Lassa fever
| Lassa fever | |
|---|---|
| Lassa hemorrhagic fever | |
 | |
| Specialty | infectious disease |
| Symptoms | fever, headaches, bleeding[1] |
| Usual onset | 1–3 weeks following exposure[1] |
| Causes | Lassa virus[1] |
| Risk factors | exposure to rodents in West Africa[1] |
| Differential diagnosis | Ebola, malaria, typhoid[1] |
| Treatment | supportive, ribavirin[1] |
| Frequency | ~400,000 cases per year[2] |
| Deaths | ~5,000 deaths per year[2] |
Lassa fever, also known as Lassa hemorrhagic fever (LHF), is a type of viral hemorrhagic fever caused by the Lassa virus. Many of those infected by the virus do not develop symptoms. When symptoms occur they typically include fever, weakness, headaches, vomiting, and muscle pains. Less commonly there may be bleeding from the mouth or gastrointestinal tract. The risk of death once infected is about one percent and frequently occurs within two weeks of the onset of symptoms. Among those who survive about a quarter have deafness which improves over time in about half.[1]
The disease is usually initially spread to people via contact with the urine or feces of an infected multimammate rat. Spread can than occur via direct contact between people. Diagnosis based on symptoms is difficult. Confirmation is by laboratory testing to detect the viruses RNA, antibodies to the virus, or the virus itself in cell culture. Other conditions that may present similarly include Ebola fever, malaria, typhoid fever, and yellow fever. The Lassa virus is a member of the Arenaviridae virus family.[1]
There is no vaccine.[3] Prevention requires isolating those who are infected and decreasing contact with the rats. Efforts include having a cat to hunt vermin, and storing food in sealed containers. Treatment is directed at addressing dehydration and improving symptoms. The antiviral medication, ribavirin may be useful when given early. These measures improve outcomes.[1]
Descriptions of the disease date from the 1950s. The virus was first described in 1969 from a case in the town of Lassa, in Borno State, Nigeria.[1][4] Lassa fever occurs relatively commonly in West Africa including the countries of Nigeria, Liberia, Sierra Leone, Guinea, and Ghana.[1][2] There are about 300,000 to 500,000 cases which result in 5,000 deaths a year.[2]
Signs and symptoms
In 80% of cases, the disease is asymptomatic, but in the remaining 20%, it takes a complicated course. The virus is estimated to be responsible for about 5,000 deaths annually. The fever accounts for up to one-third of deaths in hospitals within the affected regions and 10 to 16% of total cases.[5]
After an incubation period of six to 21 days, an acute illness with multiorgan involvement develops. Nonspecific symptoms include fever, facial swelling, and muscle fatigue, as well as conjunctivitis and mucosal bleeding. The other symptoms arising from the affected organs are:
- Gastrointestinal tract
- Nausea
- Vomiting (bloody)
- Diarrhea (bloody)
- Stomach ache
- Constipation
- Dysphagia (difficulty swallowing)
- Hepatitis
- Cardiovascular system
- Pericarditis
- Hypertension
- Hypotension
- Tachycardia (abnormally high heart rate)
- Respiratory tract
- Cough
- Chest pain
- Dyspnoea
- Pharyngitis
- Pleuritis
- Nervous system
- Encephalitis
- Meningitis
- Unilateral or bilateral hearing deficit
- Seizures
Clinically, Lassa fever infections are difficult to distinguish from other viral hemorrhagic fevers such as Ebola and Marburg, and from more common febrile illnesses such as malaria.
The virus is excreted in urine for 3–9 weeks and in semen for three months.
Cause

Lassa virus is transmitted from animals, specifically it spreads to humans from a rodent known as a natal multimammate mouse (Mastomys natalensis).[6] This is probably the most common mouse in equatorial Africa, ubiquitous in human households and eaten as a delicacy in some areas.[6][7] It is also called the natal multimammate rat or African rat.
