Gender differences in stroke care
This article describes disparities existing between men and women in accessing and receiving care for a stroke. This article also describes factors outside of the health-care system which contribute to this disparity.
Disparity in accessing care
Among patients greater than 50 years of age, women appear less likely than men to be admitted to the ICU.[1] Finally, women experience longer waiting times in the emergency department than men.[1]
Disparity in symptom recognition/diagnosis
There are marked differences in the clinical symptom presentation of stroke between men and women.[2]
Women who suffer an acute stroke are more likely to present with non-traditional and non-neurological stroke symptoms, for example chest pain and/or shortness of breath. More atypical symptoms in women may result in a delayed diagnosis, longer in-hospital delays, and less aggressive rt-PA treatment.[3]
Disparity in treatment
Research findings indicate that physicians treat women experiencing stroke less aggressively than they treat men experiencing stroke. Women with cardiovascular disease, as an example, are less frequently offered invasive procedures when compared with their male counterparts.[1]
The use of rt-PA (Recombinant Tissue Plasminogen Activator), a protein enzyme that helps break up blood clots, is a common treatment for stroke. Research indicates that women have between 22% to 30% lower odds of receiving rt-PA treatment for acute stroke than men.[3] When comparing the treatment of men and women with acute stroke, research has found that women are consistently less likely to receive thrombolytic (blood clot dissolving) treatments,[3] despite findings indicating that women experiencing stroke benefit more than men from thrombolytic treatment.[4]
Between 1997 and 2006, women hospitalized for acute ischemic stroke (AIS) were less likely to receive cerebro-vascular and cardiac reperfusion/revascularization therapies, intravenous tPA (Tissue Plasminogen Activator to break up clots), catheter angiography (imaging of blood vessels), angioplasty/stent (opening of blocked blood vessels), and carotid endarterectomy (surgical removal of plaque).[4]
Non health-system factors contributing to sex disparity
Wage Gap
Employed women earn less than men for the same work, in every field.[5] Women constitute nearly half of the workforce, comprise over half of all college and graduate degree recipients in the United States, and yet earn only 77 cents for every dollar earned by a man.11 Researchers attribute this 23 percent Gender pay gap, also known as the Glass ceiling, to three differentiated barriers. First, societal barriers such as stereotyping based on gender, second, internal barriers such as corporate climates, which impose rules and organizational cultures that are oppressive to female employees, and third, barriers by government agencies, which fail to audit, or evaluate the progress of women in the workplace.[6]
.[7]
Poverty
Women in the United States are disproportionately affected by poverty, or a relative lack of wages. According to findings by the Institute for Women’s Policy Research (IWPR), adult women, ages 18–64 years, made up .2 percent of individuals living below the poverty line at the start of the economic recession of 2008, compared to 10.1 percent of adult males.[7] And the poverty rate for female-headed households represented 31.4 percent of the population living below the poverty line in 2008.[7]
Employer-sponsored health insurance and the employment gap
Women do not access Health insurance in the United States at the rate of men because women are less likely to be employed than men, there are fewer women in the workforce than men, and women are more likely to work part-time than men.[8]
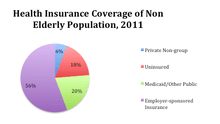
In the United States, the current standard for acquiring health coverage by an individual and their family is through a group plan made available by an employer.14 As of a 2011 study by the Kaiser Family Foundation, 55.8% of Americans access health[8] coverage through their employer, 20.5% depend on public programs such as Medicaid and Medicare, 5.7% access coverage through a private non-group, and the remaining 18% are uninsured.[9]
Even for those individuals who are covered by employer-based plans, women remain disproportionately underinsured, meaning that their medical expenses after insurance (and excluding Insurance) represent 10 percent or more of their incomes. Twelve percent of insured individuals, between the ages of 19 and 64, are underinsured, and of that group, women paid 16 percent of their income to health care costs, compared with 9 percent paid by men.[8]
Caretaking role
Women are also disproportionately impacted by unpaid work in the home.[7] Despite increased educational attainment, and growing numbers in the workforce over the past 60 years, women still spend more time contributing to unpaid household labor than men.[7] And while unemployed women contribute 50 percent more time to caregiving than employed women, rates of caregiving between employed and unemployed men, is negligible. The responsibility of Caregiver, and other household tasks, traditionally fall to women, however workplace standards have not adapted to the needs of women caregivers, with many workplaces maintaining strict limitations on Sick leave, Paid family leave, Flextime, and subsidized Child care, often causing women to leave their place of employment, and source of income, in search options which better accommodate their caregiving responsibilities.[7]
References
- 1 2 3 Kent, Jennifer A.; Patel, Vinisha; Varela, Natalie A. (September 2012). "Gender Disparities in Health Care". Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine. 79 (5): 555–559. doi:10.1002/msj.21336.
- ↑ Haast, Roy A M; Gustafson, Deborah R; Kiliaan, Amanda J (3 October 2012). "Sex differences in stroke". Journal of Cerebral Blood Flow & Metabolism. 32 (12): 2100–2107. doi:10.1038/jcbfm.2012.141.
- 1 2 3 Reeves, M.; Bhatt, A.; Jajou, P.; Brown, M.; Lisabeth, L. (19 February 2009). "Sex Differences in the Use of Intravenous rt-PA Thrombolysis Treatment for Acute Ischemic Stroke: A Meta-Analysis". Stroke. 40 (5): 1743–1749. doi:10.1161/STROKEAHA.108.543181.
- 1 2 Towfighi, Amytis; Markovic, Daniela; Ovbiagele, Bruce (November 2013). "Sex Differences in Revascularization Interventions after Acute Ischemic Stroke". Journal of Stroke and Cerebrovascular Diseases. 22 (8): e347–e353. doi:10.1016/j.jstrokecerebrovasdis.2013.03.018.
- ↑ "Women Earn Less Than Men for Same Work… No Matter What Field They Go Into". The Henry J. Kaiser Family Foundation. Retrieved 5 March 2014.
- ↑ Cabeza, Maria Florencia; Johnson, JB; Tyner, LJ (2011). "Glass Ceiling and Maternity Leave as Important Contributors to the Gender Wage Gap". Southern Journal of Business and Ethics. 3: 73–85.
- 1 2 3 4 5 6 Hartmann, H; English, A; Hayes, J (2010). "Women and men's employment and unemployment in the great recession". Institute for Women's Policy Research (Brief C373).
- 1 2 3 Patchias, E; Waxman, J (2007). "Women and Health Coverage: The Affordability Gap". The National Women's Law Center Issue Brief.
- ↑ "Health Insurance Coverage in America, 2011". The Henry J. Kaiser Family Foundation.