproteins B-48 and B-100, which are used in the synthesis and exportation of chylomicrons and VLDL respectively. It is not to be confused with familial dysbetalipoproteinemia.
Features
Abetalipoproteinemia affects the absorption of dietary fats, cholesterol, and certain vitamins. People affected by this disorder are not able to make certain lipoproteins, which are molecules that consist of proteins combined with cholesterol and particular fats called triglycerides. This leads to a multiple vitamin deficiency, affecting the fat-soluble vitamin A, vitamin D, vitamin E, and vitamin K.[3] However, many of the observed effects are due to vitamin E deficiency in particular.[3]

The signs and symptoms of abetalipoproteinemia appear in the first few months of life (because pancreatic lipase is not active in this period). They can include failure to gain weight and grow at the expected rate (failure to thrive); diarrhea; abnormal star-shaped red blood cells (acanthocytosis); and fatty, foul-smelling stools (steatorrhea).[3] The stool may contain large chunks of fat and/or blood. Other features of this disorder may develop later in childhood and often impair the function of the nervous system. They can include poor muscle coordination, difficulty with balance and movement (ataxia),[3][4] and progressive degeneration of the retina (the light-sensitive layer in the posterior eye) that can progress to near-blindness (due to deficiency of vitamin A, retinol).[3] Adults in their thirties or forties may have increasing difficulty with balance and walking. Many of the signs and symptoms of abetalipoproteinemia result from a severe vitamin deficiency, especially vitamin E deficiency, which typically results in eye problems with degeneration of the spinocerebellar and dorsal column tracts.
Presentation
Symptoms
Often symptoms will arise that indicate the body is not absorbing or making the lipoproteins that it needs. These symptoms usually appear en masse, meaning that they happen all together, all the time. These symptoms come as follows:
- Failure to thrive/Failure to grow in infancy[5]
- Steatorrhea/Fatty, pale stools[5][6]
- Frothy stools[5]
- Foul smelling stools[5]
- Protruding abdomen
- Intellectual disability/developmental delay
- Developmental coordination disorder, evident by age ten
- Muscle weakness
- Slurred speech
- Scoliosis (curvature of the spine)
- Progressive decreased vision
- Balance and coordination problems
Signs
- Acanthocytosis[5][7]
- Retinitis pigmentosa
- Hypocholesterolemia/low blood cholesterol[6]
Diagnosis
The initial workup of abetalipoproteinemia typically consists of stool sampling, a blood smear, and a fasting lipid panel though these tests are not confirmatory.[8] As the disease is rare, though a genetics test is necessary for diagnosis, it is generally not done initially.
Acanthocytes are seen on blood smear.[9] Since there is no or little assimilation of chylomicrons, their levels in plasma remains low.
The inability to absorb fat in the ileum will result in steatorrhea, or fat in the stool. As a result, this can be clinically diagnosed when foul-smelling stool is encountered. Low levels of plasma chylomicron are also characteristic.
There is an absence of apolipoprotein B. On intestinal biopsy, vacuoles containing lipids are seen in enterocytes. This disorder may also result in fat accumulation in the liver (hepatic steatosis). Because the epithelial cells of the bowel lack the ability to place fats into chylomicrons, lipids accumulate at the surface of the cell, crowding the functions that are necessary for proper absorption.
Genetics

Mutations in the microsomal triglyceride transfer protein (MTTP) gene has been associated with this condition.[3] (Apolipoprotein B deficiency, a related condition, is associated with deficiencies of apolipoprotein B.)[10]
The MTTP gene provides instructions for making a protein called microsomal triglyceride transfer protein, which is essential for creating beta-lipoproteins.[11] These lipoproteins are both necessary for the absorption of fats, cholesterol, and fat-soluble vitamins from the diet and necessary for the efficient transport of these substances in the bloodstream.[12] Most of the mutations in this gene lead to the production of an abnormally short microsomal triglyceride transfer protein, which prevents the normal creation of beta-lipoproteins in the body.[13] MTTP-associated mutations are inherited in an autosomal recessive pattern, which means both copies of the gene must be faulty to produce the disease.[13]
Treatment
Treatment normally consists of rigorous dieting, involving massive amounts of vitamin E.[4] Vitamin E helps the body restore and produce lipoproteins, which people with abetalipoprotenimia usually lack. Vitamin E also helps keep skin and eyes healthy; studies show that many affected males will have vision problems later on in life. Developmental coordination disorder and muscle weakness are usually treated with physiotherapy or occupational therapy. Dietary restriction of triglycerides has also been useful.
Prognosis
If treatment is initiated early in disease the neurologic sequelae may be reversed and further deterioration can be prevented.[14]
References
- ↑ Bassen FA; Kornzweig AL (1950). "Malformation of the erythrocytes in a case of atypical retinitis pigmentosa". Blood. 5 (4): 381–87. PMID 15411425.
