Conduction aphasia
| Conduction aphasia | |
|---|---|
 | |
| Broca's area and Wernicke's area | |
| Classification and external resources | |
| MeSH | D018886 |
Conduction aphasia, also called associative aphasia, is a relatively rare form of aphasia. An acquired language disorder, it is characterized by intact auditory comprehension, fluent (yet paraphasic) speech production, but poor speech repetition. They are fully capable of understanding what they are hearing, but show significant difficulty repeating phrases, particularly as the phrases increase in length and complexity and as they stumble over words they are attempting to pronounce.[1][2] Patients will display frequent errors during spontaneous speech, such as substituting or transposing sounds. They will also be aware of their errors, and will show significant difficulty correcting them.[3] Shallice and Warrington (1970) were able to differentiate two variants of this constellation: the reproduction and the repetition type. These authors suggested an exclusive deficit of auditory-verbal short-term memory in repetition conduction aphasia whereas the other variant was assumed to reflect disrupted phonological encoding mechanism, afflicting confrontation tasks such as repetition, reading and naming in a similar manner.[4]
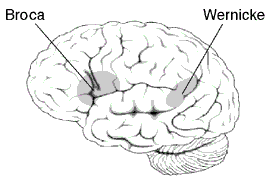
Typical lesion location for conduction aphasia is on the supramarginal gyrus of the parietal lobe, posterior to the primary sensory cortex and just above Wernicke's area.[5] The classical explanation for conduction aphasia is that of a disconnection between the brain areas responsible for speech comprehension (Wernicke's area) and speech production (Broca's area), due specifically to damage to the arcuate fasciculus, a deep white matter tract. Recent research has challenged this notion on the basis that patients with conduction aphasia more often have lesions in the supramarginal gyrus or deep parietal matter. However, conduction aphasia remains a controversial topic from the understanding of its neurologic foundations.
Presentation
Conduction aphasics will show relatively well-preserved auditory comprehension, which may even be completely functional. Spontaneous speech production will be fluent and generally grammatically and syntactically correct. Intonation and articulation will also be preserved. Speech will often contain paraphasic errors: phonemes and syllables will be dropped or transposed (e.g., "snowball" → "snowall", "television" → "vellitision", "ninety-five percent" → "ninety-twenty percent"). The hallmark deficit of this disorder, however, is in repetition. Patients will show a marked inability to repeat words or sentences when prompted by an examiner.[6][7] After saying a sentence to a person with conduction aphasia, he or she will be able to paraphrase the sentence accurately but will not be able to repeat it.[8] When prompted to repeat words, patients will be unable to do so, and produce many paraphasic errors. For example, when prompted with "bagger", a patient may respond with, "gabber".[9] Oral reading can also be poor.
Patients recognize their paraphasias and errors and will try to correct them, with multiple attempts often necessary for success. Error sequences frequently fit a pattern of incorrect approximations featuring known morphemes that a) share one or more similarly located phonemes but b) differ in at least one aspect that makes the substituted morpheme(s) semantically distinct. This repetitive effort to approximate the appropriate word or phrase is known as conduite d’approche.[7] For example, when prompted to repeat "Rosenkranz", a German-speaking patient may respond with, "rosenbrau... rosenbrauch... rosengrau... bro... grosenbrau... grossenlau, rosenkranz,... kranz... rosenkranz".[9]
Conduction aphasia is a relatively mild language impairment, and most patients return to day-to-day life.[9][10] Symptoms of conduction aphasia, as with other aphasias, can be transient, lasting only several hours or a few days. As aphasias and other language disorders are frequently due to stroke, their symptoms can change and evolve over time, or simply disappear. This is due to healing in the brain after inflammation or hemorrhage, which leads to decreased local impairment. Furthermore, plastic changes in the brain may lead to the recruitment of new pathways to restore lost function. However, chronic conduction aphasia is possible, without transformation to other aphasias.[9] These patients show prolonged, profound deficits in repetition, frequent phonemic paraphasias, and conduite d'approche during spontaneous speech.
