Fibroadenoma
| Fibroadenoma | |
|---|---|
.jpg) | |
| Histopathologic image of breast fibroadenoma. Core needle biopsy. Hematoxylin & eosin stain. | |
| Classification and external resources | |
| Specialty | Gynecology |
| ICD-10 | D24 |
| ICD-9-CM | 217 |
| ICD-O | M9010/0-M9012, M9020, M9030 |
| DiseasesDB | 1595 |
| MedlinePlus | 007216 |
| eMedicine | radio/109 |
| MeSH | D018226 |
Fibroadenomas of the breast are benign tumors characterized by an admixture of stromal and epithelial tissue. Since both fibroadenomas and breast cancer can appear as similar lumps, it is currently recommended to perform ultrasound analyses and possibly tissue sampling with subsequent histopathologic analysis in order to perform diagnosis. Unlike typical lumps from breast cancer, fibroadenomas are easy to move, with clearly defined edges.[1][2]
Fibroadenomas are sometimes called breast mice or a breast mouse owing to their high mobility in the breast.[3]
Signs and symptoms
The typical case is the presence of a painless, firm, solitary, mobile, slowly growing lump in the breast of a woman of child-bearing years.[2][4][5]
In the male breast, fibroepithelial tumors are very rare, and are mostly phyllodes tumors. Exceptionally rare case reports exist of fibroadenomas in the male breast, however these cases may be associated with antiandrogen treatment.[6]
Cause
Fibroadenomas are partially hormone-related and frequently regress after menopause.
Higher intake of fruits and vegetables, higher number of live births, use of oral contraceptives and moderate exercise are associated with lower frequency of fibroadenomas.[7]
Histopathology

Fibroadenomas arise in the terminal duct lobular unit of the breast.
Cytology
The diagnostic findings on needle biopsy consist of abundant stromal cells, which appear as bare bipolar nuclei, throughout the aspirate; sheets of fairly uniform-size epithelial cells that are typically arranged in either an antler-like pattern or a honeycomb pattern. These epithelial sheets tend to show typical metachromatic blue staining on DiffQuick staining. Foam cells and apocrine cells may also be seen, although these are less diagnostic features.[4][8] The gallery images below demonstrate these features.
Cellular fibroadenoma, also known as juvenile fibroadenoma, is a variant type of fibroadenoma with increased stromal cellularity.[9][10]
Macroscopic
Approximately 90% of fibroadenomas are less than 3 cm in diameter. However, these tumors have the potential to grow reaching a remarkable size, particularly in young individuals. The tumor is round or ovoid, elastic, and nodular, and has a smooth surface. The cut surface usually appears homogenous and firm, and is grey-white or tan in colour. The pericanalicular type (hard) has a whorly appearance with a complete capsule, while the intracanalicular type (soft) has an incomplete capsule.[8]
Microscopic
Fibroadenoma of the breast is a benign tumor composed of a biphasic proliferation of both stromal and epithelial components that can be arranged in two growth patterns: pericanalicular (stromal proliferation around epithelial structures) and intracanalicular (stromal proliferation compressing the epithelial structures into clefts).
These tumors characteristically display hypovascular stroma compared to malignant neoplasms.[2][5][8] Furthermore, the epithelial proliferation appears in a single terminal ductal unit and describes duct-like spaces surrounded by a fibroblastic stroma. The basement membrane is intact.[11]
Molecular pathology
Up to 66% of fibroadenomas harbor somatic mutations in the exon 2 of the mediator complex subunit 12 (MED12) gene. In particular, these mutations are restricted to the stromal component.[12][13]
Diagnosis
A fibroadenoma is usually diagnosed through clinical examination, ultrasound or mammography, and often a needle biopsy sample of the lump.[4]
.jpg) Fibroadenoma Histology (H&E). The image demonstrates intracanalicular morphology (top right) and pericanalicular morphology (bottom left)
Fibroadenoma Histology (H&E). The image demonstrates intracanalicular morphology (top right) and pericanalicular morphology (bottom left)_DG_stain.jpg) Fibroadenoma, Fine Needle Aspiration Biopsy (Giemsa or DiffQuickTM stain). The image shows abundant bare bipolar stromal nuclei surrounding sheets of metachromatic epithelial cells.
Fibroadenoma, Fine Needle Aspiration Biopsy (Giemsa or DiffQuickTM stain). The image shows abundant bare bipolar stromal nuclei surrounding sheets of metachromatic epithelial cells._PAP_stain.jpg) Fibroadenoma, Fine Needle Aspiration Biopsy (Papanicolou stain). The image shows a sheet of epithelial cells in the typical antler pattern.
