Babesia
| Babesia[1][2] | |
|---|---|
 | |
| Scientific classification | |
| Domain: | Eukaryota |
| (unranked): | SAR |
| (unranked): | Alveolata |
| Phylum: | Apicomplexa |
| Class: | Aconoidasida |
| Order: | Piroplasmida |
| Family: | Babesiidae |
| Genus: | Babesia |
| Species | |
|
Babesia bigemina | |
Babesia (also called Nuttallia)[3] is a genus of protozoan apicomplexan piroplasms that infect the blood and cause a parasitic, hemolytic disease known as babesiosis. Originally discovered by the Romanian bacteriologist Victor Babeș, over 100 species of Babesia have been identified, but only a few have been documented to be pathogenic in humans.[4]
In the United States, B. microti is the most common strain associated with humans. Other species infect cattle, livestock, and occasionally domestic animals.[5][6] People who contract babesiosis suffer from malaria-like symptoms. As a result, malaria is a common misdiagnosis for the disease.
Classification
Babesia is a protozoan parasite of which B. microti and B. divergens are the two species most frequently found to infect humans. Infections from other species of Babesia have been documented in humans, but are not regularly seen. Babesiosis is also known as piroplasmosis.[5] Due to historical misclassifications, this protozoan was labeled with many names that are no longer used. Common names of the disease include Texas cattle fever, redwater fever, tick fever, and Nantucket fever.[6]
Genomics
Although it was initially reported that the mitochondrial genome is circular unlike other sequenced Apicomplexa mitochondrial genomes, this has now been revised. The mitochondrial genome is actually linear.[7]
Partial RNA sequencing of canine piroplams has identified a number of additional species.
The genome of B. microti has been sequenced.[8] The sequence shows that this species does not belong to the either of the established genera — Babesia and Theileria — but instead belongs to a separate genus.
History
For centuries, babesiosis was known to be a serious illness for wild and domesticated animals, especially cattle. Victor Babeș, who first documented the disease in Romania in 1888, described symptoms of a severe hemolytic illness seen uniquely in cattle and sheep.[6][9] Although he identified the causative agent in 1888, he incorrectly believed it to be due to the bacterium he named Haematococcus bovis.
In 1893, Americans Theobald Smith and Fred Kilborne identified the parasite as the cause of Texas cattle fever, the same disease described by Babeș. Smith and Kilborne also identified the tick as the agent of transmission, a discovery that first introduced the concept of arthropods functioning as disease vectors.[10] Long believed to be a disease that only affected nonhuman mammals, the first case of babesiosis was seen in humans in 1957.[5] The first case was observed in a splenectomized patient (as were all people diagnosed with the infection until 1969). The first case of babesiosis seen in a nonsplenectomized patient proved the protozoan parasite was a potential pathogen in anyone.[11]
Clinical presentation
The severity of B. microti infections varies. For 25% of cases in adults and 50% of cases in children, the disease is asymptomatic or mild with flu-like symptoms. In other cases, symptoms are characterized by irregular fevers, chills, headaches, general lethargy, pain, and malaise.[5] In severe cases, hemolytic anemia, jaundice, shortness of breath, and hemoglobinuria are documented due to the lytic effects of parasitic multiplication.[6][12] Immunocompetent individuals with healthy spleens often recover without treatment.[5] Splenectomized patients are more susceptible to contracting the disease and the course of infection often ends fatally within five to eight days of symptom onset.[13] Parasitemia levels can reach up to 85% in patients without spleens compared to 1–10% in individuals with spleens and effective immune systems. Splenectomized patients suffer from severe hemolytic anemia with occasional incidences of hepatomegaly and splenomegaly documented.[12]
Complications arising from B. microti infections include acute respiratory failure, congestive heart failure, and renal failure. Infections can be fatal in 5-10% of hospitalized patients, with increased risk of death in the immunosuppressed, the elderly, and those coinfected with Lyme disease.[12] B. divergens infections have a much higher fatality rate (42%) and present with more severe symptoms. Infected individuals suffer from hemoglobinuria followed by jaundice, a persistently high fever, chills, and sweats. If left untreated, B. divergens infections can develop into shock-like symptoms with pulmonary edema and renal failure.[12]
Signs of infection usually arise one to eight weeks after a bite from an infectious tick.[13] Infections from B. divergens have a shorter latent period, usually ranging from one to three weeks.[12]
Bovine babesiosis caused by B. bovis remains an important constraint for the development of cattle industries worldwide. Effective control can be achieved by vaccination with live attenuated phenotypes of the parasite. However, these vaccines have a number of drawbacks, which justifies the search for better, safer vaccines. In recent years, a number of parasite proteins with immunogenic potential have been discovered. Through polymerase chain reaction, genetic sequencing, and bioinformatics analysis of the genes, a high degree of conservation (98-100%) was found among Brazilian isolates of B. bovis and the T2Bo isolate. Thus, these genes are worth considering as viable candidates to be included in a recombinant cocktail vaccine for cattle babesiosis caused by B. bovis.
