Obstetric fistula
| Obstetric fistula | |
|---|---|
 | |
| Areas where obstetric fistulae commonly occur | |
| Classification and external resources | |
| Specialty | urology |
| ICD-10 | N82 |
| ICD-9-CM | 619 |
| MeSH | D014624 |
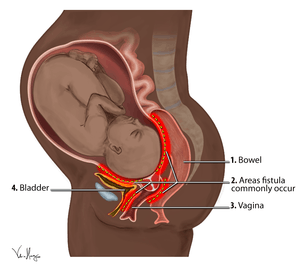
Obstetric fistula (or vaginal fistula) is a medical condition in which a fistula (hole) develops between either the rectum and vagina (see rectovaginal fistula) or between the bladder and vagina (see vesicovaginal fistula) after severe or failed childbirth, when adequate medical care is not available.[1] The United Nations Population Fund (UNFPA) defines obstetric fistula as,[2]
“A childbirth injury that has been largely neglected, despite the devastating impact it has on the lives of affected girls and women. It is usually caused by prolonged, obstructed labour, without timely medical intervention—typically an emergency Caesarean section. During unassisted, prolonged, obstructed labour, the sustained pressure of the baby’s head on the mother’s pelvic bone damages soft tissues, creating a hole—or fistula—between the vagina and the bladder and/or rectum. The pressure deprives blood flow to the tissue, leading to necrosis. Eventually, the dead tissue comes away, leaving a fistula, which causes a constant leaking of urine and/or faeces through the vagina.”
It is considered a disease of poverty because of its tendency to occur in women in poor countries who do not have health resources comparable to developed nations. An estimated 2 million women in sub-Saharan Africa, Asia, the Arab region, and Latin America and the Caribbean are living with this injury, and some 50,000 to 100,000 new cases develop each year.[3][4][5]
In developed countries, the majority of women with OF suffer rectovaginal fistula (RVF). This is caused by episiotomy and forceps/vacuum extraction of the baby from the vagina. Over 80% of RVFs in the USA are obstetric and either preventable or treatable, followed in frequency by Crohn's disease and radiation.[6]
A fistula is almost entirely preventable. According to health advocates, its persistence is a sign that health systems are failing to meet women’s essential needs.[3]
Signs and symptoms
Symptoms of obstetric fistula include:
- Flatulence, urinary or fecal incontinence, which may be continual or only happen at night[7][8][9]
- Foul-smelling vaginal discharge[8][9][10]
- Repeated vaginal or urinary tract infections[9][10][11]
- Irritation or pain in the vagina or surrounding areas[10][12][13]
- Pain during sexual activity[10][12][13]
Other effects of obstetric fistulae include stillborn babies due to prolonged labor, which happens 85% to 100% of the time,[14][15][16][17] severe ulcerations of the vaginal tract, "foot drop", which is the paralysis of the lower limbs caused by nerve damage, making it impossible for women to walk,[9][18][19] infection of the fistula forming an abscess,[10] and up to two-thirds of the women become amenorrhoeic.[5]
Obstetric fistulae have far-reaching physical, social, economic, and psychological consequences for the women affected.
General consequences
According to UNFPA, “Due to the prolonged obstructed labour, the baby almost inevitably dies, and the woman is left with chronic incontinence. Unable to control the flow of urine or faeces, or both, she may be abandoned by her husband and family and ostracized by her community. Without treatment, her prospects for work and family life are virtually non-existent.” [20]
Physical consequences
The most direct consequence of an obstetric fistula is the constant leaking of urine, feces, and blood as a result of a hole that forms between the vagina and bladder or rectum.[21] This leaking has both physical and societal penalties. The acid in the urine, feces, and blood causes severe burn wounds on the legs from the continuous dripping.[22] Nerve damage that can result from the leaking can cause women to struggle with walking and eventually lose mobility. In an attempt to avoid the dripping, women limit their intake of water and liquid which can ultimately lead to dangerous cases of dehydration. Ulceration and infections can persist, as well as kidney disease and kidney failure, which can each lead to death. Further, only a quarter of women who suffer a fistula in their first birth are able to have a living baby, and therefore have minuscule chances of conceiving a healthy baby later on. Some women, due to obstetric fistulae and other complications from childbirth, do not survive.[23]
Social consequences
Physical consequences of obstetric fistulae lead to severe sociocultural stigmatization for various reasons. For example, in Burkina Faso, most citizens do not believe an obstetric fistula to be a medical condition, but as a divine punishment or a curse for disloyal or disrespectful behavior.[24] Other sub-Saharan cultures view offspring as an indicator of a family's wealth. A woman who is unable to successfully produce children as assets for her family is believed to make her and her family socially and economically inferior. A patient's incontinence and pain also render her unable to perform household chores and childrearing as a wife and as a mother, thus devaluing her.[25] Other misconceptions about obstetric fistulae are that they are caused by venereal diseases or are divine punishment for sexual misconduct.[26]
