Race and health
| Race |
|---|
| Genetics and differences |
| Society |
| Race and... |
| Related topics |
|
Race and health refers to the relationship between individual health and one's race and ethnicity. Differences in health status, health outcomes, life expectancy, and many other indicators of health in different racial and ethnic groups is well documented, referred to as health disparities. Race is a complex concept, and the two major competing theories of race use biological definitions and social construction to define racial difference. Although this relationship can vary depending on the definitions used, race is generally used in the context of health research as a fluid concept to group populations of people according to various factors that include but are not limited to ancestry, social identity, visible phenotype, and genetic makeup.[1] Determinants of health include environmental, social, and genetic factors, as well as the person's individual characteristics and behaviors.[2]
Health disparities
Health disparities refer to gaps in the quality of health and health care across racial and ethnic groups.[3] The US Health Resources and Services Administration defines health disparities as "population-specific differences in the presence of disease, health outcomes, or access to health care."[4] Health is measured through variables such as life expectancy and incidence of diseases.[5]
How researchers view race is often linked to how we address racial disparities because the national administrator of health uses these research findings to implement policies.[6]
For more information, see the Health equity page's section on "Ethnic and racial disparities."
Defining race
There are various paradigms used to discuss race, including biological and social views. Definitions have changed throughout history to yield a modern understanding of race that is complex and fluid. Moreover, there is no one definition that stands, as there are many competing and interlocking ways to look at race.[6] The terms race, genetic population, ethnicity, geographic population, and ancestry are used interchangeably in everyday discourse involving race.
Biological definitions of race encompass essentialist and anti-essentialist views. The scientific community does not universally accept a single definition of race. Essentialism is a mode of thought that uses scientific data to argue that racial groups are genetically distinct populations. Essentialists describe "races as groups of people who share certain innate, inherited biological traits, aka use of biological evidence to demonstrate racial differences."[7] As its counterpart, anti-essentialism uses biological evidence to demonstrate that "race groupings do not reflect patterns of human biological variation, countering essentialist claims to the contrary."[8]
Social definitions are commonly constructionist. Racial groups are "constructed" from differing historical, political, and economic contexts, rather than corresponding to inherited, biological variations. Proponents of the constructionist view claim that biological definitions have been used to justify racism in the past and still have the potential to be used to encourage racist thinking in the future.[7]
Social views also better explain the ambiguity of racial definitions. An individual may self-identify as one race based on one set of determinants (for example, phenotype, culture, ancestry) while society may ascribe the person otherwise based on external forces and discrete racial standards. Dominant racial conceptions influence how individuals label both themselves and others within society.[9] Modern human populations are becoming more difficult to define within traditional racial boundaries due to racial admixture. Most scientific studies, applications, and government documents ask individuals to self-identify race from a limited assortment of common racial categories.[10] The conflict between self-identification and societal ascription further complicates biomedical research and public health policies. However complex its sociological roots, race has real biological ramifications; the intersection of race, science, and society permeates everyday life and influences human health via genetics, access to medical care, diagnosis, and treatment.
Race and disease
There are myriad factors that affect health disparities between racial groups. Among these factors are genetic differences within racial populations, cultural mores, and social and environmental factors. For instance, in some populations where perceptions of race are linked with socioeconomic disparities and differences, the access to care can be considerably lesser.[11] Dually, bias in healthcare systems themselves can perpetuate non-biologically founded higher instances of disease. For instance, in a study conducted by the National Health Service checks programme in the United Kingdom, which aims to increase diagnosis across demographics, "due to the reported lower screening in specific black and minority ethnic communities [-] who are recognised as being more at risk of cardiovascular disease [-] there are concerns that NHS Health Checks may increase inequalities in health."[12] In this specific case, the structure of services intended to treat and diagnose, these lower levels of attention to certain demographics can be seen as a cause of increased instances of disease from this lack of proper, equal preventative care. One must consider these external factors in evaluating statistics on the prevalence of disease in populations, as, though genetic components can be at play in terms of predispositions to contracting some illnesses, these linkages should be more closely evaluated than by ethnicity.[13] Overall, health disparities, which include variations in life expectancy and prevalence of disease, due to the differences in health conditions across various ethnic populations that can be attributed to inequalities in living environment and access to healthcare may also play a role.
Single-gene disorders
There are many single gene genetic disorders that differ in frequency between different populations due to the region, though many assume it to be solely based on race.[14] Examples include:
- Cystic fibrosis, the most common life-limiting autosomal recessive disease among people of Northern European heritage
- Sickle-cell anemia, most prevalent in populations with sub-Saharan African ancestry but also common among Latin-American, Indian, and Saudi Arab populations, as well as those people of South European regions such as Turkey, Greece, and Italy[15][16]
- Thalassemia, most prevalent in populations having Mediterranean ancestry, to the point that the disease's name is derived from Greek thalasson, "sea"
- Tay–Sachs disease, an autosomal recessive disorder more frequent among Ashkenazi Jews than among other Jewish groups and non-Jewish populations[17]
- Hereditary hemochromatosis, most common among persons having Northern European ancestry, in particular those people of Celtic descent
- Lactose intolerance affects (over their lifetime) as many as 25% of Europeans but up to 50-80% of Hispanics, along with people from southern India and Ashkenazi Jews, but nearly 100% of Native Americans.[18]
Multifactorial polygenic diseases
Many diseases differ in frequency between different populations. However, complex diseases are affected by multiple factors, both genetic and environmental. There is controversy over the extent to which some of these conditions are influenced by genes, and ongoing research aims to identify which genetic loci, if any, are linked to these diseases. "Risk is the probability that an event will occur. In epidemiology, it is most often used to express the probability that a particular outcome will occur following a particular exposure."[19][20] Different populations are considered "high-risk" or "low-risk" groups for various diseases due to the probability of that particular population being more exposed to certain risk factors. Beyond genetic factors, history and culture, as well as current environmental and social conditions, influence a certain populations' risk for specific diseases.
