Probiotics in pediatrics
Probiotics are defined to be non-pathogenic strains of organism that are incorporated into the diet to modify gut microbial ecology, leading to beneficial structural and functional changes in the gut. Some probiotics may serve as a barrier for the colonization of pathogens to prevent disease and enhance the immune system. In addition, some may carry out metabolic functions such as helping the fermentation of nondigestible fibres, and storing energy in the form of short-chain fatty acids. Of all the types of gut microbiota, Bifidobacteria and Lactobacilli are considered the two most essential bacteria beneficial to human health while Staphylococci and Clostridia are considered pathogenic to human health.[1] Organisms that are considered as probiotics remain viable even after culturing, modification, and storage before ingestion. They are not killed during digestion, and ultimately adhere to the epithelium in the gut. As a consequence, the host may gain clinical health benefits, such as the reduction in antibiotic-associated diarrhea and allergies in infants. The microbiome, which is composed of ecosystems within and on the human body, is necessary for infants in the development of the gut-associated lymphoid tissue (GALT), an essential prerequisite for a normal immune system.[2]
Intestinal microflora in infancy
Determinants of the gut microbiota

At birth, the infant's intestines are free of bacteria, but bacteria starts to colonize within the intestine quickly after birth. Facultative aerobes are the first to colonize the intestine in infants. However, as time goes by, these facultative aerobes start to deplete the oxygen store within the infant's intestine, making the intestine a favorable environment to harbor anaerobes.[1] Overall, an infant's intestine is mainly colonized by enterobacteria during the first two days after birth.[2]
Bifidobacteria, lactobacilli, Escherichia coli and Clostridium difficile bacteroids are the major types of bacteria that are commonly found in infants’ GI tract but the proportion of each bacterium differs depending on several determinants.
The composition of the gut microbiota during the first few days is contributed mainly by the method of delivery, meaning that the composition is generally influenced by the mother and the surroundings.[1] Other than these, the environment during birth, prematurity, hygiene measures, and the type of infant feeding also contribute to the composition of an infant's intestinal microflora.
The mode of delivery is a first major determinant of an infant's intestinal flora in early life.
Cesarean section versus vaginal delivery
Infants that were given birth through cesarean section tend to contain fewer Bifidobacteria and Bacteroides and a higher amount of Clostridium difficile when compared with infants that were given birth naturally. This is because infants that are delivered through cesarean section are exposed initially to bacteria originating from the hospital environment and health care workers while vaginally born infants are colonized at first by fecal and vaginal bacteria of the mother. Lab results show that C. difficile is commonly found in hospital environments but is uncommon in healthy individuals. This result is relevant to the higher count of C. difficile in infants born through cesarean section. This is also because infants born through cesarean section on average stay in the hospital longer than vaginally born infants.[1] There are other contributors to the gut microbiota, including prematurity, hygiene level, and the method used to feed the infant.[2]
The next major determinant of an infant's intestinal flora is the type of feeding.
