Tactile imaging
Tactile imaging, also called "mechanical imaging", "stress imaging" or "computerized palpation", is a medical imaging modality that translates the sense of touch into a digital image. The tactile image is a function of P(x,y,z), where P is the pressure on soft tissue surface under applied deformation and x,y,z are coordinates where pressure P was measured. The tactile image is a pressure map on which the direction of tissue deformation must be specified. Tactile imaging closely mimics manual palpation, since the probe of the device with a pressure sensor array mounted on its face acts similar to human fingers during clinical examination, deforming soft tissue by the probe and detecting resulting changes in the pressure pattern.

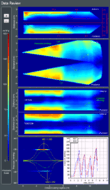
Interpretation: Inverse problem solution for P(x,y,z) would allow reconstruction of the tissue elasticity distribution (E) as function of the same coordinates E(x,y,z). The tissue elasticity image brings valuable information about the tissue or organ because the tissue elasticity modulus is highly sensitive to tissue structural changes accompanying various physiological and pathological processes. Unfortunately, the inverse problem solution is hardly possible for most real objects because it is non-linear and ill posed problem. However, it appeared that the tactile image per se, P(x,y,z), closely reflects the information content of the elasticity image and reveals tissue or organ anatomy and elasticity structure.[1] The tissue elasticity at specified location can be estimated on the basis of spatial gradients within P(x,y,z). Figure 1 presents an experiment on a composite tissue phantom examined by a tactile imaging probe illustrating the ability to visualize the structure of the object.
History
Historically, the human sense of touch has been the most prevalent and successful medical diagnostic technique. A great variety of diseases were diagnosed through tactile sensing. We find in Kahun Gynecological Papyrus[2] dated 1825 B.C.: "Discernere eam quae concepit ... like that finger upon her menaa." Hippocrates in 400 B.C. wrote: "Such swellings as are soft, free from pain, and yield to the finger, ... and are less dangerous than the others. ... then, as are painful, hard, and large, indicate danger of speedy death; but such as are soft, free of pain, and yield when pressed with the finger, are more chronic than these...".[3]
During the last century, traditional physical examination techniques were becoming outmoded and were often considered of little clinical value in comparison with many other modern diagnostic technologies. Palpation is only briefly addressed in medical school, and few physicians have the tactile ability to detect subtle variations of tissue elasticity. Few physicians are willing to devote the necessary time to master the technique, despite the fact that the American Cancer Society guidelines suggest for women that clinical breast examination (CBE) be part of a periodic health examination[4] and the American Urological Association in their 2009 Best Practices Statement recommended that men who wish to be screened for prostate cancer should have both a prostate-specific antigen (PSA) test and a digital rectal examination (DRE).[5]
The first description of a technical implementation related to Tactile Imaging was given in the late 1970s by Frei et al.[6] who proposed an instrument for breast palpation that used a plurality of spaced piezoelectric force sensors. The sensors were pressed against the breast tissue by a pressure member which applied a given periodic or steady stress to the tissue. A different principle for evaluating the pattern of pressure distribution over a compressed breast was proposed by Gentle[7] in 1980s. The pressure distribution was monitored optically by using the principle of frustrated total internal reflection to generate a brightness distribution. Then, Sabatini et al. built a robotic system for discriminating mechanical inhomogeneities in a soft tissue using a finger-like palpation device equipped with a fingertip piezoelectric polymer film tactile sensor.[8] The first review about the tactile sensor development for robots is dated by 1986.[9]
Mechanical imaging, as a modality of medical diagnostics using mechanical sensors, was introduced in the 1990s by Sarvazyan[10][11] and later by Wellman et al.[12][13] Many physical principles have been explored for the realization of tactile sensors: resistive, inductive, capacitive, optoelectric, magnetic, piezoelectric and electroacoustic principles, in a variety of configurations.[14][15][16]
Medical applications
The terms elasticity, hardness and stiffness correspond most closely to a rigorous physical parameter – Young's modulus, also elastic modulus. The significant dependence of Young's modulus on structural changes in the tissue is the basis for the palpatory diagnosis of various diseases, such as detection of cancer nodules in the breast or prostate. Detection of a mechanical heterogeneity by manual palpation is based exclusively on sensing the variations of Young’s modulus of tissue.