Disease progression
Groups may differ in how a disease progresses. Black men who were diagnosed with HIV generally fared worse than their white and Hispanic counterparts.[21] The percentage of men studied with very low CD4+ T-cell count, defined as fewer than 50 cells per microliter, at AIDS diagnosis was 24.1% for white men, 27.8% for Hispanic men, and 34.4% for Black men. Black men were also significantly less likely to be alive three years after diagnosis (80.6%) than Hispanic or white men, who had 85.2% and 84.5% survival rates, respectively. However, the reasons for these differences are not clear, and should not be understood as an essential difference between races, but rather as effects of social and environmental factors.
Prevention
Genetics have been proven to be a strong predictor for common diseases such as cancer, cardiovascular disease (CVD), diabetes, autoimmune disorders, and psychiatric illnesses,[22] and geneticists have been able to determine that “human genetic variation is geographically structured.” The different geographic regions correlate with different races,[23] which is logical when looking at the "Out of Africa" theory and understanding how changes in genetics of a population acquire over time.
Examples of diseases which are more common in certain racial groups are sickle-cell disease in African and Mediterranean populations, and cystic fibrosis and hemochromatosis in northern European populations.[23] This information can be made available to people by their physicians, and is useful in prevention or early detection of these diseases. For instance, a baby with sickle cell disease should be more closely monitored throughout their life than a baby without it.
While genetics certainly play a role in determining how susceptible a person is to specific diseases, environmental factors and lifestyle play a large role as well.[24] For this reason, it is impossible to discern exactly what causes a person to acquire a disease, but it's clear that a mixture of all 3 factors are at play. Each person's health is unique, as they have different genetic compositions and life histories.
Race-based treatment
The science of 'ethnic health', or research into ethnicity and health, and the development of services which are culturally competent to meet the specific health care needs of minority ethnic groups, is still in its infancy.[25] In the United States, the Office of Minority Health provides useful links and supports research and development relating to the needs of America's ethnic minorities. In the United Kingdom, the National Health Service established a specialist collection on Ethnicity & Health.[26] This resource was supported by the National Institute for Health and Clinical Excellence (NICE) as part of the UK NHS Evidence initiative NHS Evidence.[27] Similarly, there are growing numbers of resource and research centers which are seeking to provide this service for other national settings, such as Multicultural Mental Health Australia.
"Race-based medicine" is the term for medicines that are targeted at specific ethnic clusters which are shown to have a propensity for a certain disorder. The first example of this in the U.S. was when BiDil, a medication for congestive heart failure, was licensed specifically for use in American patients that self-identify as black.[28] Previous studies had shown that African American patients with congestive heart failure generally respond less effectively to traditional treatments than white patients with similar conditions.[29]
After two trials, BiDil was licensed exclusively for use in African American patients. Critics have argued that this particular licensing was unwarranted, since the trials did not in fact show that the drug was more effective in African Americans than in other groups, but merely that it was more effective in African Americans than other similar drugs. It was also only tested in African American males, but not in any other racial groups or among women. This peculiar trial and licensing procedure has prompted suggestions that the licensing was in fact used as a race-based advertising scheme.[30]
Critics are concerned that the trend of research on race-specific pharmaceutical treatments will result in inequitable access to pharmaceutical innovation and smaller minority groups may be ignored. This has led to a call for regulatory approaches to be put in place to ensure scientific validity of racial disparity in pharmacological treatment.[31]
An alternative to "race-based medicine" is personalized medicine that involves identifying genetic, genomic (i.e., genomic sequencing), and clinical information—as opposed to using race as a proxy for these data—to better predict a patient's predisposition to certain diseases.[32]
Environmental factors
A positive correlation between minorities and a socio economic status of being low income in industrialized and rural regions of the U.S. depict how low income communities tend to include more individuals that have a lower educational background, most importantly in health. Income status, diet, and education all construct a higher burden for low income minorities, to be conscious about their health. Research conducted by medical departments at universities in San diego, Miami, Pennsylvania, and North Carolina suggested that minorities in regions where lower socioeconomic status is common, there was a direct relationship with unhealthy diets and greater distance of supermarkets.[33] Therefore, in areas where supermarkets are less accessible (food deserts) to impoverished areas, the more likely these groups are to purchase inexpensive fast food or just follow an unhealthy diet.[33] As a result, because food deserts are more prevalent in low income communities, minorities that reside in these areas are more prone obesity, which can lead to diseases such as Chronic Kidney disease, hypertension, or diabetes.[33][34]
Furthermore, this can also occur when minorities living in rural areas undergoing urbanization, are introduced to fast food. A study done in Thailand focused on urbanized metropolitan areas, the students who participated in this study as were diagnosed as “non-obese” in their early life according to their BMI, however were increasingly at risk of developing Type 2 Diabetes, or obesity as adults, as opposed to young adults who lived in more rural areas during their early life.[35] Therefore, early exposure to urbanized regions can encourage unhealthy eating due to widespread presence of inexpensive fast food. Different racial populations that originate from more rural areas and then immigrate to the urbanized metropolitan areas can develop a fixation for a more westernized diet; this change in lifestyle typically occurs due to loss of traditional values when adapting to a new environment. For example, a 2009 study named CYKIDS was based on children from Cyprus, a country east of the mediterranean sea, who were evaluated by the KIDMED index to test their adherence to a mediterranean diet after changing from rural residence to an urban residence.[36] It was found that children in urban areas swapped their traditional dietary patterns for a diet favoring fast food.