As a result, many girls are divorced or abandoned by their husbands and partners, disowned by family, ridiculed by friends, and even isolated by health workers.[18] Divorce rates for women who suffer from an obstetric fistula range from 50%[27][28][29][30] to as high as 89%.[26] Now marginalized members of society, girls are forced to live on the edges of their villages and towns, often to live in isolation in a hut where they will likely die from starvation or an infection in the birth canal. The unavoidable odor is viewed as offensive, thus their removal from society is seen as essential. Accounts of women who suffer obstetric fistulae proclaim that their lives have been reduced to the leaking of urine, feces, and blood because they are no longer capable or allowed to participate in traditional activities, including the duties of wife and mother. Because such consequences highly stigmatize and marginalize the woman, the intense loneliness and shame can lead to clinical depression and suicidal thoughts. Some women have formed small groups and resorted to walking to seek medical help, where their characteristic odor makes them a target for sub-Saharan predatory wildlife, further endangering their lives. This trip can take on average 12 hours to complete.[31] Moreover, women are sometimes forced to turn to commercial sex work as a means of survival because the extreme poverty and social isolation that result from obstetric fistulae eliminate all other income opportunities. With only 7.5% of women with fistulae able to access treatment, the vast majority of women end up with the consequences of obstructed and prolonged labor simply because options and access to help is so limited.[32]
Psychological consequences
Some common psychological consequences that people with a fistula face are the despair from losing their child, the humiliation from their smell, and inability to perform their family roles.[15] Additionally, a fear of developing another fistula in future pregnancies exists.[33]
Causes
In the developed world, like the USA, the number one cause of obstetric fistulae, particularly RVF, is the use of episiotomy and forceps,[6] In less-developed countries, obstetric fistulae usually develop as a result of prolonged labor when a cesarean section cannot be obtained. Over the course of the three to five days of labor, the unborn child presses against the mother's vagina very tightly, cutting off blood flow to the surrounding tissues between the vagina and the rectum and between the vagina and the bladder, causing the tissues to disintegrate and rot away.[5][9][18]
Obstetric fistulae can also be caused by poorly performed abortions,[34] and pelvic fracture, cancer, or radiation therapy targeted at the pelvic area, inflammatory bowel disease (such as Crohn's disease and ulcerative colitis). Other potential causes for the development of obstetric fistulae are sexual abuse and rape, especially in conflict/postconflict areas,[35] and other trauma, such as surgical trauma.[18][36]
Risk factors
Primary risk factors in the USA and other developed countries are the use of episiotomy and forceps.[4] Primary risk factors include early or closely spaced pregnancies and lack of access to emergency obstetric care. For example, a 1983 study in Nigeria found that 54.8% of the victims were under 20 years of age, and 64.4% gave birth at home or in poorly equipped local clinics.[37] When available at all, cesarean sections and other medical interventions are usually not performed until after tissue damage has already been done.
Indirect causes
Social, political, and economic causes that indirectly lead to the development of obstetric fistulae concern issues of poverty, malnutrition, lack of education, early marriage and childbirth, the role and status of women in developing countries, harmful traditional practices, sexual violence, and lack of good quality or accessible maternal and health care.[9][18][23][38]
Poverty
Poverty is the number one indirect cause of obstetric fistulae around the world. As obstructed labor and obstetric fistulae account for 8% of maternal deaths worldwide[39] and “a 60-fold difference in gross national product per person shows up as a 120-fold difference in maternal mortality ratio,” it is clear that impoverished countries produce higher maternal mortality rates and thus higher obstetric fistula rates.[40] Furthermore, impoverished countries not only have low incomes, but also lack adequate infrastructure, trained and educated professionals, resources, and a centralized government that exist in developed nations to effectively eradicate obstetric fistulae.[41]
According to UNFPA, “Generally accepted estimates suggest that 2-3.5 million women live with obstetric fistulae in the developing world, and between 50,000 and 100,000 new cases develop each year. All but eliminated from the developed world, obstetric fistula continues to affect the poorest of the poor: women and girls living in some of the most resource-starved remote regions in the world.” [42]
Malnutrition
One reason that poverty produces such high rates of fistula cases is the malnutrition that exists in such areas.[23] Lack of money and access to proper nutrition,[43] as well as vulnerability to diseases that exist in impoverished areas because of limited basic health care and disease prevention methods, cause inhabitants of these regions to experience stunted growth. Sub-Saharan Africa is one such environment where the shortest women have on average lighter babies and more difficulties during birth when compared with full-grown women. This stunted growth causes expectant mothers to have skeletons unequipped for proper birth, such as an underdeveloped pelvis.[23] This weak and underdeveloped bone structure increases the chances that the baby will get stuck in the pelvis during birth, cutting off circulation and leading to tissue necrosis. Because of the correlation between malnutrition, stunted growth, and birthing difficulties, maternal height can at times be used as a measure for expected labor difficulties.[40]
Lack of education
