Lincomycin
 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a609005 |
| Pregnancy category |
|
| Routes of administration | IM/IV |
| ATC code | J01FF02 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | N/A |
| Biological half-life | 5.4 ± 1.0 hours after IM or IV administration |
| Excretion | renal and biliary |
| Identifiers | |
| |
| CAS Number |
154-21-2 |
| PubChem (CID) | 3000540 |
| DrugBank |
DB01627 |
| ChemSpider |
2272112 |
| UNII |
BOD072YW0F |
| KEGG |
D00223 |
| ChEBI |
CHEBI:6472 |
| ChEMBL |
CHEMBL1447 |
| ECHA InfoCard | 100.005.296 |
| Chemical and physical data | |
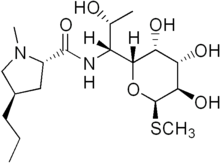
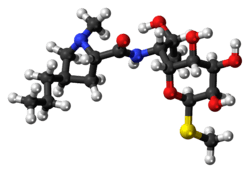
| Formula | C18H34N2O6S |
| Molar mass | 406.538 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
Lincomycin is a lincosamide antibiotic that comes from the actinomyces Streptomyces lincolnensis.[1] A related compound, clindamycin, is derived from lincomycin by using thionyl chloride to replace the 7-hydroxy group with a chlorine atom with inversion of chirality.[2]
Uses
Although similar in structure, antibacterial spectrum, and mechanism of action to macrolides, lincomycin is also effective against other organisms including actinomycetes and some species of Mycoplasma and Plasmodium.
However, because of its adverse effects and toxicity, it is rarely used today and reserved for patients allergic to penicillin or where bacteria have developed resistance.
Clinical pharmacology
Intramuscular administration of a single dose of 600 mg of Lincomycin produces average peak serum levels of 11.6 micrograms/ml at 60 minutes, and maintains therapeutic levels for 17 to 20 hours, for most susceptible gram-positive organisms. Urinary excretion after this dose ranges from 1.8 to 24.8 percent (mean: 17.3 percent).
A two-hour intravenous infusion of 600 mg of Lincomycin achieves average peak serum levels of 15.9 micrograms/ml and yields therapeutic levels for 14 hours for most susceptible gram-positive organisms. Urinary excretion ranges from 4.9 to 30.3 percent (mean: 13.8 percent).
The biological half-life after IM or IV administration is 5.4 ± 1.0 hours. The serum half-life of lincomycin may be prolonged in patients with severe impairment of renal function, compared to patients with normal renal function. In patients with abnormal hepatic function, serum half-life may be twofold longer than in patients with normal hepatic function. Hemodialysis and peritoneal dialysis are not effective in removing lincomycin from the serum.
Tissue level studies indicate that bile is an important route of excretion. Significant levels have been demonstrated in the majority of body tissues. Although lincomycin appears to diffuse in the cerebrospinal fluid (CSF), levels of lincomycin in the CSF appear inadequate for the treatment of meningitis.
Biosynthesis
Lincomycin is an antibiotic classified as a constituent of the lincosamide group, which typically feature a 6,8-dideoxy-6-aminooctose lincosamine.[3] In Lincomycin A, this sugar moiety (referred to as methylthiolincosamide) is linked via an amide bond to an amino acid derivative (referred to as propylhygric acid). Lincomycin biosynthesis occurs via a biphasic pathway. Propylproline and methylthiolincosamide are each synthesized separately, which are then condensed to form N-demethyllincomycin and finally methylated by S-adenosyl methionine to give lincomycin.
In the biosynthesis of the amino acid moiety of lincomycin, tyrosine comprises seven of the nine carbons in the prophylhygric acid, while the remaining two carbons are added in reactions with S-adenosyl methionine.[4][5][6][7] Glucose is converted via glycolysis and the hexose monophosphate pathway to phosphoenolpyruvate and erythrose-4-phosphate, respectively, which are converted via the shikimate pathway to tyrosine and dihydroxyphenylalanine. Although the multistep conversion of dihydroxyphenylalanine to propylproline remains unknown, experiments involving accumulation of 1,2,3,6-tetradehydro-propylproline in mutants lacking a reductase requiring lincomycin cosynthetic factor suggests a biosynthetic scheme that Kuo and coworkers have modified from Brahme et al.[6][7] to accommodate the remaining steps leading to propylproline.[8][9]