Genetic factors
The fact that every human has a unique genetic code, is the key to techniques such as genetic fingerprinting. Versions of a trait, known as alleles, occur at different frequencies in different human populations; populations that are more geographically and ancestrally remote tend to differ more.
A phenotype is the "outward, physical manifestation" of an organism."[37] For humans, phenotypic differences are most readily seen via skin color, eye color, hair color, or height; however, any observable structure, function, or behavior can be considered part of a phenotype. A genotype is the "internally coded, inheritable information" carried by all living organisms. The human genome is encoded in DNA[37]
For any trait of interest, observed differences among individuals "may be due to differences in the genes" coding for a trait or "the result of variation in environmental condition". This variability is due to gene-environment interactions that influence genetic expression patterns and trait heritability.[38]
For humans, there is "more genetic variation among individual people than between larger racial groups."[5] In general, an average of 80% of genetic variation exists within local populations, around 10% is between local populations within the same continent, and approximately 8% of variation occurs between large groups living on different continents.[39] Studies have found evidence of genetic differences between populations, but the distribution of genetic variants within and among human populations is impossible to describe succinctly because of the difficulty of defining a "population", the clinal nature of variation, and heterogeneity across the genome.[40] Thus, the racialization of science and medicine can lead to controversy when the term population and race are used interchangeably.
Evolutionary factors
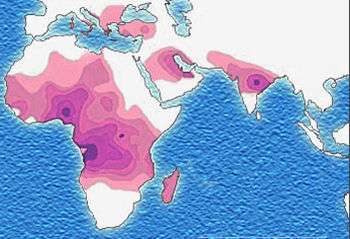
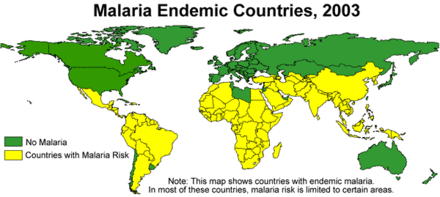
Genes may be under strong selection in response to local diseases. For example, people who are duffy negative tend to have higher resistance to malaria. Most Africans are duffy negative and most non-Africans are duffy positive.[41] A number of genetic diseases more prevalent in malaria-afflicted areas may provide some genetic resistance to malaria including sickle cell disease, thalassaemias, glucose-6-phosphate dehydrogenase, and possibly others.
Many theories about the origin of the cystic fibrosis have suggested that it provides a heterozygote advantage by giving resistance to diseases earlier common in Europe.
In earlier research, a common theory was the "common disease-common variant" model. It argues that for common illnesses, the genetic contribution comes from the additive or multiplicative effects of gene variants that each one is common in the population. Each such gene variant is argued to cause only a small risk of disease and no single variant is enough to cause the disease. An individual must have many of these common gene variants in order for the risk of disease to be substantial.[42]
More recent research indicates that the "common disease-rare variant" may be a better explanation for many common diseases. In this model, rare but higher-risk gene variants cause common diseases. This model may be relevant for diseases that reduces fertility. In contrast, for common genes associated with common disease to persist they must either have little effect during the reproductive period of life (like Alzheimer's disease) or provide some advantage in the original environment (like genes causing autoimmune diseases also providing resistance against infections). In either case varying frequencies of genes variants in different populations may be an explanation for health disparities.[42] Genetic variants associated with Alzheimer's disease, deep venous thrombosis, Crohn disease, and type 2 diabetes appear to adhere to "common disease-common variant" model.[43]
Gene flow
Gene flow and admixture can also have an effect on relationships between race and race-linked disorders. Multiple sclerosis, for example, is typically associated with people of European descent, but due to admixture African Americans have elevated levels of the disorder relative to Africans.[44]
Some diseases and physiological variables vary depending upon their admixture ratios. Examples include measures of insulin functioning[45] and obesity.[46]
Gene interactions
The same gene variant, or group of gene variants, may produce different effects in different populations depending on differences in the gene variants, or groups of gene variants, they interact with. One example is the rate of progression to AIDS and death in HIV–infected patients. In Caucasians and Hispanics, HHC haplotypes were associated with disease retardation, particularly a delayed progression to death, while for African Americans, possession of HHC haplotypes was associated with disease acceleration. In contrast, while the disease-retarding effects of the CCR2-641 allele were found in African Americans, they were not found in Caucasians.[47]
Controversy regarding race in biomedicine
There is a controversy regarding race as a method for classifying humans. Different sources argue it is purely social construct or a biological reality reflecting average genetic group differences. New interest in human biological variation has resulted in a resurgence of the use of race in biomedicine.[48]
The main impetus for this development is the possibility of improving the prevention and treatment of certain diseases by predicting hard-to-ascertain factors, such as genetically conditioned health factors, based on more easily ascertained characteristics such as phenotype and racial self-identification. Since medical judgment often involves decision making under uncertain conditions,[49] many doctors consider it useful to take race into account when treating disease because diseases and treatment responses tend to cluster by geographic ancestry.[50] The discovery that more diseases than previously thought correlate with racial identification have further sparked the interest in using race as a proxy for bio-geographical ancestry and genetic buildup.