Tactile imaging is a branch of elasticity imaging or elastography.[17] There are two major differences between tactile imaging and all other types of elasticity imaging based on either ultrasound or magnetic resonance imaging. The first difference is that tactile imaging reconstructs the internal mechanical structure of tissue using the data of stress pattern over the compressed tissue, while ultrasound or MR elasticity imaging are based on detection of strain induced in the tissue by various static or dynamic means.[18] The second difference is that tactile imaging uses relatively larger tissue deformations to collect stress data under the applied load.

Vagina and pelvic floor
There are about 2.7 billion women aged over 21 years old worldwide. Almost all of them due to the changes of tissue elasticity with pregnancy and the age will have at least one pelvic floor problem.[19][20][21][22] The effective management of pelvic floor disorders, including stress urinary incontinence (SUI) and pelvic floor prolapse (POP), requires objective tools for evaluation of physiological, anatomical and functional conditions of the female pelvic floor and its support structures. It leads to understanding of the disorders which can be challenging due to their complexity. The understanding and diagnosis, in turn, lead to use of minimally invasive and most effective treatment options with predictable response/outcome. Application of specific aesthetic procedures, e.g. vaginal tightening and rejuvenation, requires quantitive assessment of vaginal conditions before and after to demonstrate objective changes and/or improvements. The Vaginal Tactile Imager (VTI), as shown in Figure 2A, translates the sense of touch into computer image allowing visualization of the vagina and pelvic floor support structures in terms of elasticity (stiffness).[23][24] Tactile image for normal conditions is shown in Figure 2B. It enables assessment of pelvic floor conditions and function by quantitative, anatomically sensitive and specific manner. VTI allows high-definition Functional Muscle Tactile Imaging along the entire vagina during voluntary muscle contraction, involuntary relaxation, involuntary reflex contraction and Valsalva maneuver. Full VTI examination protocol includes 8 tests. An operator observes all of them in real time on VTI display. The VTI examination report is automatically generated and stored in a digital format. The Vaginal Tactile Imager is approved by the FDA as an aid in diagnosis and evaluation of vaginal and female pelvic floor conditions.
Breast
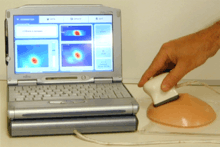

Breast cancer is one of the most common causes of death from cancer. The lifetime probability of developing breast cancer in the next 10 years is evaluated as 13%.[4] A critical key to a continued reduction in mortality is early detection and accurate diagnosis made in a cost-effective manner. Figure 3 shows a general view of Breast Tactile Imager (BTI). The device includes a probe with a pressure sensor array, an electronic unit, and a laptop computer. BTI can quantitatively evaluate multiple mechanical and structural properties of breast and breast lesions, such as Young’s modulus, elasticity contrast, tissue nonlinearity (strain hardening), heterogeneity index, nodule size, shape and mobility, which could be altered by cancer development.[1] Clinical data collected at four different sites for 179 cases have demonstrated BTI's capability for characterizing and differentiating benign and malignant breast lesions.[25] Histologically confirmed malignant breast lesions demonstrated increased hardness and strain hardening as well as decreased mobility in comparison with benign lesions. Statistical analysis of data on 147 benign and 32 malignant lesions revealed BTI's sensitivity of 91.4% and specificity of 86.8%. Examples of cysts and ductal carcinoma images recorded by BTI are shown in Figure 4. BTI has the potential to be used as a cost effective device for cancer detection as a diagnostic modality. It was estimated that the use of the BMI after standard screening procedures (mammography alone or combination of mammography and conventional ultrasound) could significantly reduce the benign biopsy rate.[25] This device similar to BTI, SureTouch is approved by the FDA as a visual mapping system for documentation of the findings at clinical breast examination.