Fibroadenoma, Fine Needle Aspiration Biopsy (Papanicolou stain). The image shows a sheet of epithelial cells in the typical antler pattern..jpg) Histopathologic image of breast fibroadenoma. Core needle biopsy. Hematoxylin & eosin stain.
Histopathologic image of breast fibroadenoma. Core needle biopsy. Hematoxylin & eosin stain. Histopathologic image of breast fibroadenoma showing proliferation of intralobular stroma compressing and distorting the epithelium. H&E stain.
Histopathologic image of breast fibroadenoma showing proliferation of intralobular stroma compressing and distorting the epithelium. H&E stain.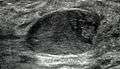 Fibroadenoma in ultrasound
Fibroadenoma in ultrasound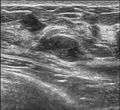
















Treatment
Most fibroadenomas are left in situ and monitored by a doctor, or the patient in question. Some are treated by surgical excision. They are removed with a small margin of normal breast tissue if the preoperative clinical investigations are suggestive of the diagnosis. A small amount of normal tissue must be removed in case the lesion turns out to be a phyllodes tumour on microscopic examination.[8][14]
Because needle biopsy is often a reliable diagnostic investigation, some doctors may decide not to operate to remove the lesion, and instead opt for clinical follow-up to observe the lesion over time using clinical examination and mammography to determine the rate of growth, if any, of the lesion. A growth rate of less than sixteen percent per month in women under fifty years of age, and a growth rate of less than thirteen percent per month in women over fifty years of age have been published as safe growth rates for continued non-operative treatment and clinical observation.[15]
Some fibroadenomas respond to treatment with ormeloxifene.[16]
Fibroadenomas have not been shown to recur following complete excision or transform into phyllodes tumours following partial or incomplete excision.[8]
There are also natural treatments being touted to diminish fibroadenomas, such as Fibrosolve, but no definite studies have been made as to prove their effectiveness.
Cryoablation
The FDA has approved cryoablation of a fibroadenoma as a safe, effective and minimally-invasive alternative to open surgical removal in 2001.[17] In the procedure, ultrasound imaging is used to guide a probe into the mass of breast tissue. Extremely cold temperatures are then used to destroy the abnormal cells,[18] and over time the cells are reabsorbed into the body. The procedure can be performed in an office setting with local anesthesia only, and leaves substantially less scarring than open surgical procedures and no breast tissue deformation.[18]
The American Society of Breast Surgeons recommends the following criteria to establish a patient as a candidate for cryoablation of a fibroadenoma:[17]
- The lesion must be sonographically visible.
- The diagnosis of fibroadenoma must be confirmed histologically.
- Lesions should be less than 4 cm in diameter.
Ultrasound
This method is non-invasive and relies on tissue heating to destroy fibroadenoma cells. Focused ultrasounds have been used to treat other benign tumors, such as fibroid disease in the uterus.[19]
Epidemiology
They are the most common breast tumor in adolescent women. They also occur in a small number of post-menopausal women. Their incidence declines with increasing age, and, in general, they appear before the age of thirty years.
External links
References
- ↑ 22-251c.Fibroadenomas at Merck Manual of Diagnosis and Therapy Home Edition
- 1 2 3 Tavassoli, F.A.; Devilee, P., eds. (2003). World Health Organization Classification of Tumours: Pathology & Genetics: Tumours of the breast and female genital organs. Lyon: IARC Press. ISBN 92-832-2412-4.
- ↑ Dirbas, Fredrick M.; Scott-Conner, Carol E.H., eds. (2010). Breast surgery office management and surgical techniques. New York: Springer. p. 71. ISBN 978-1-4419-6075-7.
- 1 2 3 DeMay, M. Practical Principles of Cytopathology (Revised ed.). ASCP Press. p. 2007. ISBN 0-89189-549-3.
- 1 2 Pathology Outlines Website. Accessed 12 February 2009.
- ↑ Shin SJ, Rosen PP (July 2007). "Bilateral presentation of fibroadenoma with digital fibroma-like inclusions in the male breast". Arch. Pathol. Lab. Med. 131 (7): 1126–9. doi:10.1043/1543-2165(2007)131[1126:BPOFWD]2.0.CO;2. PMID 17617003.