Race in medicine is used as an approximation for more specific genetic and environmental risk factors. Race is thus partly a surrogate for environmental factors such as differences in socioeconomic status that are known to affect health. It is also an imperfect surrogate for ancestral geographic regions and differences in gene frequencies between different ancestral populations and thus differences in genes that can affect health. This can give an approximation of probability for disease or for preferred treatment, although the approximation is less than perfect.[5]
Taking the example of sickle-cell disease, in an emergency room, knowing the geographic origin of a patient may help a doctor doing an initial diagnosis if a patient presents with symptoms compatible with this disease. This is unreliable evidence with the disease being present in many different groups as noted above with the trait also present in some Mediterranean European populations. Definitive diagnosis comes from examining the blood of the patient. In the US, screening for sickle cell anemia is done on all newborns regardless of race.[49]
The continued use of racial categories has been criticized. Apart from the general controversy regarding race, some argue that the continued use of racial categories in health care and as risk factors could result in increased stereotyping and discrimination in society and health services.[5][51][52] Some of those who are critical of race as a biological concept see race as socially meaningful group that is important to study epidemiologically in order to reduce disparities.[53] For example, some racial groups are less likely than others to receive adequate treatment for osteoporosis, even after risk factors have been assessed. Since the 19th century, blacks have been thought to have thicker bones than whites have and to lose bone mass more slowly with age.[54] In a recent study, African Americans were shown to be substantially less likely to receive prescription osteoporosis medications than Caucasians. Men were also significantly less likely to be treated compared with women. This discrepancy may be due to physicians' knowledge that, on average, African Americans are at lower risk for osteoporosis than Caucasians. It may be possible that these physicians generalize this data to high-risk African-Americans, leading them to fail to appropriately assess and manage these individuals' osteoporosis.[54] On the other hand, some of those who are critical of race as a biological concept see race as socially meaningful group that is important to study epidemiologically in order to reduce disparities.
David Williams (1994) argued, after an examination of articles in the journal Health Services Research during the 1966-90 period, that how race was determined and defined was seldom described. At a minimum, researchers should describe if race was assessed by self-report, proxy report, extraction from records, or direct observation. Race was also often used questionable, such as an indicator of socioeconomic status.[55] Racial genetic explanations may be overemphasized, ignoring the interaction with and the role of the environment.[56]
From concepts of race to ethnogenetic layering
There is general agreement that a goal of health-related genetics should be to move past the weak surrogate relationships of racial health disparity and get to the root causes of health and disease. This includes research which strives to analyze human genetic variation in smaller groups than races across the world.[5]
One such method is called ethnogenetic layering. It works by focusing on geographically identified microethnic groups. For example, in the Mississippi Delta region ethnogenetic layering might include such microethnic groups as the Cajun (as a subset of European Americans), the Creole and Black groups [with African origins in Senegambia, Central Africa and Bight of Benin] (as a subset of African Americans), and Choctaw, Houmas, Chickasaw, Coushatta, Caddo, Atakapa, Karankawa and Chitimacha peoples (as subsets of Native American Indians).[57][58]
Better still may be individual genetic assessment of relevant genes.[59] As genotyping and sequencing have become more accessible and affordable, avenues for determining individual genetic makeup have opened dramatically.[60] Even when such methods become commonly available, race will continue to be important when looking at groups instead of individuals such as in epidemiologic research.[59]
Some doctors and scientists such as geneticist Neil Risch argue that using self-identified race as a proxy for ancestry is necessary to be able to get a sufficiently broad sample of different ancestral populations, and in turn to be able to provide health care that is tailored to the needs of minority groups.[61]
Association studies
One area in which population categories can be important considerations in genetics research is in controlling for confounding between population genetic substructure, environmental exposures, and health outcomes. Association studies can produce spurious results if cases and controls have differing allele frequencies for genes that are not related to the disease being studied,[62][63] although the magnitude of its problem in genetic association studies is subject to debate.[64][65] Various techniques detect and account for population substructure,[66][67] but these methods can be difficult to apply in practice.[68]
Population genetic substructure also can aid genetic association studies. For example, populations that represent recent mixtures of separated ancestral groups can exhibit longer-range linkage disequilibrium between susceptibility alleles and genetic markers than is the case for other populations.[69][70][71][72] Genetic studies can use this disequilibrium to search for disease alleles with fewer markers than would be needed otherwise. Association studies also can take advantage of the contrasting experiences of racial or ethnic groups, including migrant groups, to search for interactions between particular alleles and environmental factors that might influence health.[73][74]
Human genome projects
The Human Genome Diversity Project has collected genetic samples from 52 indigenous populations.