Formula-fed infants versus breast-fed infants
When comparing formula-fed and breast-fed infants, formula-fed infants' intestinal culture mostly consist of coliforms such as Escherichia coli, Clostridium difficile, bacteroids, and Lactobacilli bacteria. Hence, formula-fed infants have a more complex intestinal microflora than breast-fed infants. In breast-fed infants, Bifidobacteria contribute 80-90% of the microflora, while Lactobacilli and bacteroids constitutes a small amount in the intestine. However, Bacteroides, Veillonella, and Fusobacterium in the intestines start to increase in number after weaning. At this point, the child's intestinal microflora starts to develop in line with that in adults.[2]
Other determinants
Premature babies are found to have higher counts of C. difficile in their intestine. Furthermore, infants with older siblings tend to be colonized by more bifidobacteria in their intestines than infants with no siblings. Hence, the mode of delivery, type of infant feeding, gestational age, infant hospitalization and antibiotic use by the infant all greatly contribute to the composition of microflora in infants.[2]
Oral supplementation of Bifidobacteria and Lactobacilli are also useful in modifying the intestinal microflora in infants.[2]
Immunity
About 80% of all the immunologically active cells are located in the GALT. This implies that microbes in the gut are crucial in contributing to the immunological development of the GALT. It is necessary for the body to establish an efficient microbe-gut immune system interaction because there are about 1010 to 1012 prokaryotic organisms that are harbored in an infant's intestine and some are potentially pathogenic.[2]
Studies have been done to examine the gut-tissues of germ-free mice and found that the absence of microbes gave rise to an underdeveloped and sparse mucosal immune system. Characteristics of this underdeveloped mucosal immune system include a lamina propria that does not have IgA plasma cells or CD4 cells, and very small numbers of intraepithelial lymphocytes. This indicates that the mucosal immune system is dependent on gut bateria. Since new born infants do not show an underdeveloped and sparse mucosal immune system, it explains how microbes harbored in an infant's intestine are crucial for the development of a proper mucosal immune system.[2]
Furthermore, intestinal bacteria affect epithelium cell functions through signaling receptors such as Toll-like receptors. The function of the epithelium cell is to regulate immune gut response by controlling T cell differentiation and antibody responses to T cell-dependent antigens. One example is the IgA responses to luminal antigens. When pathogen antigens and gut lumen protein are present, one antibody response to these molecules would be IgA secretion. Hence, microbial colonization has an effect on the IgA responses to antigens in the lumen. Another immune function that microbial colonization gives is the ability to reduce the possibility of immune hyperreactivity such as allergies through inducing modulation of the T-helper type 2 and T-helper type 1 ratio.[2]
Importance of intestinal bacteria on immune function
Lactobacilli and Bifidobacteria are the two of the main types of bacteria that reside in the small intestine. Some commercial strains of these groups of bacteria are used as probiotics. Both bacterial groups may play a role in both local and systemic immunity of the intestine. Aside from providing a gut defense barrier, some strains of these two types of bacteria may secrete antimicrobial substates to inhibit the growth of pathogens.[2]
Intestinal bacteria are also shown to improve the secretory immune function and the intestinal flora such as influencing secretory immunoglobulin A (sIgA) synthesis and sIgA precursors. sIgA is an immunoglobulin that is present in mucosal surfaces. Its function is mainly to protect against the attack of antigens, pathogens, toxins and viruses.[2]
Researches have shown that high bacteroid and Clostridium counts accompanied by low Bifidobacterium counts can lead to an altered immune responses in infants. Premature infants are expected to have intestines that contain non-bifidobacterium species because of their frequent exposure to microbial environments and antibiotic use.[2]
Health benefits
Acute diarrhea
Many studies show that probiotics exhibit a protective effect against different types of acute diarrhea, such as antibiotic-associated diarrhea, traveller’s diarrhea and viral diarrhea.[3] In the United States, more than 15 million children develop acute diarrhea per year, with the treatment typically being rehydration and recuperative procedures.[4] As many prevention methods for diarrhea have adverse effects (e.g. intestinal intussusception in the usage of rotavirus vaccine), scientists are now turning to probiotics in hope of using it as a supplement to treat acute diarrhea.[5] In a review that covered 34 masked, randomized, placebo-controlled trials related to diarrhea and probiotics, it was concluded that there was an overall reduction of 52% in antibiotic associated diarrhea, an 8% reduction in traveller’s diarrhea, and a 34% reduction in other types of acute diarrhea. These numbers reflect a protective effect against diarrhea in subjects including both adults and children. In terms of children (age < 18 years), seven out of the 12 trials conducted in a health care setting showed a reduction in acute diarrhea of 57%. There was no significant difference in the protective effect of strains, namely Saccharomyces boulardii, Lactobacillus rhamnosus GG, Lactobacillus acidophilus, and Lactobacillus bulgaricus.[3]