Transmission
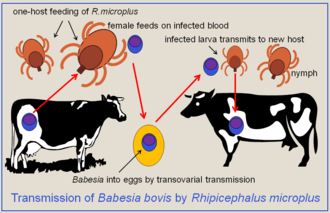
Babesia species are spread through the saliva of a tick when it bites. At its nymphal stage, a tick bites into the skin for a blood meal. The tick, if not removed, stays attached for three to four days, with longer periods of feeding associated with a higher probability of acquiring the parasite. The parasite can survive in the tick as it molts through its various developmental stages, resulting in all stages being potentially infectious. Some species of Babesia can be transmitted from a female tick to its offspring before migrating to salivary glands for feeding.[5] B. microti, the most common species in humans, though, has not been shown to transmit transovarially.[4] Ticks of domestic animals that transmit Babesia, causing much disease, include the very widespread cattle ticks, Rhipicephalus (Boophilus) microplus, and R.(B.) decoloratus. These ticks have a strict one-host feeding cycle on cattle, so the Babesia can only be transmitted by the transovarial route.
In the Americas, Ixodes scapularis is the most common vector. This hard tick, commonly known as a deer tick, is also the vector for other tick-associated illnesses, such as Lyme disease. Many species of Babesia only infect nonhuman mammalian hosts, most commonly cattle, horses, and sheep. B. microti and B. divergens are the two main pathogenic species in humans. Their reservoirs are theorized to be the white-footed mouse (Peromyscus leucopus), microtus voles (Microtus spp.), and the white-tailed deer (Odocoileus virginianus).[14] These woodland species are hypothesized reservoirs because although they are known to harbor the disease, complete reservoir competence has not yet been shown.[15]
Most cases of transmission between humans are attributed to a tick vector. As of 2003, though, the Centers for Disease Control and Prevention (CDC) acknowledged more than 40 cases of babesiosis contracted from packed red blood cell (PRBC) transfusions and two infections documented from organ transplantation. PRBC transfusions that cause infections were identified through testing of the blood donor for B. microti antibodies.[16] The occurrence of PRBC transfusions as a mechanism of Babesia transmission puts pressure on governmental organizations, such as the CDC, to heighten standard measures for screening blood donations.
Adaptations of Babesia and Rise of Genetic Diversity
Babesia show host specificity, allowing many different subspecies of Babesia to emerge, each infecting a different kind of vertebrae organism.[17] Interestingly, while the different subspecies, such as B. bovis and Babesia bigemina prefer to infect cattle in tropical environments, they are capable of infecting other animals, such as the white-tailed deer.[17] Therefore, while the organism has the capacity to display host specificity, and thus increase transmission effectiveness, it can also infect a variety of hosts.[17]
The process by which Babesia achieves this is through mutations and natural selection. As the protozoa exposes itself to different environments, individuals within the population may develop mutations that increase their fitness within the current environment. These individuals exhibit greater fitness and thus the population evolves to increase their numbers. This also explains why there is such great genetic diversity for this organism.[17]
Babesia persists long-term in the host's system and maintains a selfish relationship with it: the host gains no benefit from the parasite invasion but rather suffers by being infected. This allows the parasite to exploit all of the resources offered by the host, allowing it to increase in number, and eventually increase rate of transmission.[17] Too lethal of an infection would result in the death of the host resulting in the parasite being unable to spread, which would ultimately be seen as a loss from an evolutionary standpoint.[17] Different species of Babesia are able to withstand the stress of the host's immune system. Infection typically stimulates the innate, and not humoral, immune system.[17] This results in control of the infection, but not clearance, allowing the organism to persist.[17]
Morphology