Sources of racial disparities in care
In a report by the Institute of Medicine called Unequal Treatment, three major source categories are put forth as potential explanations for disparities in health care: patient-level variables, healthcare system-level factors, and care process-level variables.[75]
Patient-level variables
There are many individual factors that could explain the established differences in health care between different racial and ethnic groups. First, attitudes and behaviors of minority patients are different. They are more likely to refuse recommended services, adhere poorly to treatment regimens, and delay seeking care, yet despite this, these behaviors and attitudes are unlikely to explain the differences in health care.[75] In addition to behaviors and attitudes, biological based racial differences have been documented, but these also seem unlikely to explain the majority of observed disparities in care.[75]
Health system-level factors
Health system-level factors include any aspects of health systems that can have different effects on patient outcomes. Some of these factors include different access to services, access to insurance or other means to pay for services, access to adequate language and interpretation services, and geographic availability of different services.[75] Many studies assert that these factors explain portions of the existing disparities in health of racial and ethnic minorities in the United States when compared to their white counterparts.
Care process-level variables
Three major mechanisms are suggested by the Institute of Medicine that may contribute to healthcare disparities from the provider's side: bias (or prejudice) against racial and ethnic minorities; greater clinical uncertainty when interacting with minority patients; and beliefs held by the provider about the behavior or health of minorities.[75] Research in this area is new and ongoing.
See also
- Dark skin#Health implications
- Light skin#Health implications
- HapMap[76]
- Human stature#Average height around the world
- List of countries by life expectancy
- Ethnic bioweapon
- Social determinants of health
- Social determinants of health in poverty#Ethnicity
- Health equity#Ethnic and racial disparities
- Ethnopsychopharmacology
- Pharmacogenomics
- Category:Human genome projects
United States:
General:
References
- ↑ http://www.genome.gov/Glossary/index.cfm?id=171
- ↑ World Health Organization. The determinants of health. Geneva. Accessed 12 May 2011 (which are inter-related with all three, but mostly social factors).
- ↑ U.S. Department of Health and Human Services (HHS), Healthy People 2010: National Health Promotion and Disease Prevention Objectives, conference ed. in two vols (Washington, D.C., January 2000).
- ↑ Goldberg, Janet; Hayes, William; Huntley, Jill (November 2004). Understanding Health Disparities (PDF). Health Policy Institute of Ohio. p. 3.
- 1 2 3 4 5 Collins, Francis S. (November 2004). "What we do and don't know about 'race', 'ethnicity', genetics and health at the dawn of the genome era". Nature Genetics. 36 (11 Suppl): S13–S15. doi:10.1038/ng1436. PMID 15507997.
- 1 2 http://library.brown.edu/reserves/pdffiles/34469_Whitmarsh_Vernaculars.pdf
- 1 2 http://raceandgenomics.ssrc.org/Morning/
- ↑ The Nature Of Race: How Scientists Think And Teach About Human Difference, Chapter 4: Teaching Race, Ann Morning p 114.
- ↑ Social interpretations of race
- ↑ http://rds.epi-ucsf.org/ticr/syllabus/courses/23/2012/03/29/Lecture/readings/The%20Importance%20of%20Race%20%26%20Ethnicity%20in%20Biomedical%20Research%20and%20Clinical%20Practice..pdf
- ↑ Williams, D R; Lavizzo-Mourey, R; Warren, R C (1994-01-01). "The concept of race and health status in America.". Public Health Reports. 109 (1): 26–41. ISSN 0033-3549. PMC 1402239
 . PMID 8303011.
. PMID 8303011. - ↑ Riley, Ruth; Coghill, Nikki; Montgomery, Alan; Feder, Gene; Horwood, Jeremy (2015-12-10). "The provision of NHS health checks in a community setting: an ethnographic account". BMC Health Services Research. 15. doi:10.1186/s12913-015-1209-1. ISSN 1472-6963. PMC 4676171
 . PMID 26651487.
. PMID 26651487. - ↑ Horowitz, Carol R.; Davis, Margaret H.; Palermo, Ann-Gel S.; Vladeck, Bruce C. (2000-01-01). "Approaches to Eliminating Sociocultural Disparities in Health". Health Care Financing Review. 21 (4): 57–74. ISSN 0195-8631. PMC 4194638
 . PMID 11481745.
. PMID 11481745. - ↑ Lu, YF; Goldstein, DB; Angrist, M; Cavalleri, G (24 July 2014). "Personalized medicine and human genetic diversity.". Cold Spring Harbor perspectives in medicine. 4 (9): a008581. doi:10.1101/cshperspect.a008581. PMID 25059740.
