Urothelium
| Urothelium | |
|---|---|
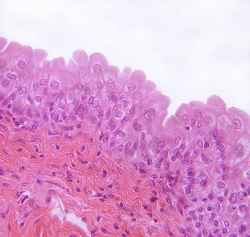 Transitional epithelium of the urinary bladder. Note the rounded surface of the apical cells -- a distinguishing characteristic of this type of epithelium. | |
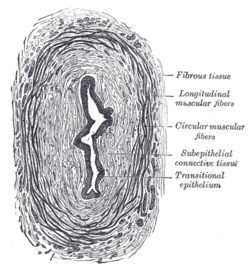 Transverse section of ureter. | |
| Identifiers | |
| FMA | 67695 |
Urothelium (or uroepithelium) is an example of "transitional epithelium". It is the type of epithelium that lines much of the urinary tract including the renal pelvis, the ureters, the bladder,[1] and parts of the urethra.[2]
Structure and function
Urothelial tissue is highly specific to the urinary tract, and has high elasticity and trans-epithelial electrical resistance.[2]
Urothelium consists of approximately 3-5 cell layers, accompanied by a thick layer of protective glycoprotein plaques at its luminal (apical) surface, and is classified as transitional epithelium.
Pathology
Epithelia are sites of specific diseases.
- Cancers that originate in epithelial cells are termed carcinomas, and they are characterized as having lost the mature, differentiated morphology and molecular patterns of the normal tissue. Infectious diseases also afflict epithelia where diverse microbes (viruses, bacteria, fungi) have surface structures that bind specific features of particular epithelial cells (e.g., influenza virus binds respiratory epithelium). Genetic defects can also inhibit normal epithelial integrity, such as defects in intercellular adhesion molecules that result in blistering diseases.
- The second most common infectious disease is urinary tract infection (UTI). UTIs afflict approximately half of all women during their lifetime, and about 25% of these women will suffer recurrent UTIs. The majority of these infections are due to uropathogenic Escherichia coli bacteria (commonly known as E. coli). However, UTIs can also develop in healthcare settings and such infections are caused by a greater frequency of non-E. coli bacteria.
- One unusual condition which affects the urothelium is interstitial cystitis (IC), a condition with symptoms similar to UTI (urinary frequency, urinary urgency, pressure and/or pain). Urine culture, however, is negative. During hydrodistention of the bladder, small petechial hemorrhages (aka glomerulations) are frequently found throughout the bladder. Larger "Hunner's Ulcers", known for their characteristic waterfall bleeding effect, represent larger areas of bladder wall thinning and/or trauma. The cause of IC is currently unknown though some suggest that it could be genetic, the result of traumatic injury (aka chemical exposure), infection, autoimmune disease, etc. Researcher Susan Keay (University of Maryland) has found an unusual protein in the urine of IC patients which appears to interfere with healing, known as an Antiproliferative Factor. Research efforts into IC are focused on the urothelium, including newly discovered signaling molecules which suggest that the urothelium is far more than a barrier, as well as how the urothelium interacts with proximal nerves and smooth muscle.
- Urothelium is susceptible to carcinoma. Because the bladder is in contact with urine for extended periods, chemicals that become concentrated in the urine can cause Bladder cancer. For example, cigarette smoking leads to the concentration of carcinogens in the urine and is a leading cause of bladder cancer. Aristolochic acid, a compound found in plants of the Aristolochiaceae family, also causes DNA mutations and is a cause of liver, urothelial and bladder cancers.[3] Occupational exposure to certain chemicals is also a risk factor for bladder cancer. This can include aromatic amines (aniline dye), polycytic aromatic hydrocarbons, and diesel engine exhaust.[4]
Urothelial lesions
- Papillary urothelial lesions
- Papillary urothelial hyperplasia
- Urothelial papilloma
- Papillary urothelial neoplasm of low malignant potential (PUNLMP)
- Low-grade papillary urothelial carcinoma
- High-grade papillary urothelial carcinoma
- Invasive urothelial carcinoma
- Flat urothelial lesions
- Reactive urothelial atypia
- Urothelial inverted papilloma
- Urothelial atypia of unknown significance
- Urothelial dysplasia
- Urothelial carcinoma in situ
- Invasive urothelial carcinoma
- Invasive urothelial carcinoma (NOS)
- Urothelial carcinoma with inverted growth pattern
- Urothelial carcinoma with squamous differentiation
- Urothelial carcinoma with villoglandular differentiation
- Urothelial carcinoma, micropapillary variant
- Urothelial carcinoma, lymphoepithelioma-like variant
- Urothelial carcinoma, clear cell (glycogen-rich) variant
- Urothelial carcinoma, lipoid cell variant
- Urothelial carcinoma with syncitiotrophoblastic giant cells
- Urothelial carcinoma with rhabdoid differentiation
- Urothelial carcinoma similar to giant cell tumor of bone
References
Notes
- ↑ Moro, C; Uchiyama, J; Chess-Williams, R (December 2011). "Urothelial/lamina propria spontaneous activity and the role of M3 muscarinic receptors in mediating rate responses to stretch and carbachol". Urology. 76 (6): 1442.e9–15. doi:10.1016/j.urology.2011.08.039. PMID 22001099.
- 1 2 Andersson, 2011: p. 134
- ↑ "Mutation signatures implicate aristolochic acid in bladder cancer development". Genome Medicine. 7 (1). Dec 2015. doi:10.1186/s13073-015-0161-3.
- ↑ "Bladder cancer risk factors". Cancer Research UK. Retrieved 27 July 2014.
Bibliography
- Andersson, Karl-Erik (2011). Urinary Tract. Springer. ISBN 978-3-642-16498-9.
External links
- www.urothelium.com is an online resource for information about Human Urothelium and the "Biomimetic Urothelium"
- Urothelium at the US National Library of Medicine Medical Subject Headings (MeSH)
- Histology at qmul.ac.uk
- Diagram at umich.edu
- Histology at wisc.edu
This article is issued from Wikipedia - version of the 11/1/2016. The text is available under the Creative Commons Attribution/Share Alike but additional terms may apply for the media files.