High levels of poverty also lead to low levels of education among impoverished women concerning maternal health. This lack of information in combination with obstacles preventing rural women to easily travel to and from hospitals lead many to arrive at the birthing process without prenatal care. This can cause a development of unplanned complications that may arise during home births, in which traditional techniques are used. These techniques often fail in the event of unplanned emergencies, leading women to go to hospital for care too late, desperately ill, and therefore vulnerable to the risks of anesthesia and surgery that must be used on them. In a study of women who had prenatal care and those who had unbooked emergency births, “the death rate in the booked-healthy group was as good as that in many developed countries, [but] the death rate in the unbooked emergencies was the same as the death rate in England in the 16th and 17th centuries.” In this study, 62 unbooked emergency women were diagnosed with obstetric fistulae out of 7,707 studied, in comparison to three diagnosed booked mothers out of 15,020 studied.[40] In addition, studies find that education is associated with lower desired family size, greater use of contraceptives, and increased use of professional medical services. Educated families are also more likely to be able to afford health care, especially maternal healthcare.[44]
Early marriages and early childbirth
In sub-Saharan Africa, many girls enter into arranged marriages soon after menarche (usually between the ages of 9 and 15). Social factors and economic factors contribute to this practice of early marriages. Socially, some grooms want to ensure their brides are virgins when they get married, so an earlier marriage is desirable.[43] Economically, the bride price received and having one less person to feed in the family helps alleviate the financial burdens of the bride's family.[45] Early marriages lead to early childbirth, which increases the risk of obstructed labor, since young mothers who are poor and malnourished may have underdeveloped pelvises. In fact, obstructed labor is responsible for 76 to 97% of obstetric fistulae.[14]
Lack of quality maternal healthcare
Even women who do make it to the hospital may not get proper treatment. Countries that suffer from poverty, civil and political unrest or conflict, and other dangerous public health issues such as malaria, HIV/AIDS, and tuberculosis often suffer from a severe burden and breakdown within the healthcare system. This breakdown puts many people at risk, specifically women. Many hospitals within these conditions suffer from shortages of staff, supplies, and other forms of medical technology that would be necessary to perform reconstructive obstetric fistula repair.[46] There is a shortage of doctors in rural Africa, and studies find that the doctors and nurses who do exist in rural Africa often do not show up for work.[44]
Poverty hinders women from being able to access normal and emergency obstetric care because of long distances and expensive procedures. For some women, the closest maternal care facility can be more than 50 km away. In Kenya, a study by the Ministry of Health found that the "rugged landscape, long distances to health facilities, and societal preferences for delivery with a traditional birth attendant contributed to delays in accessing necessary obstetric care."[47] Emergency cesarean sections, which can help avoid fistulae caused by prolonged vaginal deliveries, are very expensive.
Role and status of women
In developing countries, women who are affected by obstetric fistulae do not necessarily have full agency over their bodies or their households. Rather, their husbands and other family members have control in determining the healthcare that the women receive.[23] For example, a woman's family may refuse medical examinations for the patient by male doctors, but female doctors may be unavailable, thus barring women from prenatal care.[43] Furthermore, many societies believe that women are supposed to suffer in childbirth, thus are less inclined to support maternal health efforts.[44]
Prevention
Prevention is the key to ending fistulae. UNFPA states that, “Ensuring skilled birth attendance at all births and providing emergency obstetric care for all women who develop complications during delivery would make fistula as rare in developing countries as it is in the industrialized world.” [3] In addition, access to health services and education – including family planning, gender equality, higher living standards, child marriage, and human rights must be addressed to reduce the marginalization of women and girls. Reducing marginalization in these areas could reduce maternal disability and death by at least 20%.[3]
Prevention comes in the form of access to obstetrical care, support from trained health care professionals throughout pregnancy, providing access to family planning, promoting the practice of spacing between births, supporting women in education, and postponing early marriage. Fistula prevention also involves many strategies to educate local communities about the cultural, social, and physiological factors of that condition and contribute to the risk for fistulae. One of these strategies involves organizing community-level awareness campaigns to educate women about prevention methods such as proper hygiene and care during pregnancy and labor.[48] Prevention of prolonged obstructed labor and fistulae should preferably begin as early as possible in each woman's life. For example, improved nutrition and outreach programs to raise awareness about the nutritional needs of children to prevent malnutrition, as well as improve the physical maturity of young mothers, are important fistula prevention strategies. It is also important to ensure access to timely and safe delivery during childbirth: measures include availability and provision of emergency obstetric care, as well as quick and safe cesarean sections for women in obstructed labor. Some organizations train local nurses and midwives to perform emergency cesarean sections to avoid vaginal delivery for young mothers who have underdeveloped pelvises.[31] Midwives located in the local communities where obstetric fistulae are prevalent can contribute to promoting health practices that help prevent future development of obstetric fistulae. NGOs also work with local governments, like the government of Niger, to offer free cesarean sections, further preventing the onset of obstetric fistulae.[23]