- ↑ http://www.ornl.gov/sci/techresources/Human_Genome/posters/chromosome/sca.shtml
- ↑ Bloom, Miriam. Understanding Sickle Cell Disease. University Press of Mississippi, 1995. Chapter 2.
- ↑ Myrianthopoulos NC, Aronson SM (July 1966). "Population dynamics of Tay-Sachs disease. I. Reproductive fitness and selection.". American Journal of Human Genetics. 18 (4): 313–27. PMC 1706099
 . PMID 5945951.
. PMID 5945951. - ↑ Bhatnagar, Shinjini; Aggarwal, Rakesh (2007), "Lactose intolerance", British Medical Journal, 334: 1331–1332, doi:10.1136/bmj.39252.524375.80, PMC 1906652
 , PMID 17599979
, PMID 17599979 |contribution=ignored (help) - ↑ http://www.nidcr.nih.gov/NR/rdonlyres/59E8463F-469F-4D06-95C3-CB877673DC98/0/Brian_Burt_Risk.pdf
- ↑ http://www.who.int/genomics/public/geneticdiseases/en/index3.html
- ↑ "Racial/ethnic and age disparities in HIV prevalence and disease progression among men who have sex with men in the United States". Am J Public Health. 97: 1060–6. 2007. doi:10.2105/AJPH.2006.087551. PMC 1874211
 . PMID 17463370.
. PMID 17463370. - ↑ Hernandez, Lyla M.; Blazer, Dan G.; Institute of Medicine (US) Committee on Assessing Interactions Among Social, Behavioral (2006-01-01). "Genetics and Health".
- 1 2 Jorde, Lynn B.; Wooding, Stephen P. (2004-10-26). "Genetic variation, classification and 'race'". Nature Genetics. 36: S28–S33. doi:10.1038/ng1435. PMID 15508000.
- ↑ Anderson, Norman B.; Bulatao, Rodolfo A.; Cohen, Barney; National Research Council (US) Panel on Race, Ethnicity (2004-01-01). "Genetic Factors in Ethnic Disparities in Health".
- ↑ Johnson, Mark (2006), "Ethnicity", in Killoran, Amanda; Swann, Catherine; Kelly, Michael P., Public Health Evidence: Tackling health inequalities, Oxford University Press http://ukcatalogue.oup.com/product/9780198520832.do Missing or empty
|title=(help) - ↑ "NHS Evidence - ethnicity and health".
- ↑ NHS Evidence
- ↑ Taylor AL, Ziesche S, Yancy C, Carson P, D'agostino Jr R, Ferdinand K, Taylor M, Adams K, et al. (2004). "(November 2004). "Combination of isosorbide dinitrate and hydralazine in blacks with heart failure"". The New England Journal of Medicine. 351 (20): 2049–57. doi:10.1056/NEJMoa042934. PMID 15533851.
- ↑ Exner DV, Dries DL, Domanski MJ, Cohn JN (2001). "Lesser response to angiotensin-converting-enzyme inhibitor therapy in blacks as compared with white patients with left ventricular dysfunction". N Engl J Med. 344 (18): 1351–7. doi:10.1056/NEJM200105033441802. PMID 11333991.
- ↑ Ellison, George (2006) Medicine in black and white: BiDil: race and the limits of evidence-based medicine. Significance, Volume 3, Number 3, September 2006 , pp. 118–121(4)
- ↑ Winichoff, D. E., Obasagie, O. K. (2008) Race-specific drugs: Regulatory trends in public policy. Trends in Pharmacological Sciences. http://www.geneticsandsociety.org/article.php?id=4110
- ↑ http://health.usnews.com/health-conditions/cancer/personalized-medicine#2
- 1 2 3 Suarez, Jonathan J.; Isakova, Tamara; Anderson, Cheryl A. M.; Boulware, L. Ebony; Wolf, Myles; Scialla, Julia J. (2015-12-01). "Food Access, Chronic Kidney Disease, and Hypertension in the U.S". American Journal of Preventive Medicine. 49 (6): 912–920. doi:10.1016/j.amepre.2015.07.017. ISSN 1873-2607. PMC 4656149
 . PMID 26590940.
. PMID 26590940. - ↑ "About Chronic Kidney Disease". The National Kidney Foundation. Retrieved 2016-03-16.
- ↑ Angkurawaranon, Chaisiri; Wisetborisut, Anawat; Rerkasem, Kittipan; Seubsman, Sam-ang; Sleigh, Adrian; Doyle, Pat; Nitsch, Dorothea (2015-09-16). "Early life urban exposure as a risk factor for developing obesity and impaired fasting glucose in later adulthood: results from two cohorts in Thailand". BMC Public Health. 15. doi:10.1186/s12889-015-2220-5. ISSN 1471-2458. PMC 4572635
 . PMID 26376960.
. PMID 26376960. - ↑ Lazarou, Chrystalleni; Kalavana, Theano (2009-01-01). "Urbanization influences dietary habits of Cypriot children: the CYKIDS study". International Journal of Public Health. 54 (2): 69–77. doi:10.1007/s00038-009-8054-0. ISSN 1661-8564. PMID 19234670.