Babesia species enter red blood cells (erythrocytes) at the sporozoite stage. Within the red blood cell, the protozoa become cyclical and develop into a trophozoite ring. The trophozoites moult into merozoites, which have a tetrad structure coined a Maltese-cross form.[18] The tetrad morphology, which can be seen with Giemsa staining of a thin blood smear, is unique to Babesia, and serves as a distinguishing feature from Plasmodium falciparum, a protozoan of similar morphology that causes malaria. Trophozoite and merozoite growth ruptures the host erythrocyte, leading to the release of vermicules, the infectious parasitic bodies, which rapidly spread the protozoa throughout the blood.[5]
Lifecycle
The lifecycle of B. microti, which is typical of parasites in that genus, requires a biological stage in a rodent or deer host, and is transmitted by ticks of the family Ixodidae between these hosts. To begin, the ticks introduce the sporozoites into the host when taking a blood meal. Sporozoites enter erythrocytes in the blood and begin the cyclical development between trophozoites and merozoites. Rather than producing more trophozoites, some merozoites produce gametocytes. The tick definitive host takes up the gametocytes when attached for a blood meal. The gametes are fertilized in the gut of the tick and develop into sporozoites in the salivary glands. The sporozoites are introduced into a human upon inoculation at the bite of an infected tick. Even as an incidental host, the phase changes which occur in the parasite are the same within humans as in the biological hosts. Babesia can be diagnosed at the trophozoite stage, and can be transmitted from human to human either through the tick vector or through blood transfusions.[4]

Patterns of incidence
Influence of increasing temperature
In the past, it was noticed that the emergence of tick-borne diseases coincided with climate change, but it is questionable whether or not climate change is a cause of the emergence.[19] After much data collection, a correlation was found between climate change and the incidence of tick-borne diseases.[19] However, the correlation is not strong enough to outright claim that climate change is a major factor of the increasing prevalence of tick-borne diseases.[19]
Influence of the environment
High environmental temperature, humidity and rainfall have been correlated with fostering a more accommodating environment for the ticks carrying Babesia.[20] This may explain why B. bigemina infection in cattle in the hilly region of Meghalaya has increased.[20] It has also been noted that the life span and number of generations of Babesia microplus are affected by the climate, as warm weather has been correlated with increasing the longevity of larvae and number of annual generations.[20] However, it is important to acknowledge what type of warm weather pertains to this claim. Dry warm weather results in interference with the life cycle of Babesia within the tick, and cold weather completely interrupts transmission.[21] Warm, wet weather increases the intensity of infestation- the population is able to better able to thrive due to the relatively fluid environment being more accommodating by making water and nutrients more accessible.[21]
Diagnosis and treatment
Diagnostic tests
As a protozoan parasite, the most effective way to identify Babesia infection is through blood sample testing. It is important to pay specific attention to particular morphologies of Babesia in blood smears because its substantial similarity to the malarial parasite Plasmodium falciparum results in many patients suffering from babesiosis being misdiagnosed. The few distinguishing factors for Babesia include protozoa with varying shapes and sizes, the potential to contain vacuoles, and the lack of pigment production. Trophozoites within an erythrocyte that appear in a tetrad formation are also indicative of Babesia. A trained eye is necessary to distinguish the two species.
Even with much study of babesiosis and malaria, misdiagnosis with blood smear can be frequent and problematic. To supplement a blood smear, diagnoses should be made with an indirect fluorescent antibody (IFA) test. IFA testing has a much higher specificity than stained blood smears with antibody detection in 88-96% of infected patients.[4] Diagnostic measures through antibody testing are also particularly useful for identifying serum prevalence in asymptomatic individuals. Due to the transmissibility of Babesia through blood transfusions, IFA testing would be an effective means of screening for the disease in blood donations.
Historically, babesiosis diagnosis was carried out with xenodiagnosis in hamsters for B. microti and in gerbils for B.divergens.[5] While successful at identifying the disease, this diagnostic technique has been abandoned for faster diagnostic measures.