Probiotics were found to be effective in treating acute, infectious diarrhea in children when a review was completed in 2001, involving > 700 children aged from one to 48 months with acute diarrhea.[6] A 2002 review showed that Lactobacillus reduced the average duration of acute diarrhea by 0.7 days and stool frequency by 1.6 on the second day of treatment. Dosage was most effective at more than ten billion colony-forming units of Lactobacillus during the first 48 hours of diarrhea.[7] Moreover, there has been evidence showing that probiotics can prevent children and infants from gastroenteritis (also known as stomach flu), which may also cause diarrhea to occur.[6]
The general mechanism in which probiotics protect against diarrhea is not known, but studies have shown that a dose of Lactobacillus rhamnosus GG of approximately 10^10 to 10^11 colony-forming units can inhibit the attachment of pathogenic organism in the intestine. Specifically for Lactobacillus, scientists have proposed that the organism fights diarrhea by increasing antimicrobial substances, competing for adherence sites with pathogenic organisms, and boosting the immune response to pathogens.[7] Probiotics may also help in maintaining the integrity of the gastrointestinal epithelium by preventing the production of cytokines, which can cause injury to intestinal epithelial cells with resulting diarrhea.[8] There have been no reports in where diarrhea has increased in severity due to patients receiving probiotic therapy.[2]
Antibiotic-associated diarrhea
Diarrhea can occur in 11–40% of children treated with antibiotics, and is commonly known as antibiotic-associated diarrhea or AAD.[9] The duration of the illness can range from the start of the therapy to two months after its termination.[10] This illness can generally be accounted for by Clostridium difficile, a bacterium that can sometimes cause severe diarrhea known as pseudomembranous colitis.[11] In a review of six trials related to antibiotic-associated diarrhea in 766 children aged one month to six years, there was an overall reduction in AAD when children were fed probiotics. The reduction, when compared to placebo, was seen to be from 28.5% to 11.9%; in fact, when patients were fed probiotics along with their dose of antibiotics, one fewer patient would develop AAD out of every seven. Antibiotics fed to the children in the trials included amoxicillin, penicillin and erythromycin. Evidence suggests that S. boulardii is best at preventing AAD in children, Lactobacillus GG ranking second, and a mixture of S. thermophilus and B. lactis relatively ranking last. No conclusion can be made on how probiotics can reduce the risk of AAD from any specific types of antibiotic.[6]

One of the proposed mechanisms of how probiotics protect from AAD is by regulating the composition of organisms in the intestines. Studies involving L. acidophilus and Bifidobacterium suggest that these microbes inhibit the growth of facultative anaerobic bacteria, which tends to increase during antibiotic treatment. As a result, it is seen that probiotics can alter and prevent changes in the intestinal microflora caused by antibiotics.[8]
Viral diarrhea
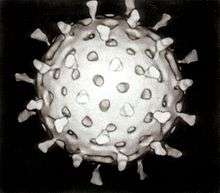
Viral diarrhea refers to diarrhea caused by a rotavirus, a virus often affecting toddlers and infants. A meta-analysis of nine previously conducted studies has shown that probiotics are also effective in treating viral diarrhea in hospitalized children. Countries of where these studies originated from include Canada, Thailand, and Finland, with subjects ranging from one to above 36 months old. On average, the duration of the illness was shortened by 0.7 days when placing the children on Lactobacillus therapy. Although it is still largely unknown as to how probiotics do this, two mechanisms have been currently proposed. The first mechanism suggests that Lactobacilli augment the development of intestinal mucins (glyosylated proteins), which consequently protect the body from intestinal infections. For the second mechanism, scientists suggest that probiotics prevent the growth of urease-producing bacteria, which typically occurs in the second stage of rotavirus diarrhea.[12]
Persistent diarrhea
A 2013 review suggested probiotics are effective in treating persistent diarrhea in children, though more research is needed. Persistent diarrhea is an episode that starts acutely but then lasts for 14 days or more; In developing countries it is an important cause of morbidity and mortality in children under five years old. The study showed average duration reduced by four days and shorter hospital stay; stool frequency was reduced on the fifth day.[13]
Allergy
Since the 1990s the incidence of allergic disease has increased in industrialized countries. Although current research is inconclusive, it suggests that probiotics may be beneficial in modulating host immune response and control allergic disease at an early age.[14] Atopic infants have shown to have a lower count of Bifidobacteria when compared to non-atopic infants and are more susceptible to allergen sensitization.