The biosynthetic pathway for production of the methythiolincosamide sugar moiety is still not entirely known, although two different pathways have been predicted.[7][10] One possible pathway proposes the C8 carbon framework of methythiolincosamide originates from the condensation of a pentose (C5) unit, stemming from either the hexose monophosphate or condensation through a transketolase reaction with glyceraldehyde-3-phosphate and sedoheptulose-7-phosphate, and a C3 unit, added through a transaldolase reaction with sedoheptulose-7-phosphate. Once condensed, an octose (C8) unit is formed that can undergo isomerization to octose, dephosphorylation and reduction of the C8 carbon, transamination of 6-ketooctose, and thiomethylation of C1 to finally convert the octose unit to the methylthiolincosamide. A substantially different pathway for the formation of the methythiolincosamide proposes that its biosynthesis involves nucleotide activation followed by a series of modifications of dNTP-activated sugar intermediates. Eight genes, lmb-LMNZPOSQ, have been found to form a "sugar subcluster" which might be involved in this sugar metabolism.[11]
Condensation of the carboxyl group on the propylproline with the amine group of the methylthiolincosamide via an amide bond is catalyzed by N-Demethyllincomycin-synthetase. The resulting N-demethyllincomycin is then methylated by S-adenosyl methionine through N-Demethyllincomycin methyl transferase to form the final lincomycin product.[12]
Spectrum of susceptibility
Lincomycin is a narrow spectrum antibiotic with activity against Gram-positive and cell wall-less bacteria including pathogenic species of Streptococcus, Staphylococcus, and Mycoplasma.[13] Lincomycin is used to treat severe bacterial infections in people who cannot use penicillin antibiotics.[14] Lincomycin shows weak activity against most Gram-negative bacteria. The following represents susceptibility (MIC) data for a few pathogenic bacteria:
- Staphylococcus aureus - 0.2 µg/mL - 32 µg/mL
- Streptococcus pneumoniae - 0.05 µg/mL - 0.4 µg/mL[15]
- Streptococcus pyogenes - 0.04 µg/mL - 0.8 µg/mL[16]
See also
References
- ↑ PMID 14217764
- ↑ Birkenmeyer, R. D.; Kagan, F. (1970). "Lincomycin. XI. Synthesis and structure of clindamycin, a potent antibacterial agent". Journal of Medicinal Chemistry. 13 (4): 616–619. doi:10.1021/jm00298a007. PMID 4916317.
- ↑ Spízek J, Rezanka T (February 2004). "Lincomycin, cultivation of producing strains and biosynthesis". Appl. Microbiol. Biotechnol. 63 (5): 510–9. doi:10.1007/s00253-003-1431-3. PMID 14593504.
- ↑ Argoudelis AD, Eble TE, Fox JA, Mason DJ (August 1969). "Studies on the biosynthesis of lincomycin. IV. The origin of methyl groups". Biochemistry. 8 (8): 3408–11. doi:10.1021/bi00836a040. PMID 5809230.
- ↑ Witz DF, Hessler EJ, Miller TL (March 1971). "Bioconversion of tyrosine into the propylhygric acid moity of lincomycin". Biochemistry. 10 (7): 1128–33. doi:10.1021/bi00783a005. PMID 5553319.
- 1 2 Brahme NM, Gonzalez JE, Mizsak S, Rolls JR, Hessler EJ, Hurley LH (1984a) Biosynthesis of the lincomycins. 2. Studies using stable isotopes on the biosynthesis of methylthiolincosaminide moiety of lincomycin A. J Am Chem Soc 106:7878–7883.
- 1 2 3 Brahme NM, Gonzalez JE, Rolls JR, Hessler EJ, Mizsak S, Hurley LH (1984b) Biosynthesis of the lincomycins. 1. Studies using stable isotopes on the biosynthesis of the propyl- and ethyl-Lhygric aci moieties of lincomycin A and B. J Am Chem Soc 106:7873–7878.
- ↑ Kuo MS, Yurek DA, Coats JH, Li GP (March 1989). "Isolation and identification of 7,8-didemethyl-8-hydroxy-5-deazariboflavin, an unusual cosynthetic factor in streptomycetes, from Streptomyces lincolnensis". J. Antibiot. 42 (3): 475–8. doi:10.7164/antibiotics.42.475. PMID 2708143.
- ↑ Kuo MS, Yurek DA, Coats JH, Chung ST, Li GP (November 1992). "Isolation and identification of 3-propylidene-delta 1-pyrroline-5-carboxylic acid, a biosynthetic precursor of lincomycin". J. Antibiot. 45 (11): 1773–7. doi:10.7164/antibiotics.45.1773. PMID 1468986.
- ↑ Peschke U, Schmidt H, Zhang HZ, Piepersberg W (June 1995). "Molecular characterization of the lincomycin-production gene cluster of Streptomyces lincolnensis 78-11". Mol. Microbiol. 16 (6): 1137–56. doi:10.1111/j.1365-2958.1995.tb02338.x. PMID 8577249.
- ↑ Pissowotzki K, Mansouri K, Piepersberg W (December 1991). "Genetics of streptomycin production in Streptomyces griseus: molecular structure and putative function of genes strELMB2N". Mol. Gen. Genet. 231 (1): 113–23. doi:10.1007/BF00293829. PMID 1661369.
- ↑ Patt TE, Horvath BA (1985) Isolation and characterization of Ndemethyllincomycin methyltransferase. In: Abstracts, 13th International Congress of Biochemistry, Amsterdam, The Netherlands, August 25–30, 1985
- ↑ http://www.rxlist.com/lincocin-drug/indications-dosage.htm
- ↑ http://www.gmedication.com/?s=lincocin
- ↑ http://www.toku-e.com/Assets/MIC/Lincomycin%20HCl%20EP.pdf
- ↑ http://antibiotics.toku-e.com/antimicrobial_783.html