Causes
Conduction aphasia is caused by damage to the parietal lobe of the brain.[11] The arcuate fasciculus, which connects Broca's area and Wernicke's area (important for speech and language production and comprehension, respectively), is affected.[11] These two areas control speech and language in the brain. The arcuate fasciculus is a thick band of fiber that connects the two areas and carries messages between them. Basically, the phonological systems involved in speech output are impaired.[12] Lesions in the language centers (and connections between) have been identified as potential inducers for conduction aphasia (and other language disorders, in general). Specifically, patterns of damage in conduction aphasia patients have been observed to cluster in the posterior and inferior temporal lobe, and in the parietal-temporal junction.[6][9]
The brain damage causing conduction aphasia is often from a stroke, which can produce both localized and widespread damage. Traumatic brain injury and tumors can also lead to localized lesions, with potential to cause conduction aphasia. Conduction aphasia can also be seen in cases of cortical damage without subcortical extensions.[13]
Pathophysiology
Traditionally, it has been believed that conduction aphasia was the result of a lesion in the arcuate fasciculus, a deep, white matter bundle connecting the posterior temporoparietal junction with the frontal cortex. It was thought that this bundle transmitted information between Wernicke's area (responsible for language comprehension) and Broca's area (responsible for language production). Wernicke, and later Lichtheim and others, theorized that a disconnect between these two regions caused patients to fail to monitor speech and limited their ability to transfer information between comprehension and production functions, thus leading to paraphasic errors and a deficit in repetition of auditory input. This hypothesis fits well with the Wernicke-Geschwind model of language, which compartmentalizes and localizes speech comprehension and production.
Although the disconnection hypothesis explains many of the conditions associated with conduction aphasia, clinical evidence is lacking, and the Wernicke-Geschwind model has since become obsolete. There have been no known autopsy cases in which conduction aphasia was shown to be the result of a focused arcuate fasciculus lesion.[14] Surveys of conduction aphasics with anatomical confirmation show that in nearly all patients, there was damage to portions of the cortex as well. Furthermore, there are reports of patients with severe disruption of the arcuate fasciculus who show no symptoms of conduction aphasia (although it is plausible that the contralateral hemisphere facilitated repetition in these cases).[15]
Recent research has pointed to a different explanation for conduction aphasia, similar to Wernicke's, which is based on newer models suggesting language is facilitated by "cortically based, anatomically distributed, modular networks."[16] Anderson et al. describe an experiment in which electrical stimulation of the left posterior superior temporal cortex in a human subject induced symptoms consistent with conduction aphasia, indicating that a deep brain disconnection is not necessary.[16] While this study does not completely discredit the disconnection hypothesis, but does point to a system in which transmission of spoken language information involves more than just the arcuate fasciculus. Regardless of the role that the arcuate fasciculus plays in the disorder, the cortical component cannot be denied.
Diagnosis
Individuals with conduction aphasia are able to express themselves fairly well, with some word finding difficulty, and functional comprehension.[17] Although people with aphasia may be able to express themselves fairly well, they tend to have issues repeating phrases, especially phrases that are long and complex.[17] When asked to repeat something, the patient will be unable to do so without significant difficulty, repeatedly attempting to self-correct (conduite d'approche). When asked a question, however, patients can answer spontaneously and fluently.
Several standardized test batteries exist for diagnosing and classifying aphasias. These tests are capable of identifying conduction aphasia with relative accuracy.[7] The Boston Diagnostic Aphasia Examination (BDAE) and the Western Aphasia Battery (WAB) are two commonly used test batteries for diagnosing conduction aphasia. These examinations involve a set of tests, which include asking patients to name pictures, read printed words, count aloud, and repeat words and non-words (such as shwazel).
Treatment
Treatment for aphasias is generally individualized, focusing on specific language and communication improvements, and regular exercise with communication tasks. Regular therapy for conduction aphasics has been shown to result in steady improvement on the Western Aphasia Battery.[18] However, conduction aphasia is a mild aphasia, and conduction aphasics score highly on the WAB at baseline.
History
In the late 19th century, Paul Broca studied patients with expressive aphasia. These patients had lesions in the anterior perisylvian region (now known as Broca's area), and produced halting and labored speech, lacking in function words and grammar. Comprehension is generally preserved, although there can be deficits in interpretation of complex sentences. In an extreme example, one of his patients could only produce a single syllable, "Tan".
Meanwhile, Carl Wernicke described patients with receptive aphasia, who had damage to the left posterior superior temporal lobe, which he named "the area of word images". These patients could speak fluently, but their speech lacked meaning. They had a severe deficit in auditory comprehension. The two disorders (expressive and receptive aphasias) thus seemed complementary, and corresponded to two distinct anatomical locations.
