Tooth mobility
| Tooth mobility | |
|---|---|
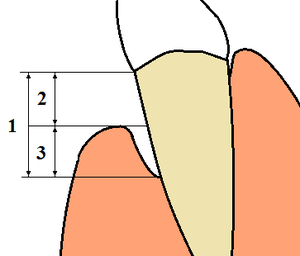 | |
| 1: Total loss of attachment (clinical attachment loss, CAL) is the sum of 2: Gingival recession, and 3: Probing depth (using a periodontal probe) | |
| Classification and external resources | |
| MeSH | D014086 |
Tooth mobility is the medical term for loose teeth.
Classification
Mobility is graded clinically by applying pressure with the ends of 2 metal instruments (e.g. dental mirrors) and trying to rock a tooth gently in a bucco-lingual direction (towards the tongue and outwards again). Using the fingers is not reliable as they are too compressible and will not detect small increases in movement.[1]:184 The location of the fulcrum may be of interest in dental trauma. Teeth which are mobile about a fulcrum half way along their root likely have a fractured root.[1]:184
Normal, physiologic tooth mobility of about 0.25 mm is present in health. This is because the tooth is not fused to the bones of the jaws, but is connected to the sockets by the periodontal ligament. This slight mobility is to accommodate forces on the teeth during chewing without damaging them.[2]:55 Milk (deciduous) teeth also become looser naturally just before their exfoliation.[1]:197 This is caused by gradual resorption of their roots, stimulated by the developing permanent tooth underneath.
Abnormal, pathologic tooth mobility occurs when the attachment of the peridontal ligament to the tooth is reduced (attachment loss, see diagram), or if the periodontal ligament is inflamed.[1]:220 Generally, the degree of mobility is inversely related to the amount of bone and periodontal ligament support left.
Grace & Smales Mobility Index[3]
- Grade 0: No apparent mobility
- Grade 1: Perceptible mobility <1mm in buccolingual direction
- Grade 2: 1mm< but <2mm
- Grade 3: 2mm< or depressibility in the socket
Miller Classification
- Class 1: < 1 mm(Horizontal)
- Class 2: >1 mm(Horizontal)
- Class 3: > 1 mm (Horizontal+vertical mobility)
Causes
Loss of attachment:
- By far the most common cause is periodontal disease (gum disease). This is painless, slowly progressing loss of bony support around teeth. It is made worse by smoking and the treatment is by improving the oral hygiene above and below the gumline.
- Dental abscesses can cause resorption of bone and consequent loss of attachment. Depending on the type of abscess, this loss of attachment may be restored once the abscess is treated, or it may be permanent.
- Many other conditions can cause permanent or temporary loss of attachment and increased tooth mobility. Examples include: Langerhans cell histiocytosis.[2]:35
Increased forces on the tooth:
- Bruxism (abnormal clenching and grinding of teeth) can aggravate attachment loss and tooth mobility if periodontal disease is already present.[2]:8 The tooth mobility is typically reversible and the tooth returns to normal level of mobility once the bruxism is controlled.
- Dental trauma. Luxations, and root fractures of teeth can cause sudden mobility after a blow. Dental trauma may be isolated or associated with other facial trauma.
- Increased biting force on one tooth can cause temporary increased mobility until corrected. A common scenario is a new filling or crown which is a fraction of a millimeter too prominent in the bite, which after a few days causes periodontal pain in that tooth and/or the opposing tooth.[1]:220
References
- 1 2 3 4 5 Odell EW (Editor) (2010). Clinical problem solving in dentistry (3rd ed.). Edinburgh: Churchill Livingstone. ISBN 9780443067846.
- 1 2 3 Heasman P (editor) (2008). Master Dentistry Vol I: Restorative dentistry, paediatric dentistry and orthodontics (2nd ed.). Edinburgh: Churchill Livingstone. ISBN 9780443068959.
- ↑ Dental Indices. In Marya, CM, editor. A Textbook of Public Health Dentistry. JP Medical Ltd, 2014. page 203