Atopic eczema is a common allergic inflammation of skin among infants. One randomized double-blind placebo-controlled study was conducted in infants who manifested atopic eczema during exclusive breast-feeding and who had no exposure to any infant or substitute formula. These infants were designated to wean to either hydrolyzed whey formula supplemented with probiotic strains Bifidobacterium lactis or Lactobacillus rhamnosus GG, or receive the hydrolyzed formula alone. The purpose of the study was to investigate incidence and severity of allergic response, growth and nutrition of studied infants, as well as to evaluate whether previous documented immunomodulatory effects of probiotics provide clinical benefit. Results were shown to improve the severity of skin manifestations by decreasing allergic-type immune response (T-cell activation) while promoting the development of suppressive helper cells and immunologic tolerance to antigens. Therefore, chances for immune hyperactivity (i.e. allergic disease) can be reduced. Another study that measured inflammatory mediator levels in infants' stool showed that infants with atopic dermititis (one type of eczema that is highly associated with cow's milk protein) and who were fed with GG supplemented-hydrolyzed whey formula excreted smaller amounts of inflammatory mediators. This suggested that Lactobacillus rhamnosus GG is one of the probiotics that improves integrity of the intestinal mucosal barrier and decreases gut inflammation.[15]
Numerous studies that used probiotics in different forms or sources—such as supplemented formula, supplemented water, and capsule in which contents were mixed with food—for treatment and management of atopy have associated with positive anti-inflammatory responses.[16][17][18] These suggested that regular probiotic supplementation may stabilize intestinal mucosal barrier function and play a role in modulating allergic responses and reduce severity of atopic symptoms.
Necrotizing enterocolitis

Necrotizing enterocolitis (NEC) is a medical condition primarily seen in premature infants where a portion of bowel undergoes necrosis (tissue death). A variety of factors has shown negatively to affect premature infants in obtaining adequate or optimal colonization of gut microflora: lack of exposure to normal maternal flora and immature mucosa are two reasons. Thus microflora establishment and composition in premature infants is a major determinant in the pathophysiology of NEC.
Using probiotics to prevent NEC is considered one of the most exciting probiotics applications today. Data in this area of research have shown reduction of NEC risk. Probiotics are beneficial in reducing enteric pathogens, improving gut structure and function, facilitating enteral nutrition, reducing dependence on parenteral nutrition, maintaining gut permeability, promoting intestinal mucosal barrier function, enhancing tolerance and reducing side-effects of antibiotic use. All of these lead to the clinical outcome of NEC prevention in infants.[19][20][21] The mechanisms of action of probiotics are that colonization of favourable types of microflora is increased, while the amount of pathogens is reduced. Probiotics are also capable of modulating gut immune response and improving humoral immunity, and thus host response changes.