Treatment
Several methods are available to manage and treat babesiosis in animals. In many cases, patients spontaneously recover, having only experienced mild symptoms undiagnosed as the disease. This occurrence is almost always seen in B. microti infections, which are generally more common in the United States. For B. divergens and more severe B. microti infections, the standard treatment historically for symptomatic individuals was oral or intravenous clindamycin with oral quinine.[4] With the results of research completed in 2000, however, treatment regimens have been increasingly leaning towards oral atovaquone with oral azithromycin. The latter medications are preferred, as they are equally effective in all but the most severe cases and exhibit fewer associated adverse reactions.[22] In severe cases, blood exchange transfusions have been performed to lower the parasitic load in the individual.[5] Other rudimentary treatment measures include addressing and correcting abnormal clinical signals.[6]
Epidemiology
Of the species to infect humans, B. microti is most common in the Americas, whereas B. divergens is the predominant strain found in Europe. Endemic areas are regions of tick habitat, including the forest regions of the northeastern United States and temperate regions of Europe.[13] Ixodidae, the tick vectors of B. microti, also transmit the better-known Borrelia burgdorferi, causative agent of Lyme disease. For reasons that remain unclear, in areas endemic to both Lyme disease and babesiosis, Lyme disease transmission prevails and is more predominant in the region.[5] Prevalence of babesiosis in malaria-endemic regions remains unknown due to the likelihood of misdiagnosis as malaria.[12] As the disease results in a high number of asympomatic individuals, many populations can possess high seroprevalence without much documentation of illness. For example, in Rhode Island and Nantucket, seroprevalence has been measured to be 20-25%.[5] Prevalence of babesiosis is mostly documented during the months of May to September when tick activity in endemic regions is high.[13]
Prevention
The most effective public health measure for Babesia is avoidance of tick exposure. This can be performed through personal prevention strategies such as avoiding tick-infested areas (especially during high tick season between May and September), remaining covered with light clothing, searching for ticks after being outdoors, and removing discovered ticks from the skin.[12] Other preventive measures include applying diethyltoluamide (DEET), a common repellent that is effective against ticks and insects. (For people who react adversely to DEET, alternative insect repellents should be used.) On a state level, if health departments are particularly motivated, tick elimination is a possibility. In 1906, efforts were made to eradicate the tick vector of the bovine disease form of babesiosis in the United States. This eradication was recorded as being successfully completed four decades later.[6] Complete eradication efforts would be a long-term project, which would significantly reduce the prevalence of both babesiosis and Lyme disease. However, as public health departments are often short on funding, preventive measures seem to be more recommended over vector control. Due to the relatively low prevalence of the disease and the presence of several reservoirs, babesiosis is currently not a candidate for vaccine-based prevention. In regions where ticks of domestic animals are routinely controlled with chemical acaricides to reduce incidence of infection with B. bovis and B. bigemina, the risk to humans from these parasites will be reduced.
References
- ↑ Khayat, Abeer; Rathore, Mobeen (2008). "Ch. 36: Babesia Species". In Barton, Leslie L.; Volpe, J.J.; Friedman, Neil R. The Neurological Manifestations of Pediatric Infectious Diseases and Immunodeficiency Syndromes. Humana Press. pp. 343–6. ISBN 978-1-59745-391-2.
- ↑ "Babesia". NCBI Taxonomy Browser. 5864.
- ↑ Nowell, Frank (November 1969). "The blood picture resulting from Nuttallia (= Babesia) rodhaini and Nuttallia (= Babesia) microti infections in rats and mice". Parasitology. 59 (4): 991–1004. doi:10.1017/S0031182000070475.
- 1 2 3 4 5 DPDx: Laboratory Identification of Parasites of Public Health Concern. Babesiosis. CDC. Retrieved on 2009-03-05.
- 1 2 3 4 5 6 7 8 9 10 11 Despommier, Dickson D. (1995). Parasitic Diseases (3rd ed.). Springer-Verlag. pp. 224–6. ISBN 978-0-387-94223-0.
- 1 2 3 4 5 6 Ristic, Miodrag; Ambroise-Thomas, Pierre; Kreier, Julius P. (1984). Malaria and Babesiosis: Research Findings and Control Measures. New Perspectives in Clinical Microbiology. 7. M. Nijhoff. pp. 100–170. ISBN 978-0-89838-675-2. OCLC 709342375.
- ↑ Cornillot E, Dassouli A, Garg A, et al. (2013). "Whole genome mapping and re-organization of the nuclear and mitochondrial genomes of Babesia microti isolates". PLoS ONE. 8 (9): e72657. doi:10.1371/journal.pone.0072657. PMC 3762879
 . PMID 24023759.