- 1 2 http://www.brooklyn.cuny.edu/bc/ahp/BioInfo/GP/Definition.html
- ↑ "Estimating additive genetic variation and heritability of phenotypic traits". userwww.sfsu.edu. Retrieved 2016-03-25.
- ↑ Lewontin 1972; Jorde et al. 2000a; Hinds et al. 2005
- ↑ Long and Kittles 2003
- ↑ Malaria and the Red Cell,Harvard University. 2002 url=http://sickle.bwh.harvard.edu/malaria_sickle.html
- 1 2 McClellan, J.; King, M. C. (2010). "Genetic Heterogeneity in Human Disease". Cell. 141 (2): 210–217. doi:10.1016/j.cell.2010.03.032. PMID 20403315.
- ↑ Lohmueller KE, Pearce CL, Pike M, Lander ES, Hirschhorn JN (2003). "Meta-analysis of genetic association studies supports a contribution of common variants to susceptibility to common disease". Nat Genet. 33 (2): 177–182. doi:10.1038/ng1071. PMID 12524541.
- ↑ Cree BA, Khan O, Bourdette D, Goodin DS, Cohen JA, Marrie RA, Glidden D, Weinstock-Guttman B, et al. (December 2004). "Clinical characteristics of African Americans vs Caucasian Americans with multiple sclerosis". Neurology. 63 (11): 2039–45. doi:10.1212/01.WNL.0000145762.60562.5D. PMID 15596747.
- ↑ Gower B. A.; et al. (2003). "Using genetic admixture to explain racial differences in insulin-related phenotypes". Diabetes. 52: 1047–1051. doi:10.2337/diabetes.52.4.1047.
- ↑ Fernandez J. R.; et al. (2003). "Association of African genetic admixture with resting metabolic rate and obesity among women". Obes. Res. 11: 904–911. doi:10.1038/oby.2003.124. PMID 12855761.
- ↑ Gonzalez E, et al. (1999). "Race-specific HIV-1 disease-modifying effects associated with CCR5 haplotypes". Proc. Natl. Acad. Sci. USA. 96: 12004–12009.
- ↑ Ian Whitmarsh and David S. Jones, 2010, What's the Use of Race? Modern Governance and the Biology of Difference, MIT press. Page 188. "Far from waning in the age of molecular genetics, race has been resurgent in biomedical discourse, especially in relation to a torrent of new interest in human biological variation and its quantification."
- 1 2 Ian Whitmarsh and David S. Jones, 2010, What's the Use of Race? Modern Governance and the Biology of Difference, MIT press. Chapter 9.
- ↑ Satel, Sally. "I Am a Racially Profiling Doctor". The New York Times, published May 5, 2002
- ↑ Ian Whitmarsh and David S. Jones, 2010, What's the Use of Race? Modern Governance and the Biology of Difference, MIT press. Chapter 5.
- ↑ Sheldon TA, Parker H (June 1992). "Race and ethnicity in health research". Journal of Public Health Medicine. 14 (2): 104–10. PMID 1515192.
- ↑ Williams DR, Lavizzo-Mourey R, Warren RC (1994). "The concept of race and health status in America". Public Health Reports. 109 (1): 26–41. PMC 1402239
 . PMID 8303011.
. PMID 8303011. - 1 2 "Population-based fracture risk assessment and osteoporosis treatment disparities by race and gender". J Gen Intern Med. 24: 956–62. 2009. doi:10.1007/s11606-009-1031-8. PMC 2710475
 . PMID 19551449.
. PMID 19551449. - ↑ Williams DR (August 1994). "The concept of race in Health Services Research: 1966 to 1990". Health Services Research. 29 (3): 261–74. PMC 1070005
 . PMID 8063565.
. PMID 8063565. - ↑ Goodman AH (November 2000). "Why genes don't count (for racial differences in health)". American Journal of Public Health. 90 (11): 1699–702. doi:10.2105/AJPH.90.11.1699. PMC 1446406
 . PMID 11076233.
. PMID 11076233. - ↑ Jackson F.L.C. (2008). "Ethnogenetic layering (EL): an alternative to the traditional race model in human variation and health disparity studies". Annals of Human Biology. 35 (2): 121–144. doi:10.1080/03014460801941752.
- ↑ Jackson, F. L. (2004). "Human genetic variation and health: new assessment approaches based on ethnogenetic layering". British Medical Bulletin. 69: 215–235. doi:10.1093/bmb/ldh012. PMID 15226208.
- 1 2 Jordge Lynn B.; Wooding Stephen P. (2004). "Genetic Variation, classification and 'race'".". Nature Genetics. 36 (11): S28–S33. doi:10.1038/ng1435. PMID 15508000.
- ↑ http://www.gis.a-star.edu.sg/internet/site/data/sup_data/2253/individual_genomes_instead_of_race_for_personalized_medicine.pdf
- ↑ Risch N.; Burchard E.; Ziv E.; Tang H. (2002). "Categorization of humans in biomedical research: genes, race and disease". Genome Biol. 3 (7): 1–12. doi:10.1186/gb-2002-3-7-comment2007. PMC 139378
 . PMID 12184798.