There have been many studies conducted on premature infants who weigh less than normal healthy infants and are fed with Bifidobacteria and/or Lactobacillus at an early stage of life. Results showed significant decrease in expression of NEC and reduced severity when NEC did occur.[22][23][24] Other research conducted in more than 12,000 premature infants showed similar results and also showed reduction in NEC-associated mortality in the probiotic group.[22] Clinical trials also demonstrated increased bifidobacterium count significantly improves gut flora balancing and is associated with lower intestinal permeability in preterm infants.[25] Very low birth weight (VLBW) infants that are breast fed with probiotics supplemented have lower incidence of NEC when compared to VLBW infants that take breast milk alone.[23]
Safety
It is reported that most of the lactic acid-producing bacteria (LAB) strains used in the food supply are nonpathogenic and nontoxigenic.[2] They have been incorporated in food products for many years and are generally accepted as traditional food-grade organisms. Over 70 clinical studies to investigate potential probiotic-side effects have been conducted on more than 4000 children and infants that consume food containing microbial ingredients. None has shown any adverse effects.[2] Other studies that focused on long-term intake of probiotic-supplemented formula in infants have also shown no toxicity effect and incorporation well tolerated.[26] According to the 2002 report Guidelines for the Evaluation of Probiotics in Food, jointly published by the FAO and WHO, "documented correlations between systemetic infections and probiotic consumption are few and all occurred in patients with underlying medical conditions."[27] Rarely, consumption of probiotics may cause bacteremia, fungemia and sepsis in children with lowered immune systems who are already critically ill.[28] A 2013 systematic review found no adverse effects from Lactobacillus ingestion.[13]
Dose and Canadian regulations
Probiotics within Canadian regulations can be separated into two categories: probiotics in foods and in natural health products (NHP). For probiotics in foods, the bacterial cultures are considered as food ingredients and should be explicitly labeled on the product. Food products with microorganisms are regulated under the Food and Drugs Act, although there are no specific regulations for probiotics. In the case that the probiotic strain has been contained in the past in the food product with no dangers observed, Health Canada does not require a premarket safety review of the product. Probiotics that are sold as natural health products (e.g. in pharmaceutical form as in capsules) are regulated under the Natural Health Products Regulation.[29]
Health Canada defines health claims to be “any representation in labeling or advertising that states, suggests, or implies that a relationship exists between consumption of a food or food constituent (including an ingredient in the food) and a person’s health”. The following is a part of the regulation for health claims pertaining to probiotics:
- (a) The term "probiotic(s)" and similar terms or representations should be accompanied by a statement of the demonstrated effect of the probiotic;
- (b) The claimed effect of the probiotic microorganism in a food should be clearly stated in a manner that is not false, misleading, deceptive, or likely to create an erroneous impression with respect to the effect of or benefit from the probiotic microorganism(s) in the food;
- (c) Where a health claim is made, the Latin name (i.e., genus and species) and the strain of the probiotic microorganism or mixed culture that is the subject of the claim should be declared;
- (d) The level of the probiotic strain expressed in colony forming units (cfu) in a serving of stated size of the food should be declared; and
- (e) If more than one probiotic strain is added to a food, the above recommendations apply to the mixed culture.[30]
The probiotic products’ manufacturer is responsible for having the labeled level of microorganism delivered to the consumer. Thus, they are responsible for maintaining the stability and viability of the bacterial culture throughout the product’s shelf life. For example, when applying for a product to be an NHP, applicants must prove that the probiotic strain to be resistant to gastric and bile acid, safe for human use, and can benefit humans in one or more ways. Details on strains and quantity allowed for in bacterial cultures in NHP are outlined by the Natural Health Product Monograph.[31]
References
- 1 2 3 4 Penders, J.; Thijs, C.; Vink, C.; Stelma, F.F.; Snijders, B.; Kummeling, I.; Brandt, P.A.; Stobberingh, E.E. (2006). "Factors Influencing the Composition of the Intestinal Microbiota in Early Infancy". Pediatrics. 118 (2): 511–520. doi:10.1542/peds.2005-2824.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Saavedra, Jose M (2007). "Use of Probiotics in Pediatrics: Rationale, Mechanisms of Action, and Practical Aspects". Nutrition in Clinical Practice. 22 (3): 351–365. doi:10.1177/0115426507022003351.
- 1 2 Sazawal, S.; Hiremath, G.; Dhingra, U.; Malik, P.; Deb, S.; Black, R. E. (2006). "Efficacy of Probiotics in Prevention of Acute Diarrhoea: a Meta-analysis of Masked, Randomized, Placebo-controlled Trials". Lancet Infectious Diseases. 6: 374–382. doi:10.1016/s1473-3099(06)70495-9.