Promoting education for girls is also a key factor to preventing fistulae in the long term. Former fistula patients often act as "community fistula advocates" or "ambassadors of hope," a UNFPA-sponsored initiative, to educate the community.[49] These survivors help current patients, educate pregnant mothers, and dispel cultural myths that obstetric fistulae are caused by adultery or evil spirits.[36][50][51] Successful ambassador programs are in place in Kenya, Bangladesh, Nigeria, Ghana, Côte d'Ivoire, and Liberia.[23]
Several organizations have developed effective fistula prevention strategies. One, the Tanzanian Midwives Association, works to prevent fistulae by improving clinical healthcare for women, encouraging the delay of early marriages and childbearing years, and helping the local communities to advocate for women's rights.[52]
Treatment
The nature of the injury varies depending on the size and location of the fistula, so a surgeon with experience is needed to improvise on the spot.[53] Before the patient undergoes surgery, treatment and evaluation are needed for conditions including anemia, malnutrition, and malaria. Quality treatment in low-resource settings are possible (as in the cases of Nigeria and Ethiopia).[18] Treatment is available through reconstructive surgery.[54] Primary fistula repair has a 91% success rate.[45] The corrective surgery alone costs about US$100 – 400,[55] and the cost for the entire procedure, which includes the actual surgery, postoperative care, and rehabilitation support, is estimated to cost $300–450. Initial surgeries done by inadequately trained doctors and midwives increase the number of follow-up surgeries that must be performed to restore full continence.[45] Successful surgery enables women to live normal lives and have more children, but it is recommended to have a cesarean section to prevent the fistula from recurring. Postoperative care is vital to prevent infection. Some women are not candidates for this surgery due to patient comorbidity or disease-related factors. In those cases, fecal diversion can help the patient, but not necessarily cure them.[56] Physical therapy is also crucial to the rehabilitation process, both before and after the surgery, to help patients adjust.
Besides physical treatment, mental health services are also needed to rehabilitate fistula patients, who experience psychological trauma from being ostracized by the community and from fear of developing fistulae again. A study on the first formal counseling program for fistula survivors in Eritrea shows positive results, whereby counseling significantly improved the women's self-esteem, knowledge about fistulae and fistula prevention, and behavioral intentions for "health maintenance and social reintegration" following surgery.[57]
Challenges
Challenges with regards to treatment include the very high number of women needing reconstructive surgery, access to facilities and trained surgeons, and the cost of treatment. For many women, US$300 is an impossible price and they cannot afford the surgery. Access and availability of treatment also vary widely across different sub-Saharan countries. Certain regions also do not have enough maternal care clinics that are equipped, willing to treat fistula patients, and adequately staffed. At the Evangelical Hospital of Bemberéke in Benin, only one expatriate volunteer obstetrics and gynecology doctor is available a few months per year, with one certified nurse and seven informal hospital workers.[58] In all of Niger, two medical centers treat fistula patients.[45] In Nigeria, more dedicated health professionals operate on up to 1,600 women with a fistula per year.[59] The world is currently severely under capacity for treating the problem; it would take up to 400 years to treat the backlog of patients.[5] To prevent any new cases of obstetric fistulae, about 75,000 new emergency obstetric care facilities would have to be built in Africa alone,[60] plus an increase in financial support and an even higher number of certified doctors, midwives, and nurses needed.
Another challenge standing between women and fistula treatment is information. Most women have no idea that treatment is available. Because this is a condition of shame and embarrassment, most women hide themselves and their condition and suffer in silence. In addition, after receiving initial treatment, health education is important to prevent fistulae in subsequent pregnancies.[18]
Another challenge is the lack of trained professionals to provide surgery for fistula patients. As a result, nonphysicians are sometimes trained to provide obstetric services. For example, the Addis Ababa Fistula Hospital has medical staff without formal degrees, and one of its top surgeons was illiterate, but she had been trained over years and now regularly successfully performs fistula surgery.[44]
Catheterization
Fistula cases can also be treated through urethral catheterization if identified early enough. The Foley catheter is recommended because it has a balloon to hold it in place. The indwelling Foley catheter drains urine from the bladder. This decompresses the bladder wall so that the wounded edges come together and stay together, giving it a greater chance of closing naturally, at least in the smaller fistulae.