Wernicke predicted the existence of conduction aphasia in his landmark 1874 monograph, Der Aphasische Symptomenkompleks: Eine Psychologische Studie auf Anatomischer Basis.[3][16][19] He was the first to distinguish the various aphasias in an anatomical framework, and proposed that a disconnection between the two speech systems (motor and sensory) would lead to a unique condition, distinct from both expressive and receptive aphasias, which he termed Leitungsaphasie. He did not explicitly predict the repetition deficit, but did note that, unlike those with Wernicke's aphasia, conduction aphasics would be able to comprehend speech properly, and intriguingly, would be able to hear and understand their own speech errors, leading to frustration and self-correction.[19][20]
Wernicke was influenced by Theodor Meynert, his mentor, who postulated that aphasias were due to perisylvian lesions. Meynert also distinguished between the posterior and anterior language systems, leading Wernicke to localize the two regions.[16] Wernicke's research into the fiber pathways connecting the posterior and anterior regions lead him to theorize that damage to the fibers under the insula would lead to conduction aphasia. Ludwig Lichtheim expanded on Wernicke's work, although he labeled the disorder commissural aphasia, to distinguish between aphasias tied to processing centers.[21]
Sigmund Freud would argue in 1891 that the old framework was inaccurate; the entire perisylvian area, from the posterior to the anterior regions, were equivalent in facilitating speech function. In 1948 Kurt Goldstein postulated that spoken language was a central phenomenon, as opposed to a differentiated and disparate set of functionally distinct modules. To Freud and Goldstein, conduction aphasia was thus the result of a central, core language breakdown; Goldstein labeled the disorder central aphasia.[16]
Later work and examination of brain structures, however, implicated the arcuate fasciculus, a white matter bundle connecting the posterior temporoparietal junction with the frontal cortex. Norman Geschwind proposed that damage to this bundle caused conduction aphasia; the characteristic deficits in auditory repetition were due to failed transmission of information between the two language centers.[16] Studies showed that conduction aphasics had an intact 'inner voice', which discredited the central deficit model of Freud and Goldstein.[22] The Wernicke-Lichtheim-Geschwind disconnection hypothesis thus became the prevailing explanation for conduction aphasia. However, recent reviews and research have cast doubt on the singular role of the arcuate fasciculus and the model of spoken language in general.
See also
References
- ↑ Conduction Aphasia. (n.d.). Retrieved from http://www.asha.org/Glossary/Conduction-Aphasia/
- ↑ Carlson, Neil R.; Heth, C. Donald (2007). Psychology the science of behaviour (4th ed.). Pearson Education Inc. ISBN 0-205-64524-0.
- 1 2 Gazzaniga, Michael S.; Ivry, Richard B.; George R. Mangun (2002). Cognitive neuroscience: the biology of the mind. New York: W. W. Norton. p. 389. ISBN 0-393-97777-3.
- ↑ Sidiropoulos K, de Bleser R, Ackermann H, Preilowski B (Dec 2008). "Pre-lexical disorders in repetition conduction aphasia". Neuropsychologia. 46 (14): 3225–38. doi:10.1016/j.neuropsychologia.2008.07.026. PMID 18761023.
- ↑ Manasco, M. H. (2014). Introduction to Neurogenic Communication Disorders. Burlington: Jones & Bartlett Learning.
- 1 2 Damasio H, Damasio AR (June 1980). "The anatomical basis of conduction aphasia". Brain. 103 (2): 337–50. doi:10.1093/brain/103.2.337. PMID 7397481.
- 1 2 3 Kohn, Susan E. (1992). Conduction aphasia. Hillsdale, N.J: L. Erlbaum. pp. 40–42. ISBN 0-8058-0681-4.
- ↑ Manasco, M. (2014). Chapter 4: The Aphasias. In Introduction to neurogenic communication disorders . Burlington, MA: Jones & Barlett Learning.
- 1 2 3 4 5 Bartha L, Benke T (April 2003). "Acute conduction aphasia: an analysis of 20 cases". Brain Lang. 85 (1): 93–108. doi:10.1016/S0093-934X(02)00502-3. PMID 12681350.