Prostate


Prostate cancer is the most prevalent type of cancer among men and is projected to be diagnosed in about 600,000 men in the U.S. and Europe.[26] Figure 5A shows a general view of Prostate Mechanical Imager (PMI). The device includes a probe with a pressure sensor array and motion tracking system, a movable cart with an electronic unit and a computer. PMI provides a real-time 3-D image of the prostate and detects the presence and location of abnormalities within the gland. PMI enables a physician to visually examine and store a 3-D reconstructed image of the prostate and evaluate prostate volume, elasticity and elasticity contrast. The utility of PMI is similar to the utility provided by DRE, which is currently considered a standard of care for men over the age of 50. PMI can minimize subjectivity in the DRE by providing an ease-to-use and accurate tool for visualizing abnormalities of the prostate.[27][28][29] Figure 5B illustrates the PMI examination as an electronic palpation and shows a characteristic example of clinical data. This device, Prostate Mechanical Imager, is approved by the FDA as a system which produces an elasticity image of the prostate to document prostate abnormalities that were previously identified by digital rectal examination.


Myofascial trigger points
Chronic pain is a critical public health problem. A majority of patients in specialty pain management centers and those with chronic pain disorders suffer from a poorly understood condition called myofascial pain syndrome, which is characterized by pain associated with localized tender nodules in taut bands of skeletal muscle called myofascial trigger points. The Myofascial Trigger Point Tactile Imager (MTPTI) as shown in Figure 6A is a tactile imaging device that provides a 2-D tactile visualization and assessment of the elastic properties of the myofascial trigger points by using a tactile imaging probe.[30] The images and signal information are stored and can be accessed for review or data analysis. The MTPTI can be used by a chiropractic or massage therapy practitioner to map the tissue elasticity of the myofascial trigger points (Figure 6B).
See also
References
- 1 2 Egorov V, Sarvazyan AP (September 2008). "Mechanical imaging of the breast". IEEE Transactions on Medical Imaging. 27 (9): 1275–87. doi:10.1109/TMI.2008.922192. PMC 2581459
 . PMID 18753043.
. PMID 18753043. - ↑ The Kahun Gynaecological Papyrus. 1825 B.C.
- ↑ Hippocrates. The Book of Prognostics. 400 B.C.
- 1 2 American Cancer Society. 2010. Breast Cancer Facts & Figures 2009–2010. Atlanta, GA: American Cancer Society, Inc. pp.1-40
- ↑ Greene KL, Albertsen PC, Babaian RJ, et al. (November 2009). "Prostate specific antigen best practice statement: 2009 update". The Journal of Urology. 182 (5): 2232–41. doi:10.1016/j.juro.2009.07.093. PMID 19781717.
- ↑ Frei EH, Sollish BD, Yerushalmi S. inventors; Yeda Research and Development Co. Ltd., assignee. Instrument for viscoelastic measurement. U.S. Patent 4,144,877; 1979.
- ↑ Gentle CR (April 1988). "Mammobarography: a possible method of mass breast screening". Journal of Biomedical Engineering. 10 (2): 124–6. doi:10.1016/0141-5425(88)90086-6. PMID 3361866.
- ↑ Sabatini, AM; Dario, P; Bergamasco, M (1990). "Interpretation of mechanical properties of soft tissues from tactile measurements". Experimental Robotics I, Lecture Notes in Control and Information Sciences. 139: 452–462. doi:10.1007/BFb0042534.
- ↑ Yardley AMM, Baker KD. Tactile Sensors for Robots: A Review. In: The world Yearbook of Robotics Research and development. Eds. Scott PB. 1986: 47-83.
- ↑ Sarvazyan AP, Skovoroda AR. June 1996. Method and apparatus for elasticity imaging. U.S. Patent 5,524,636; 1996.
- ↑ Sarvazyan A (April 1998). "Mechanical imaging: a new technology for medical diagnostics". International Journal of Medical Informatics. 49 (2): 195–216. doi:10.1016/S1386-5056(98)00040-9. PMID 9741894.
- ↑ Wellman, PS (1999). Tactile imaging (PhD thesis). Cambridge, MA: Harvard University's Division of Engineering and Applied Sciences. pp. 1–158. OCLC 46515069.
- ↑ Wellman PS, Dalton EP, Krag D, Kern KA, Howe RD (February 2001). "Tactile imaging of breast masses: first clinical report". Archives of Surgery. 136 (2): 204–8. doi:10.1001/archsurg.136.2.204. PMID 11177142.
- ↑ Regtien, PPL (1992). "Tactile imaging". Sensors and Actuators A: Physical. 31 (1–3): 83–9. doi:10.1016/0924-4247(92)80084-G.