According to data collected by Dr Kees Waaldijk, Director of the Nigeria National Fistula Programme, out of a case series of 4424 patients with obstetric fistulae who were treated within 75 days post partum, 37% (1579 patients) are cured completely with the use of a Foley catheter without the need of surgery. Even without preselecting the least complicated obstetric fistula cases, the systematic use of a Foley catheter by midwives after the onset of urinary incontinence could cure over 25% of all new fistula cases each year without the need for surgery.[60]
Epidemiology

Obstetric fistulae were very common throughout the world, but since the late 19th century, the rise of gynecology developed safe practices for childbirth, including giving birth at local hospitals rather than at home, which dramatically reduced rates of obstructed labor and obstetric fistulae in Europe and North America.[45][61] The surgery to cure it was developed by J. Marion Sims and perfected by Australian doctors Reg and Catherine Hamlin of the Addis Ababa Fistula Hospital,[62] now the largest fistula repair center in the world.[17]
Adequate population-based epidemiological data on obstetric fistulae are lacking due to the historic neglect of this condition since it was mostly eradicated in developed nations. Available data are estimations that should be viewed with caution.[18] About 30% of women over age 45 in developed nations are affected by urinary incontinence, primarily caused by obstetric fistulae.[45] The rate of obstetrical fistulae is much lower in places that discourage early marriage, encourage and provide general education for women, and grant women access to family planning] and skilled medical teams to assist during childbirth.[58]
Obstetric fistulae are still very prevalent in the developing world, especially in sub-Saharan Africa (Kenya,[63] Mali, Niger,[45] Nigeria, Rwanda, Sierra Leone, South Africa, Benin, Chad, Malawi, Mali, Mozambique, Niger, Nigeria, Uganda, and Zambia) and much of South Asia (Afghanistan, Bangladesh, India, Pakistan, and Nepal). According to the World Health Organization (WHO), an estimated 50,000 to 100,000 women develop obstetric fistulae each year and over two million women currently live with an obstetric fistula.[64] In particular, most of the two million-plus women in developing nations who suffer from obstetric fistulae are under the age of 30.[45] Between 50 and 80% of women under the age of 20 in poor countries develop obstetric fistulae (the youngest patients are 12–13 years old).[43] Other estimates indicate about 73,000 new cases occur per year.[65]
Society and culture
During most of the 20th century, obstetric fistulae were largely missing from the international global health agenda. This is reflected by the fact that the condition was not included as a topic at the landmark United Nations 1994 International Conference on Population and Development (ICPD).[66] The 194-page report from the ICPD does not include any reference to obstetric fistulae. In 2000, eight Millennium Development Goals were adopted after the United Nations Millennium Summit to be achieved by 2015. The fifth goal of improving maternal health is directly related to obstetric fistula. Since 2003, obstetric fistula has been gaining awareness amongst the general public and has received critical attention from UNFPA, who has organized a global "Campaign to End Fistula."[67] New York Times columnist Nicholas Kristof, a Pulitzer Prize–winning writer, wrote several columns in 2003, 2005, and 2006[68] focusing on fistula and particularly treatment provided by Catherine Hamlin at the Fistula Hospital in Ethiopia. In 2007, Fistula Foundation, Engel Entertainment, and a number of other organizations including PBS NOVA released the documentary film, A Walk to Beautiful, which traced the journey of five women from Ethiopia who sought treatment for their obstetric fistulae at the Addis Ababa Fistula Hospital in Ethiopia. The film still airs frequently on PBS in the U.S. and is credited with increasing awareness of obstetric fistulae greatly. Increased public awareness and corresponding political pressure have helped fund the UNFPA's Campaign to End Fistula, and helped motivate the United States Agency for International Development to dramatically increase funding for the prevention and treatment of obstetric fistulae.