- ↑ Nelson, Z. C.; Ray, R. M.; Wu, C.; Stalsberg, H.; Porter, P.; Lampe, J. W.; Shannon, J.; Horner, N.; Li, W.; Wang, W.; Hu, Y.; Gao, D.; Thomas, D. B. (2010). "Fruit and Vegetable Intakes Are Associated with Lower Risk of Breast Fibroadenomas in Chinese Women". Journal of Nutrition. 140 (7): 1294–1301. doi:10.3945/jn.109.119719. PMC 2884330
 . PMID 20484549.
. PMID 20484549. - 1 2 3 4 5 Rosen, PP. Rosen's Breast Pathology (3rd ed.). ISBN 978-0-7817-7137-5.
- ↑ Fekete, P; Petrek J; Majmudar B; Someren A; Sandberg W. (May 1987). "Fibroadenomas with stromal cellularity. A clinicopathologic study of 21 patients". Arch Pathol Lab Med. 111 (5): 427–32. PMID 3032124.
- ↑ Nassar, Hind. "Cellular fibroadenoma of breast". Retrieved 14 January 2013.
- ↑ "Fibroadenoma of the breast". Retrieved 2007-12-15.
- ↑ Lim WK, Ong CK, Tan J, Thike AA, Ng CC, Rajasegaran V, Myint SS, Nagarajan S, Nasir ND, McPherson JR, Cutcutache I, Poore G, Tay ST, Ooi WS, Tan VK, Hartman M, Ong KW, Tan BK, Rozen SG, Tan PH, Tan P, Teh BT (Aug 2014). "Exome sequencing identifies highly recurrent MED12 somatic mutations in breast fibroadenoma". Nat Genet. 46 (8): 877–880. doi:10.1038/ng.3037. PMID 25038752.
- ↑ Piscuoglio S, Murray M, Fusco N, Marchiò C, Loo FL, Martelotto LG, Schultheis AM, Akram M, Weigelt B, Brogi E, Reis-Filho JS (Nov 2015). "MED12 somatic mutations in fibroadenomas and phyllodes tumours of the breast". Histopathology. 67 (5): 719–29. doi:10.1111/his.12712. PMID 25855048.
- ↑ Rosai, J. (2004). Rosai and Ackerman's Surgical Pathology (9th ed.). ISBN 0-323-01342-2.
- ↑ Gordon PB, Gagnon FA, Lanzkowsky L (October 2003). "Solid breast masses diagnosed as fibroadenoma at fine-needle aspiration biopsy: acceptable rates of growth at long-term follow-up". Radiology. 229 (1): 233–8. doi:10.1148/radiol.2291010282. PMID 14519878.
- ↑ Dhar, A.; Srivastava, A. (2007). "Role of Centchroman in Regression of Mastalgia and Fibroadenoma". World Journal of Surgery. 31 (6): 1178–1184. doi:10.1007/s00268-007-9040-4. PMID 17431715.
- 1 2 Management of Fibroadenomas of the Breast
- 1 2 WebMD — Cryotherapy Shrinks Benign Breast Lumps
- ↑ Jolesz, FA; Hynynen, K; McDannold, N; Tempany, C (August 2005). "MR imaging-controlled focused ultrasound ablation: a noninvasive image-guided surgery.". Magnetic resonance imaging clinics of North America. 13 (3): 545–60. doi:10.1016/j.mric.2005.04.008. PMID 16084419.
- http://www.medgadget.com/2012/12/theraclion-echopulse-ultrasound-therapy-for-breast-fibroadenomas-cleared-in-eu.html
- Jolesz FA, Hynynen K, McDannold N, Tempany C (2005). "MR imaging-controlled focused ultrasound ablation: a noninvasive image-guided surgery". Magn Reson Imaging Clin N Am. 13 (3): 545–60. doi:10.1016/j.mric.2005.04.008. PMID 16084419.
- Gombos EC, Kacher DF, Furusawa H, Namba K (2006). "Breast focused ultrasound surgery with magnetic resonance guidance". Top Magn Reson Imaging. 17 (3): 181–8. doi:10.1097/rmr.0b013e318033789f.
- Hynynen K, Pomeroy O, Smith DN, Huber PE, McDannold NJ, Kettenbach J, Baum J, Singer S, Jolesz FA (2001). "MR imaging-guided focused ultrasound surgery of fibroadenomas in the breast: a feasibility study". Radiology. 219: 176–185. doi:10.1148/radiology.219.1.r01ap02176.
- Marret H, Bleuzen A, Guérin A, Lauvin-Gaillard MA, Herbreteau D, Patat F, Tranquart F (Jan 2011). "French first results using magnetic resonance-guided focused ultrasound for myoma treatment". Gynecol Obstet Fertil. 39 (1): 12–20.