- ↑ Galea, AM (2004). Mapping tactile imaging information: parameter estimation and deformable registration (PhD thesis). Cambridge, MA: Harvard University's Division of Engineering and Applied Sciences. pp. 1–235. OCLC 70682744.
- ↑ Tegin, J; Wikander, J (2005). "Tactile sensing in intelligent robotic manipulation – a review". Industrial Robot. 32 (1): 64–70. doi:10.1108/01439910510573318.
- ↑ Sarvazyan A, Egorov V (February 2012). "Mechanical Imaging - a Technology for 3-D Visualization and Characterization of Soft Tissue Abnormalities. A Review". Current Medical Imaging Reviews. 8 (1): 64–73. doi:10.2174/157340512799220571. PMC 3776320
 . PMID 24058326.
. PMID 24058326. - ↑ Sarvazyan A, Egorov V, Sarvazyan N (2012). "Tactile Sensing and Tactile Imaging in Detection of Cancer". In Harold, Keith E. Biosensors and Molecular Technologies for Cancer Diagnostics. CRC Press. pp. 337–52.
- ↑ Swift SE. The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol. 2000;183:277-85.
- ↑ Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet 2007;369(9566):1027-38.
- ↑ Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096-100.
- ↑ Rahn DD, Ruff MD, Brown SA, Tibbals HF, Word RA. Biomechanical properties of the vaginal wall: effect of pregnancy, elastic fiber deficiency, and pelvic organ prolapse. Am J Obstet Gynecol. 2008;198(5):590.e1-6.
- ↑ Egorov V, van Raalte H, Sarvazyan AP (July 2010). "Vaginal tactile imaging". IEEE Transactions on Bio-medical Engineering. 57 (7): 1736–44. doi:10.1109/TBME.2010.2045757. PMC 3079341
 . PMID 20483695.
. PMID 20483695. - ↑ Egorov V, van Raalte H, Lucente V (April 2012). "Quantifying vaginal tissue elasticity under normal and prolapse conditions by tactile imaging". International Urogynecology Journal. 23 (4): 459–66. doi:10.1007/s00192-011-1592-z. PMC 3306492
 . PMID 22072417.
. PMID 22072417. - 1 2 Egorov V, Kearney T, Pollak SB, et al. (November 2009). "Differentiation of benign and malignant breast lesions by mechanical imaging". Breast Cancer Research and Treatment. 118 (1): 67–80. doi:10.1007/s10549-009-0369-2. PMC 2803347
 . PMID 19306059.
. PMID 19306059. - ↑ Ferlay J, Parkin DM, Steliarova-Foucher E (March 2010). "Estimates of cancer incidence and mortality in Europe in 2008". European Journal of Cancer. 46 (4): 765–81. doi:10.1016/j.ejca.2009.12.014. PMID 20116997.
- ↑ Weiss RE, Hartanto V, Perrotti M, et al. (December 2001). "In vitro trial of the pilot prototype of the prostate mechanical imaging system". Urology. 58 (6): 1059–63. doi:10.1016/S0090-4295(01)01407-8. PMID 11744495.
- ↑ Egorov V, Ayrapetyan S, Sarvazyan AP (October 2006). "Prostate mechanical imaging: 3-D image composition and feature calculations". IEEE Transactions on Medical Imaging. 25 (10): 1329–40. doi:10.1109/tmi.2006.880667. PMC 2572682
 . PMID 17024836.
. PMID 17024836. - ↑ Weiss RE, Egorov V, Ayrapetyan S, Sarvazyan N, Sarvazyan A (March 2008). "Prostate mechanical imaging: a new method for prostate assessment". Urology. 71 (3): 425–9. doi:10.1016/j.urology.2007.11.021. PMC 2323601
 . PMID 18342178.
. PMID 18342178. - ↑ Turo, D; Otto, P; Egorov, V; Sarvazyan, A; Gerber, LH; Sikdar, S (2012). "Elastography and tactile imaging for mechanical characterization of superficial muscles". The Journal of the Acoustical Society of America. 132 (3): 1983. Bibcode:2012ASAJ..132.1983T. doi:10.1121/1.4755316.