Countries that signed the United Nations Millennium Declaration have begun adopting policies and creating task forces to address issues of maternal morbidity and infant mortality, including Tanzania, Democratic Republic of Congo, Sudan, Pakistan, Bangladesh, Burkina Faso, Chad, Mali, Uganda, Eritrea, Niger, and Kenya. Laws to increase the minimum age for marriage have also been enacted in Bangladesh, Nigeria, and Kenya. To monitor these countries and hold them accountable, the UN has developed six "process indicators", a benchmark tool with minimum acceptable levels that measures whether or not women receive the services they need.[23]
The UNFPA set out several strategies to address fistulae, including "postponing marriage and pregnancy for young girls, increasing access to education and family planning services for women and men, provide access to adequate medical care for all pregnant women and emergency obstetric care for all who develop complications, and repairing physical damage through medical intervention and emotional damage through counselling."[69] One of the UNFPA's initiatives to reduce the cost of transportation in accessing medical care provided ambulances and motorcycles for women in Benin, Chad, Guinea, Guinea-Bissau, Kenya, Rwanda, Senegal, Tanzania, Uganda, and Zambia.[23]
Campaign to end fistula
The Addis Ababa Fistula Hospital in Ethiopia successfully treats women with obstetric fistulae, even in less than desirable environments. As a result, the UNFPA gathered partners in London in 2001, and officially launched an international initiative to address obstetric fistulae later in 2003. Partners in this initiative include Columbia University's Averting Maternal Death and Disability Program, the International Federation of Gynecology and Obstetrics, and the World Health Organization. The official international partnership formed by the Campaign to End Fistula is named the Obstetric Fistula Working Group (OFWG) and its purpose is to coordinate and collaborate global efforts to eliminate obstetric fistulae.[18]
The first thing that the initiative did was to quantitatively assess the issue in countries where the prevalence is suspected to be high, including nine countries in sub-Saharan Africa. The studies found that fistula patients are mostly illiterate, young, and poor women. Moreover, local legislators and government officials' lack of awareness exacerbate the problem.[58][70] The OFWG improves awareness for prenatal and neonatal care and develops strategies for clinically managing obstetric fistula cases.[18]
To date, the Campaign to End Fistula has involved more than 30 countries in sub-Saharan Africa, South Asia, and the Middle East, and completed rapid needs assessments in many of those countries to continually assess the needs in each country. The national strategies that the campaign helps each nation to develop are three-fold: prevention of new cases, treatment for patients, and support for reintegration into society after the operation. Prevention efforts include access to maternal health services and mobilizing communities and legislators to increase awareness of maternal health problems. Training health providers and ensuring affordable treatment services, as well as providing social services such as health education and mental health services, help treat and reintegrate women into their communities. Other tasks undertaken by the campaign include fundraising and introducing new donors and gathering new partners of all perspectives, such as faith-based organizations, NGOs, and private-sector companies.[18]
Fistula Foundation
Fistula Foundation is a U.S. based organization dedicated to treating obstetric fistula in more than 20 countries throughout sub-Saharan Africa and Southeast Asia. Its CEO is Kate Grant.[71] The organization focuses its funding entirely on treatment, primarily via fistula repair surgeries, which cost as little as $586 on average. Fistula Foundation also funds training for surgeons and fistula care providers, as well as funds to upgrade facilities to enable providers to give the best care possible to women seeking treatment. To date, the organization has funded nearly 18,000 obstetric fistula surgeries since changing its mission in 2009,[72] making it the largest provider of obstetric fistula surgeries of any other organization not accepting government funding.[72]
Fistula Fortnight
The Fistula Fortnight was a two-week initiative that took place from February 21 to March 6, 2005, where fistula experts treated fistula patients for free at four surgical camps in the northern Nigerian states of Kano, Katsina, Kebbi, and Sokoto. The initiative was collaborated by many partners such as the federal and state governments of Nigeria, 13 Nigerian fistula surgeons, the Nigerian Red Cross, and UNFPA. During the nine-month preparation period, facilities were renovated, equipment were provided, and staff were extensively trained to treat fistula.[18] The goals of this initiative were to alleviate the backlog of patients waiting for surgery, provide treatment services at host sites, and to raise awareness for maternal health.
The Fistula Fortnight treated 569 women at no cost, with an 87.8% rate of successful closures. Follow-up treatments and services were provided, such as bed rest, analgesics, oral fluids, visual monitoring of urination by nurses, a catheter, catheter removal, and an examination and discharge from the hospital at a minimum of four weeks, with instruction to avoid sexual intercourse. The Fistula Fortnight also had preoperative and postoperative counseling provided by nurses and social workers and held health education workshops for fistula patients and their families.[73]
Community organizations
Recovering fistula patients in the postoperative period need support to fully reintegrate into society. In particular, physical labor is limited in the first year of recovery, so women need alternative ways to earn an income.[33] Since poverty is an indirect cause of obstetric fistulae, some community organizations aim to provide postoperative services to enhance the women's socioeconomic situation. Delta Survie, located in Mopti, Mali, is a community center that provides skills training and helps women to produce hand-made jewelry to generate income and meet other women while they recover.[74] Another organization, IAMANEH Suisse, identifies Malian fistula patients, facilitates operations for those without the financial means, and helps them access follow-up services to prevent recurrence of fistulae in their subsequent pregnancies.[75]
Other organizations also help to arrange mission trips for medical personnel to visit countries with women affected by fistulae, perform surgeries, and train local doctors to give medical assistance for fistula patients. The International Organization for Women and Development (IOWD) is one such nonprofit organization. The IOWD hosts four to five mission trips per year to provide relief to obstetric fistula patients in West Africa. IOWD mission trip members have evaluated thousands of patients at no cost and performed surgeries for over a thousand women.[45]
Notable treatment centers
The Addis Ababa Fistula Hospital in Ethiopia is the largest center in the world and the only one dedicated exclusively to comprehensive fistula treatment. Four more sister hospitals have been opened in other parts of Ethiopia.