. PMID 12184798. - ↑ Cardon LR, Palmer LJ (2003). "Population stratification and spurious allelic association". Lancet. 361 (9357): 598–604. doi:10.1016/S0140-6736(03)12520-2. PMID 12598158.
- ↑ Marchini J, Cardon LR, Phillips MS, Donnelly P (2004). "The effects of human population structure on large genetic association studies". Nat Genet. 36 (5): 512–517. doi:10.1038/ng1337. PMID 15052271.
- ↑ Thomas DC, Witte JS (2002). "Point: population stratification: a problem for case-control studies of candidate-gene associations?". Cancer Epidemiol Biomarkers Prev. 11 (6): 505–512. PMID 12050090.
- ↑ Wacholder S, Rothman N, Caporaso N, "Counterpoint: bias from population stratification is not a major threat to the validity of conclusions from epidemiological studies of common polymorphisms and cancer," Cancer Epidemiol Biomarkers Prev (2002) 11 :513–520.
- ↑ Morton NE, Collins A (1998). "Tests and estimates of allelic association in complex inheritance". Proc Natl Acad Sci USA. 95 (19): 11389–11393. doi:10.1073/pnas.95.19.11389. PMC 21652
 . PMID 9736746.
. PMID 9736746. - ↑ Hoggart CJ, Parra EJ, Shriver MD, Bonilla C, Kittles RA, Clayton DG, McKeigue PM (2003). "Control of confounding of genetic associations in stratified populations". American Journal of Human Genetics. 72 (6): 1492–1504. doi:10.1086/375613. PMC 1180309
 . PMID 12817591.
. PMID 12817591. - ↑ Freedman ML, Reich D, Penney KL, McDonald GJ, Mignault AA, Patterson N, Gabriel SB, Topol EJ, Smoller JW; Reich; Penney; McDonald; Mignault; Patterson; Gabriel; Topol; Smoller; Pato; Pato; Petryshen; Kolonel; Lander; Sklar; Henderson; Hirschhorn; Altshuler; et al. (2004). "Assessing the impact of population stratification on genetic association studies". Nat Genet. 36 (4): 388–393. doi:10.1038/ng1333. PMID 15052270.
- ↑ Hoggart CJ, Shriver MD, Kittles RA, Clayton DG, McKeigue PM; Shriver; Kittles; Clayton; McKeigue (2004). "Design and analysis of admixture mapping studies". American Journal of Human Genetics. 74 (5): 965–978. doi:10.1086/420855. PMC 1181989
 . PMID 15088268.
. PMID 15088268. - ↑ Patterson N, Hattangadi N, Lane B, Lohmueller KE, Hafler DA, Oksenberg JR, Hauser SL, Smith MW, O'Brien SJ; Hattangadi; Lane; Lohmueller; Hafler; Oksenberg; Hauser; Smith; O'Brien; Altshuler; Daly; Reich; et al. (2004). "Methods for high-density admixture mapping of disease genes". American Journal of Human Genetics. 74 (5): 979–1000. doi:10.1086/420871. PMC 1181990
 . PMID 15088269.
. PMID 15088269. - ↑ Smith MW, Patterson N, Lautenberger JA, Truelove AL, McDonald GJ, Waliszewska A, Kessing BD; Patterson; Lautenberger; Truelove; McDonald; Waliszewska; Kessing; Malasky; Scafe; Le; De Jager; Mignault; Yi; De The; Essex; Sankale; Moore; Poku; Phair; Goedert; Vlahov; Williams; Tishkoff; Winkler; de la Vega; Woodage; Sninsky; Hafler; Altshuler; et al. (2004). ", "A high-density admixture map for disease gene discovery in African Americans". American Journal of Human Genetics. 74 (5): 1001–1013. doi:10.1086/420856. PMC 1181963
 . PMID 15088270.
. PMID 15088270. - ↑ McKeigue PM (2005). "Prospects for admixture mapping of complex traits". American Journal of Human Genetics. 76 (1): 1–7. doi:10.1086/426949. PMC 1196412
 . PMID 15540159.
. PMID 15540159. - ↑ Chaturvedi N (2001). "Ethnicity as an epidemiological determinant—crudely racist or crucially important?". Int J Epidemiol. 30 (5): 925–927. doi:10.1093/ije/30.5.925. PMID 11689494.
- ↑ Collins FS, Green ED, Guttmacher AE, Guyer MS, US National Human Genome, Institute Research (2003). "A vision for the future of genomics research". Nature. 422 (6934): 835–847. doi:10.1038/nature01626. PMID 12695777.
- 1 2 3 4 5 Smedley, Brian D. (2002). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC.: National Academies Press. pp. 7–12. ISBN 0-309-50911-4.
- ↑ HapMap
External links
- Cultural Diversity in Healthcare Speaker Series University of Wisconsin School of Medicine and Public Health
- Cultural Diversity in Healthcare Research Symposium University of Wisconsin School of Medicine and Public Health
- News-Medical.net
- Unnatural causes, videos on how racial inequalities influence health
Governmental
- United States Office of Minority Health
- United Kingdom National Health Service - Ethnicity & Health
- Multicultural Mental Health Australia