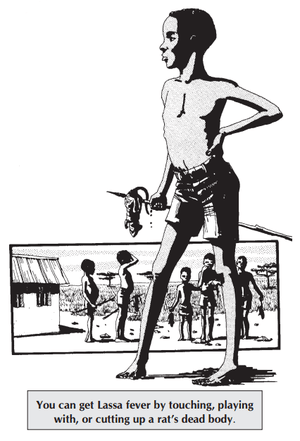
In these rodents, infection is in a persistent asymptomatic state. The virus is probably transmitted by contact with the feces or urine of animals accessing grain stores in residences.[7]
Infection in humans typically occurs by exposure to animal excrement through the respiratory or gastrointestinal tracts. Inhalation of tiny particles of infectious material (aerosol) is believed to be the most significant means of exposure. It is possible to acquire the infection through broken skin or mucous membranes that are directly exposed to infectious material. Transmission from person to person has also been established, presenting a disease risk for healthcare workers. The virus is still present in the urine for between three and nine weeks after infection, and it can be transmitted in semen for up to three months after becoming infected.[8][9]
Diagnosis
A range of laboratory investigations are performed, where possible, to diagnose the disease and assess its course and complications. An ELISA test for antigen and IgM antibodies give 88% sensitivity and 90% specificity for the presence of the infection. Other laboratory findings in Lassa fever include lymphopenia (low white blood cell count), thrombocytopenia (low platelets), and elevated aspartate aminotransferase levels in the blood. Lassa fever virus can also be found in cerebrospinal fluid.[10] In West Africa, where Lassa is most prevalent, it is difficult for doctors to diagnose due to the absence of proper equipment to perform tests.[11] In cases with abdominal pain, in countries where Lassa is common, Lassa fever is often misdiagnosed for example as appendicitis and intussusception which delays treatment with the antiviral ribavirin.[12]
Prevention
Control of the Mastomys rodent population is impractical, so measures are limited to keeping rodents out of homes and food supplies, as well as maintaining effective personal hygiene. Gloves, masks, laboratory coats, and goggles are advised while in contact with an infected person. These issues in many countries are monitored by a department of public health. In less developed countries, these types of organizations may not have the necessary means to effectively control outbreaks.
Researchers at the USAMRIID facility, where military biologists study infectious diseases, have a promising vaccine candidate.[13] They have developed a replication-competent vaccine against Lassa virus based on recombinant vesicular stomatitis virus vectors expressing the Lassa virus glycoprotein. After a single intramuscular injection, test primates have survived lethal challenge, while showing no clinical symptoms.[14]
Treatment
All persons suspected of Lassa fever infection should be admitted to isolation facilities and their body fluids and excreta properly disposed of.
Early and aggressive treatment using ribavirin was pioneered by Joe McCormick in 1979. After extensive testing, early administration was determined to be critical to success. Additionally, ribavirin is almost twice as effective when given intravenously as when taken by mouth.[15] Ribavirin is a prodrug which appears to interfere with viral replication by inhibiting RNA-dependent nucleic acid synthesis, although the precise mechanism of action is disputed.[16] The drug is relatively inexpensive, but the cost of the drug is still very high for many of those in West African states. Fluid replacement, blood transfusion, and fighting hypotension are usually required. Intravenous interferon therapy has also been used.
When Lassa fever infects pregnant women late in their third trimester, induction of delivery is necessary for the mother to have a good chance of survival.[17] This is because the virus has an affinity for the placenta and other highly vascular tissues. The fetus has only a one in ten chance of survival no matter what course of action is taken; hence, the focus is always on saving the life of the mother. Following delivery, women should receive the same treatment as other Lassa fever patients.
Work on a vaccine is continuing, with multiple approaches showing positive results in animal trials.
Prognosis
About 15-20% of hospitalized Lassa fever patients will die from the illness. The overall mortality rate is estimated to be 1%, but during epidemics, mortality can climb as high as 50%. The mortality rate is greater than 80% when it occurs in pregnant women during their third trimester; fetal death also occurs in nearly all those cases. Abortion decreases the risk of death to the mother.[18] Some survivors experience lasting effects of the disease,[19] and can include partial or complete deafness.[1]
Because of treatment with ribavirin, fatality rates are continuing to decline.
Epidemiology
Around 300,000 people are infected annually, with up to 5,000 deaths per year.[20]
It is relatively common in parts of West Africa where the multimammate rat is common, particularly Guinea (Kindia, Faranah and Nzerekore regions), Liberia (mostly in Lofa, Bong, and Nimba counties), Nigeria (everywhere) and Sierra Leone (typically from Kenema and Kailahun districts). It is present but less common in the Central African Republic, Mali, Senegal and other nearby countries, and less common yet in Ghana and the Democratic Republic of the Congo. Benin had its first confirmed cases in 2014, and Togo had its first confirmed cases in 2016.[8]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "Lassa fever". WHO. March 2016. Retrieved 2 November 2016.
- 1 2 3 4 Ogbu O, Ajuluchukwu E, Uneke CJ (2007). "Lassa fever in West African sub-region: an overview". Journal of vector borne diseases. 44 (1): 1–11. PMID 17378212.
Lassa fever is endemic in West Africa
- ↑ Yun, N. E.; Walker, D. H. (2012). "Pathogenesis of Lassa Fever". Viruses. 4 (12): 2031–2048. doi:10.3390/v4102031. PMC 3497040
 . PMID 23202452.
. PMID 23202452. - ↑ Frame JD, Baldwin JM, Gocke DJ, Troup JM (1 July 1970). "Lassa fever, a new virus disease of man from West Africa. I. Clinical description and pathological findings". Am. J. Trop. Med. Hyg. 19 (4): 670–6. PMID 4246571.