The newest treatment center is the Danja Fistula Center in Danja, Niger, opened by the Worldwide Fistula Fund in February 2012. Danja Fistula Center, like the Addis Ababa Fistula Hospital, is funded in part by Fistula Foundation[76] and offers free surgery and postoperative care to fistula patients in western Africa. Along with comprehensive treatment services, Danja Fistula Center also provides social reintegration services, prevention outreach and education, and acts as a training and research center for medical personnel.
The latest treatment centre is being built in Kenya by MaterCare International (www.MaterCare.org).
See also
References
- ↑ Creanga, A. A.; R.R. Genadry (November 2007). "Obstetric fistulas: A clinical review". International Journal of Gynecology & Obstetrics. 99 (Supplement 1): S40. doi:10.1016/j.ijgo.2007.06.030.
- ↑ "When Pregnancy Harms: Obstetric Fistula". UNFPA. 2012.
- 1 2 3 4 http://www.unfpa.org/obstetric-fistula
- 1 2 https://www.fascrs.org/core-subject/rectovaginal-fistula-and-rectourethral-fistula
- 1 2 3 4 Browning, Andrew. "Obstetric Fistula In Ilorin, Nigeria." Plos Medicine 1.1 (2004): 022-024. Academic Search Complete. Web. 25 Oct. 2012.
- 1 2 http://www.fascrs.org/core-subject/rectovaginal-fistula-and-rectourethral-fistula
- ↑ Creanga, A.A.; R.R. Genadry (November 2007). "Obstetric fistulas: A clinical review". International Journal of Gynecology & Obstetrics. 99 (Supplement 1): S42. doi:10.1016/j.ijgo.2007.06.021.
- 1 2 "Women's Health." Vaginal Fistula Causes, Symptoms, & Treatments. WebMD, n.d. Web. 22 Oct. 2012. <http://women.webmd.com/tc/vaginal-fistula-topic-overview>
- 1 2 3 4 5 6 "Obstetric Fistula." Our Bodies Ourselves Health Resource Center. Our Bodies Ourselves Health Resource Center, n.d. Web. 22 Oct. 2012. <http://www.ourbodiesourselves.org/book/companion.asp?id=22>
- 1 2 3 4 5 "Rectovaginal Fistula." Mayo Clinic. Mayo Foundation for Medical Education and Research, 29 May 2010. Web. 22 Oct. 2012. <http://www.mayoclinic.com/health/rectovaginal-fistula/DS01065/DSECTION=symptoms>
- ↑ Champagne BJ, et al. (2010). "Rectovaginal fistula". The Surgical Clinics of North America. 90: 69–82. doi:10.1016/j.suc.2009.09.003.
- 1 2 Novi JM, et al. (2005). "Rectovaginal fistula". Journal of Pelvic Medicine & Surgery. 11: 283–293. doi:10.1097/01.spv.0000190848.17284.d3.
- 1 2 Wong M, Ozel B (2010). Fistulae. In Management of Common Problems in Obstetrics and Gynecology, 5th ed., pp. 328-332. Chichester: Wiley-Blackwell.
- 1 2 Semere, L. & Nour, N.M. (2008). Obstetric fistula: Living with incontinence and shame. Reviews in Obstetrics & Gynecology, 1(4), 193-197.
- 1 2 Ahmed, S., & Holtz, S.A. (2007). Social and economic consequences of obstetric fistula: Life changes forever? International Journal of Gyne - cology & Obstetrics, 99, S10-S15.
- ↑ Wall L.L. (2006). "Obstetric vesicovaginal fistula as an international public health problem". Lancet. 368: 1201–1209. doi:10.1016/s0140-6736(06)69476-2.
- 1 2 Zheng, A.X., & Anderson, F.W. (2009). Obstetric fistula in low-income countries. International Journal of Gynecology & Obstetrics, 104(2), 85- 89.
- 1 2 3 4 5 6 7 8 9 10 11 12 Donnay F., Ramsey K. (2006). "Eliminating obstetric fistula: Progress in partnerships, International". Journal of Gynecology & Obstetrics. 94 (3): 254–261. doi:10.1016/j.ijgo.2006.04.005.
- ↑ Arrowsmith S, Hamlin EC, Wall LL (1996). "Obstructed labor injury complex: obstetric fistula formation and the multifaceted morbidity of maternal birth trauma in the developing world". Obstet Gynecol Surv. 51 (9): 568–74. doi:10.1097/00006254-199609000-00024.