- ↑ Glass, R. I.; Lew, J. F.; Gangarose, R. E.; Lebaron, C. W.; Ho, M. (1991). "Estimates of Morbidity and Mortality Rates for Diarrhea Diseases in American Children". The Journal of Pediatrics. 118 (2): S27–S33.
- ↑ Huang, J. S.; Bousvaros, A.; Lee (2002). "Efficacy of Probiotic Use in Acute Diarrhea in Children: A Meta-analysis". Digestive Diseases and Sciences. 47 (11): 2625–2534.
- 1 2 3 Szajewska, H.; Mrukowicz, J. (2001). "Probiotics in the Treatment and Prevention of Acute Infectious Diarrhea in Infants and Children: A Systematic Review of Published Randomized, Double-Blind, Placebo-Controlled Trials". Journal of Pediatric Gastroenterology and Nutrition. 33 (2): S17–S25. doi:10.1097/00005176-200110002-00004.
- 1 2 Van Niel, C. W.; Feudtner, C.; Garrison, M. M.; Christakis, D. A. (2002). "Lactobacillus Therapy for Acute Infectious Diarrhea in Children: A Meta-analysis". Pediatrics. 109 (4): 678–685. doi:10.1542/peds.109.4.678.
- 1 2 Yan, F; Polk, D. B. (2006). "Probiotics as Functional Food in the Treatment of Diarrhea". Current Opinion in Clinical Nutrition and Metabolic Care. 9 (6): 717–721. doi:10.1097/01.mco.0000247477.02650.51.
- ↑ Turck, D.; Bernet, J. P.; Marx, J.; Kempf, H.; Giard, P.; Walbaum, O.; Lacombe, A.; Rembert, F.; Toursel, F.; Bernasconi, P.; Gottrand, G.; McFarland, L. V.; Bloch, K. (2003). "Incidence and Risk Factors of Oral Antibiotic-associated Diarrhea in an Outpatient Pediatric Population". Journal of Pediatric Gastroenterology and Nutrition. 37 (1): 22–26. doi:10.1097/00005176-200307000-00004.
- ↑ Elstner, C. L.; Lindsay, A. N.; Book, L. S.; Matsen, J. M. (1983). "Lack of Relationship of Clostridium difficile to antibiotic-associated diarrhea in Children". Pediatric Infectious Disease. 2 (5): 364–366. doi:10.1097/00006454-198309000-00006.
- ↑ Bartlett, J. G.; Chang, T. W.; Gurwith, M.; Gorbach, S.; Onderdonk, A. B. (1987). "Antibiotic-associated Pseudomembranous Colitis due to Toxin-producing Clostridia". The New England Journal of Medicine. 298 (10): 531–534.
- ↑ Nelson, J. M.; McCracken, G. H. (2005). "The Pediatric Infectious Disease Journal® Newsletter". The Pediatric Infectious Disease Journal. 24 (3): 267–268.
- 1 2 Bernaola Aponte, G; Bada Mancilla C; Carreazo N; Rojas Galarza R (August 2013). "Probiotics for persistent diarrhoea in children". Cochrane Database of Systematic Reviews (8). doi:10.1002/14651858.CD007401.pub3#sthash.DwpPRows.dpuf. Retrieved 23 September 2013.
- ↑ Isolauri, E.; Arvola, T.; Salminen, S. J.; et al. (2000). "Probiotics in the management of atopic eczema". Clin Exp Allergy. 30: 1604–1610.
- ↑ Isolauri, E (1996). "Studies on Lactobacillus GG in food hypersensitivity disorders". Nutr Today Suppl. 31: 285–315.