- ↑ Benson DF, Sheremata WA, Bouchard R, Segarra JM, Price D, Geschwind N (May 1973). "Conduction aphasia. A clinicopathological study". Arch. Neurol. 28 (5): 339–46. doi:10.1001/archneur.1973.00490230075011. PMID 4696016.
- 1 2 Manasco, M. Hunter (2014). Introduction to Neurogenic Communication Disorders. Jones & Bartlett Learning.
- ↑ Kohn, Susan E. (1992). Conduction aphasia. Hillsdale, N.J: L. Erlbaum. p. 1035. ISBN 0-8058-0681-4.
- ↑ Ardila A. (November 2010). " A Review of Conduction aphasia". Current Neurology and Neuroscience Reports. 10 (6): 499-503.
- ↑ Tanabe H, Sawada T, Inoue N, Ogawa M, Kuriyama Y, Shiraishi J (December 1987). "Conduction aphasia and arcuate fasciculus". Acta Neurol. Scand. 76 (6): 422–7. doi:10.1111/j.1600-0404.1987.tb03597.x. PMID 3434200.
- ↑ Shuren JE, Schefft BK, Yeh HS, Privitera MD, Cahill WT, Houston W (September 1995). "Repetition and the arcuate fasciculus". J. Neurol. 242 (9): 596–8. doi:10.1007/BF00868813. PMID 8551322.
- 1 2 3 4 5 6 Anderson JM, Gilmore R, Roper S, et al. (October 1999). "Conduction aphasia and the arcuate fasciculus: A reexamination of the Wernicke-Geschwind model". Brain Lang. 70 (1): 1–12. doi:10.1006/brln.1999.2135. PMID 10534369.
- 1 2 "Conduction Aphasia". www.asha.org. Retrieved 2015-11-13.
- ↑ Bakheit AM, Shaw S, Carrington S, Griffiths S (October 2007). "The rate and extent of improvement with therapy from the different types of aphasia in the first year after stroke". Clin Rehabil. 21 (10): 941–9. doi:10.1177/0269215507078452. PMID 17981853.
- 1 2 Kohn, Susan E. (1992). Conduction aphasia. Hillsdale, N.J: L. Erlbaum. pp. 25–26. ISBN 0-8058-0681-4.
- ↑ Kohler K, Bartels C, Herrman M, et al. (October 1998). "Conduction aphasia--11 classic cases". Aphasiology. 12 (10): 865–884. doi:10.1080/02687039808249456.
- ↑ Kohn, Susan E. (1992). Conduction aphasia. Hillsdale, N.J: L. Erlbaum. pp. 28–29. ISBN 0-8058-0681-4.
- ↑ Feinberg TE, Gonzalez Rothi LJ, Heilman KM (June 1986). "'Inner speech' in conduction aphasia". Arch. Neurol. 43 (6): 591–3. doi:10.1001/archneur.1986.00520060053017. PMID 3718287.
Further reading
- Hickok G, Buchsbaum B, Humphries C, Muftuler T (July 2003). "Auditory-motor interaction revealed by fMRI: speech, music, and working memory in area Spt". J Cogn Neurosci. 15 (5): 673–82. doi:10.1162/089892903322307393. PMID 12965041.
- Hickok G, Poeppel D (2004). "Dorsal and ventral streams: a framework for understanding aspects of the functional anatomy of language". Cognition. 92 (1-2): 67–99. doi:10.1016/j.cognition.2003.10.011. PMID 15037127.
- Baldo JV, Klostermann EC, Dronkers NF (May 2008). "It's either a cook or a baker: patients with conduction aphasia get the gist but lose the trace". Brain Lang. 105 (2): 134–40. doi:10.1016/j.bandl.2007.12.007. PMID 18243294.
- Carlson, Neil R.; Heth, C. Donald (2007). Psychology the science of behaviour (4th ed.). Pearson Education Inc. ISBN 0-205-64524-0.
- Sidiropoulos Kyriakos; Ackermann Hermann; Wannke Michael; Ingo Hertrich (August 2010). "Temporal processing capabilities in repetition conduction aphasia". J Brain and Cognition. 73 (3): 194–202. doi:10.1016/j.bandc.2010.05.003. PMID 20621742.
External links
- Aphasia Center of California in Oakland, CA, U.S.