- ↑ Centers for Disease Control and Prevention, "Lassa Fever"
- 1 2 Richmond, J. K.; Baglole, D. J. (2003). "Lassa fever: Epidemiology, clinical features, and social consequences". BMJ. 327 (7426): 1271–1275. doi:10.1136/bmj.327.7426.1271. PMC 286250
 . PMID 14644972.
. PMID 14644972. - 1 2 Werner, Dietrich, editor (2004). Biological Resources and Migration. Springer. p. 363. ISBN 978-3-540-21470-0.
- 1 2 Public Health England: Lassa fever: origins, reservoirs, transmission and guidelines First published: 5 September 2014. Last updated: 1 April 2016
- ↑ "Lassa fever". Media Centre Fact Sheet No 179. World Health Organization. Retrieved 26 May 2015.
- ↑ Günther, S.; Weisner, B.; Roth, A.; Grewing, T.; Asper, M.; Drosten, C.; Emmerich, P.; Petersen, J.; Wilczek, M.; Schmitz, H. (2001). "Lassa Fever Encephalopathy: Lassa Virus in Cerebrospinal Fluid but Not in Serum". The Journal of Infectious Diseases. 184 (3): 345–349. doi:10.1086/322033. PMID 11443561.
- ↑ Asogun, D. A.; Adomeh, D. I.; Ehimuan, J.; Odia, I.; Hass, M.; Gabriel, M.; Olschläger, S.; Becker-Ziaja, B.; Folarin, O.; Phelan, E.; Ehiane, P. E.; Ifeh, V. E.; Uyigue, E. A.; Oladapo, Y. T.; Muoebonam, E. B.; Osunde, O.; Dongo, A.; Okokhere, P. O.; Okogbenin, S. A.; Momoh, M.; Alikah, S. O.; Akhuemokhan, O. C.; Imomeh, P.; Odike, M. A.; Gire, S.; Andersen, K.; Sabeti, P. C.; Happi, C. T.; Akpede, G. O.; Günther, S. (2012). Bausch, Daniel G, ed. "Molecular Diagnostics for Lassa Fever at Irrua Specialist Teaching Hospital, Nigeria: Lessons Learnt from Two Years of Laboratory Operation". PLoS Neglected Tropical Diseases. 6 (9): e1839. doi:10.1371/journal.pntd.0001839. PMC 3459880
 . PMID 23029594.
. PMID 23029594. - ↑ Dongo, A. E.; Kesieme, E. B.; Iyamu, C. E.; Okokhere, P. O.; Akhuemokhan, O. C.; Akpede, G. O. (2013). "Lassa fever presenting as acute abdomen: a case series". Virology Journal. 10: 124. doi:10.1186/1743-422X-10-123. PMC 3651342
 . PMID 23602143.
. PMID 23602143. - ↑ Preston, Richard (2002). The demon in the freezer: a true story. New York: Random House. ISBN 0-375-50856-2.
- ↑ Geisbert TW, Jones S, Fritz EA, et al. (2005). "Development of a New Vaccine for the Prevention of Lassa Fever". PLoS Med. 2 (6): e183. doi:10.1371/journal.pmed.0020183. PMC 1160587
 . PMID 15971954.
. PMID 15971954. - ↑ Fisher-Hoch SP, McCormick JB (2004). "Lassa fever vaccine". Expert review of vaccines. 3 (2): 189–97. doi:10.1586/14760584.3.4.S189. PMID 15056044.
- ↑ Crotty S, Cameron C, Andino R (2002). "Ribavirin's antiviral mechanism of action: lethal mutagenesis?". J. Mol. Med. 80 (2): 86–95. doi:10.1007/s00109-001-0308-0. PMID 11907645.
- ↑ Price ME, Fisher-Hoch SP, Craven RB, McCormick JB (September 1988). "A prospective study of maternal and fetal outcome in acute Lassa fever infection during pregnancy". BMJ. 297 (6648): 584–7. doi:10.1136/bmj.297.6648.584. PMC 1834487
 . PMID 3139220.
. PMID 3139220. - ↑ Centers for Disease Control and Prevention, "Lassa Fever, Signs and Symptoms"
- ↑ Emond, R. T.; Bannister, B.; Lloyd, G.; Southee, T. J.; Bowen, E. T. (1982). "A case of Lassa fever: Clinical and virological findings". British medical journal (Clinical research ed.). 285 (6347): 1001–1002. doi:10.1136/bmj.285.6347.1001. PMC 1500383
 . PMID 6812716.
. PMID 6812716. - ↑ Viral Hemorrhagic Fever Consortium Lassa fever Page accessed April 6, 2016
Further reading
- Garrett, Laurie. The coming plague: newly emerging diseases in a world out of balance. New York: Farrar, Straus and Giroux, 1994. ISBN 978-0140250916
- Lashley, Felissa R., and Jerry D. Durham. Emerging infectious diseases: trends and issues. New York: Springer Pub., 2002. ISBN 978-0826102508
| Classification | |
|---|---|
| External resources |