- ↑ Arvola, T., Moilanen, E., Vuento, R., Isolauri, E. (2002). Gut barrier during weaning in atopic infnats [abstract]. ESPGHAN 457
- ↑ Mullie, C.; Yazourh, A.; Thibault, H.; et al. (2004). "Increased poliovirus-specific intestinal antibody response coincides with promotion of Bifidobacterium logum or Bifidobacterium breve in infants: a randomized, double-blind, placebo-controlled trial". Pediatr Res. 56: 791–795. doi:10.1203/01.pdr.0000141955.47550.a0.
- ↑ Viljanen, M.; Kuitunen, M.; Hannhtela, T.; Juntunen-Backman, K.; Korpela, R.; Savilahti (2005). "Probiotic effects on faecal inflammatory markers and on faecal IgA in food allergic atopic eczema/dermatitis syndrome infants". Pediatr Allergy Immunol. 16: 65–71. doi:10.1111/j.1399-3038.2005.00224.x.
- ↑ Magne, F.; Suau, A.; Pochart, P.; Desjuex, J. F. (2005). "Fecal microbial community in preterm infants". J Pediatr Gastroenterol Nutr. 41: 386–392. doi:10.1097/01.mpg.0000179855.38543.85.
- ↑ Miller, M., Wilks, M., Costeloe, K. (2003). Probiotics for infants? Arch Dis Child Fetal Neonatal Ed. (88):F354-F358
- ↑ Vanderhoof J. A., Young, R. J. (2005). Pediatric applications of probiotics. Gastroenterol Clin North Am. (34): 451-454
- 1 2 Hoyos, A. B. (1999). Reduced incidence of necrotizing enterocolitis associated with enteral administration of Lactobacillus acidophilus and Bifidobacterium infantitis to neonates in an intensive care unit. Int J Infect Dis. (3): 197-202
- 1 2 Lin H.C., Su, B. H., Chen, A. C. et al.(2005). Oral probiotics reduce the incidence and severity of necrotizing enterocolitis in very low birth weight infants. Pediatrics (115): 1-4
- ↑ Bin-Nun A., Bromker, R., Wilschanski, M., et al. (2005). Oral probiotics prevent necrotizing enterocolitis in very low birth weight neonates. J Pediatr. (147): 192-196
- ↑ Stratiki, Z.; Costalos, C.; Sevastiadou, S.; et al. (2007). "The effect of a bifidobacter supplemented bovine milk on intestinal permeability of preterm infants". Early Hum Dev. 83: 575–579. doi:10.1016/j.earlhumdev.2006.12.002.
- ↑ Saavedra, J. M.; Abi-Hanna, A.; Moore, N.; Yolken, R. H. (2004). "Long-term consumption of infant formulas containing probiotic bacteria: tolerance and safety". American Journal of Clinical Nutrition. 79 (2): 261–261.
- ↑ Joint FAO/WHO. (2002). Guidelines for the Evaluation of Probiotics in Food. Joint FAO/WHO Working Group Report. Retrieved from ftp://ftp.fao.org/es/esn/food/wgreport2.pdf
- ↑ Singhi SC, Kumar S (2016). "Probiotics in critically ill children.". F1000Res (Review). 5. doi:10.12688/f1000research.7630.1. PMC 4813632
 . PMID 27081478.
. PMID 27081478. - ↑ Health Canada. (2009). Questions and Answers on Probiotics – Food Labelling. Retrieved from http://www.hc-sc.gc.ca/fn-an/label-etiquet/claims-reclam/probiotics_qa-qr_probiotiques-eng.php
- ↑ Health Canada. (2009). Guidance Document – The Use of Probiotic Microorganisms in Food. Retrieved from http://www.hc-sc.gc.ca/fn-an/legislation/guide-ld/probiotics_guidance-orientation_probiotiques-eng.php
- ↑ Health Canada. (2009). Natural Health Product Monograph - Probiotics. Retrieved from http://www.hc-sc.gc.ca/dhp-mps/prodnatur/applications/licen-prod/monograph/mono_probioti-eng.php