- ↑ Benayoun, Liat; Granot, Esther; Rizel, Leah; Allon-Shalev, Stavit; Behar, Doron M.; Ben-Yosef, Tamar (April 2007). "Abetalipoproteinemia in Israel: Evidence for a founder mutation in the Ashkenazi Jewish population and a contiguous gene deletion in an Arab patient". Molecular Genetics and Metabolism. 90 (4): 453–7. doi:10.1016/j.ymgme.2006.12.010. PMID 17275380.
- 1 2 3 4 5 6 "Abetalipoproteinemia - Genetics Home Reference". Retrieved 2008-02-24.
- 1 2 Hentati, F; El-Euch, G; Bouhlal, Y; Amouri, R (2012). "Ataxia with vitamin E deficiency and abetalipoproteinemia". Handbook of clinical neurology. Handbook of Clinical Neurology. 103: 295–305. doi:10.1016/B978-0-444-51892-7.00018-8. ISBN 9780444518927. PMID 21827896.
- 1 2 3 4 5 Hasosah, MY; Shesha, SJ; Sukkar, GA; Bassuni, WY (2010). "Rickets and dysmorphic findings in a child with abetalipoproteinemia". Saudi medical journal. 31 (10): 1169–71. PMID 20953537.
- 1 2 Moutzouri, E; Elisaf, M; Liberopoulos, EN (March 2011). "Hypocholesterolemia.". Current Vascular Pharmacology. 9 (2): 200–12. doi:10.2174/157016111794519354. PMID 20626336.
- ↑ Cooper RA; Durocher JR; Leslie MH (July 1977). "Decreased fluidity of red cell membrane lipids in abetalipoproteinemia". J. Clin. Invest. 60 (1): 115–21. doi:10.1172/JCI108747. PMC 372349
 . PMID 874076.
. PMID 874076. - ↑ Demircioğlu, F; Oren, H; Yilmaz, S; Arslan, N; Gürcü, O; Irken, G (August 2005). "Abetalipoproteinemia: importance of the peripheral blood smear.". Pediatric blood & cancer. 45 (2): 237. doi:10.1002/pbc.20360. PMID 15765527.
- ↑ Ozsoylu, S (Jan–Feb 2011). "Red cells in abetalipoproteinemia.". The Turkish journal of pediatrics. 53 (1): 119. PMID 21534356.
- ↑ Hussain, M Mahmood; Rava, Paul; Walsh, Meghan; Rana, Muhammad; Iqbal, Jahangir (2012). "Multiple functions of microsomal triglyceride transfer protein". Nutrition & Metabolism. 9: 14. doi:10.1186/1743-7075-9-14. PMC 3337244
 . PMID 22353470.
. PMID 22353470. - ↑ Mohamed, N; Mohamed Youssef, S; Mohamed Yahia, H; Afef, S; Awatef, J; Saber, H; Mohamed Fadhel, N; Sassolas, A; Mohamed Naceur, S (Apr 4, 2013). "Molecular characterization of Tunisian families with abetalipoproteinemia and identification of a novel mutation in MTTP gene". Diagnostic pathology. 8 (1): 54. doi:10.1186/1746-1596-8-54. PMC 3632489
 . PMID 23556456.
. PMID 23556456. - ↑ Magnolo, Lucia; Najah, Mohamed; Fancello, Tatiana; Di Leo, Enza; Pinotti, Elisa; Brini, Ines; Gueddiche, Neji M.; Calandra, Sebastiano; Slimene, Naceur M.; Tarugi, Patrizia (2013). "Novel mutations in SAR1B and MTTP genes in Tunisian children with chylomicron retention disease and abetalipoproteinemia". Gene. 512 (1): 28–34. doi:10.1016/j.gene.2012.09.117. PMID 23043934.
- 1 2 Pons, Véronique; Rolland, Corinne; Nauze, Michel; Danjoux, Marie; Gaibelet, Gérald; Durandy, Anne; Sassolas, Agnès; Lévy, Emile; Tercé, François; Collet, Xavier; Mas, Emmanuel (July 2011). "A severe form of abetalipoproteinemia caused by new splicing mutations of microsomal triglyceride transfer protein (MTTP)". Human Mutation. 32 (7): 751–9. doi:10.1002/humu.21494. PMID 21394827.
- ↑ Rader, DJ; Brewer HB, Jr (Aug 18, 1993). "Abetalipoproteinemia. New insights into lipoprotein assembly and vitamin E metabolism from a rare genetic disease.". JAMA: the Journal of the American Medical Association. 270 (7): 865–9. doi:10.1001/jama.1993.03510070087042. PMID 8340987.
External links
- Abetalipoproteinemia at NLM Genetics Home Reference
- AllRefer.com Bassen-Kornzweig syndrome
- David Alexander Leaf. "Abetalipoproteinemia:". Epocrates Online. Retrieved 13 May 2013.