. PMID 24023759. - ↑ Cornillot E, Hadj-Kaddour K, Dassouli A, et al. (October 2012). "Sequencing of the smallest Apicomplexan genome from the human pathogen Babesia microti". Nucleic Acids Res. 40 (18): 9102–14. doi:10.1093/nar/gks700. PMC 3467087
 . PMID 22833609.
. PMID 22833609. - ↑ Vannier E, Krause PJ (June 2012). "Human babesiosis". N. Engl. J. Med. 366 (25): 2397–407. doi:10.1056/NEJMra1202018. PMID 22716978.
- ↑ Schultz, Myron (December 2008). "Photo Quiz: Theobald Smith". Emerg Infect Dis. 14 (12): 1939. doi:10.3201/eid1412.081188. ISSN 1080-6059.
- ↑ Beaver, P.C.; Jung, R.C.; Cupp, E.W.; Craig, C.F. (1984). Clinical parasitology (9th ed.). Lea & Febiger. pp. 205–8. ISBN 978-0-8121-0876-7.
- 1 2 3 4 5 6 7 Gelfand, Jeffrey A.; Vannier, Edouard. "Ch. 204: Babesiosis". Harrison's Principles of Internal Medicine, 17e. McGraw-Hill’s Access Medicine.
- 1 2 3 4 Babesiosis National Institute of Allergy and Infectious Diseases, National Institutes of Health.
- ↑ Karbowiak G (2004). "Zoonotic reservoir of Babesia microti in Poland". Pol. J. Microbiol. 53 Suppl: 61–5. PMID 15787199.
- ↑ Telford SR, Spielman A (January 1993). "Reservoir competence of white-footed mice for Babesia microti". J. Med. Entomol. 30 (1): 223–7. doi:10.1093/jmedent/30.1.223. PMID 8433329.
- ↑ Lux JZ, Weiss D, Linden JV, et al. (January 2003). "Transfusion-associated babesiosis after heart transplant". Emerging Infect. Dis. 9 (1): 116–9. doi:10.3201/eid0901.020149. PMC 2873739
 . PMID 12533293.
. PMID 12533293. - 1 2 3 4 5 6 7 8 Chauvin, Alain; Moreau, Emmanuelle; Bonnet, Sarah; Plantard, Olivier; Malandrin, Laurence (21 April 2009). "Babesia and its hosts: adaptation to long-lasting interactions as a way to achieve efficient transmission". Veterinary Research. 40 (2): 1–18. doi:10.1051/vetres/2009020.
- ↑ Herwaldt BL, Cacciò S, Gherlinzoni F, et al. (August 2003). "Molecular characterization of a non-Babesia divergens organism causing zoonotic babesiosis in Europe". Emerging Infect. Dis. 9 (8): 942–8. doi:10.3201/eid0908.020748. PMC 3020600
 . PMID 12967491.
. PMID 12967491. Figure 2. Panel of computer-generated electronic images of photomicrographs of Babesia-infected erythrocytes on a Giemsa-stained smear of peripheral blood...
- 1 2 3 Randolph, S.E. (2004). "Evidence that climate change has caused 'emergence' of tick-borne diseases in Europe?". International Journal for Medical Microbiology. 293: 5–15. PMID 15146980.
- 1 2 3 Laha, Ramgopal; M. Das; A. Sen (2015). "Morphology, epidemiology, and phylogeny of Babesia: An overview". Tropical Parasitology. 5 (2): 94.
- 1 2 Quintão-Silva, Maria G (December 2003). "Infection rate of Babesia spp. sporokinetes in engorged Boophilus microplus from an area of enzootic stability in the State of Minas Gerais, Brazil". Mem. Inst. Oswaldo Cruz. 98 (8).
- ↑ Krause PJ, Lepore T, Sikand VK, et al. (November 2000). "Atovaquone and azithromycin for the treatment of babesiosis". N. Engl. J. Med. 343 (20): 1454–8. doi:10.1056/NEJM200011163432004. PMID 11078770.
External links
- Lyme and Tick-Borne Diseases Research Center: Babesiosis
- "Babesiosis Fact Sheet". Connecticut Department of Public Health.
- "Babesiosis". New York State Department of Health.
- "Babesia". Centers for Disease Control and Prevention.
- "Babesiosis". Laboratory Identification of Parasites of Public Health Concern. DPDx: CDC.
- "Babesia". NCBI Taxonomy Browser. 5864.