- ↑ http://www.unfpa.org/sites/default/files/resource-pdf/Fistula%20brochure-May14_0.pdf
- ↑ "Fast Facts & FAQ's". The Fistula Foundation. Retrieved April 10, 2012.
- ↑ Kristoff, Nicholas D. (2010). Half the Sky. New York: First Vintage Books.
- 1 2 3 4 5 6 7 8 9 Brodman Michael; et al. (2011). "Obstetric Fistula In Low And Middle Income Countries". Mount Sinai Journal of Medicine. 78 (3): 352–361.
- ↑ Burkina Faso Ministry of Health and UNFPA. Sociocultural study on obstetric fistula. Ouagadougou.
- ↑ Lita, Ana (8 March 2008). "Obstetric Fistula: A Dire Consequence of Child Marriage". International Humanist and Ethical Union.
- 1 2 Roush K. M. (2009). "Social implications of obstetric fistula: An integrative review". Journal of Midwifery and Women’s Health. 54 (2): e21–33. doi:10.1016/j.jmwh.2008.09.005.
- ↑ Hilton P, Ward A (1998). "Epidemiological and surgical aspects of urogenital fistula: A review of 25 years experience in south-west Nigeria". Int Urogynecol J Pelvic Floor Dysfunct. 9: 189–194. doi:10.1007/bf01901602.
- ↑ Kelly J.; Kwast B. (1993). "Epidemiological study of vesicovaginal fi stulas in Ethiopia". Int Urogyn J. 4: 271–273.
- ↑ Tahzib F (1983). "Epidemiological determinants of vesico-vaginal fistulas". Brit J Obstet Gynecol. 90: 387–391.
- ↑ Ampofo K.; Out T.; Uchebo G. (1990). "Epidemiology of vesico-vaginal fi stulas in northern Nigeria". W Afr Med J. 9: 98–102.
- 1 2 McKinney, T. B. (2006). Fistula women of Africa: The horror of their lives, and hope for their tomorrow. The International Organization for Women and Development. Lecture presented October 2006, Phoenix, AZ.
- ↑ Charlotte Warren; Annie Mwangi (December 2008). "Obstetric Fistula: Can Community Midwives Make a Difference?". UNFPA.
- 1 2 Pope Rachel; Bangser Maggie; Harris Requejo Jennifer (2011). "Restoring Dignity: Social Reintegration After Obstetric Fistula Repair In Ukerewe, Tanzania". Global Public Health. 6 (8): 859–873. doi:10.1080/17441692.2010.551519.
- ↑ Hilton P. Vesico-vaginal fistulas in developing countries. Int J Gynecol Obstet 2003;82:285—95.
- ↑ Keeton C (2004). "Sexual abuse on the rise in Africa—governments must act". Bull WHO. 82: 313.
- 1 2 The ACQUIRE Project. Traumatic gynecologic fistula as a consequence of sexual violence in conflict settings: a literature review. New York7 The ACQUIRE Project/EngenderHealth; 2005.
- ↑ "Epidemiological determinants of vesicovaginal fistulas". BJOG: An International Journal of Obstetrics & Gynaecology. 90 (5): 387–391. May 1983. doi:10.1111/j.1471-0528.1983.tb08933.x.
- ↑ Miller J, Lester F, Webster M, et al. (2005). "Obstetric fistula: a preventable tragedy". J Midwifery Womens Health. 50: 286–294. doi:10.1016/j.jmwh.2005.03.009. PMID 15973264.
- ↑ Hofmeyr GJ. Obstructed labor: using better technologies to reduce mortality Int J Gynecol Obstet 2004;85(Supp. 1): s62—72.
- 1 2 3 John Middleton; Joseph C. Miller (2008). "Childbearing". New Encyclopedia of Africa. 1: 363–370. Retrieved 10 April 2012.
- ↑ Chandiramani, Payal. "Programmatic and Policy Recommendations for Addressing Obstetric Fistula and Uterine Prolapse | Wilson Center." Wilson Center. The Woodrow Wilson International Center for Scholars, 27 Sept. 2012. Web. 27 Nov. 2012. <http://www.wilsoncenter.org/event/programmatic-and-policy-recommendations-for-addressing-obstetric-fistula-and-uterine-prolapse>
- ↑ http://www.unfpa.org/sites/default/files/resource-pdf/EN-SRH%20fact%20sheet-Fistula.pdf
- 1 2 3 4 Cook R.J.; Dickens B.M.; Syed S. (2004). "Obstetric fistula: the challenge to human rights". International Journal of Gynecology & Obstetrics. 87 (1): 72–77. doi:10.1016/j.ijgo.2004.07.005.
- 1 2 3 4 Kristof, Nicholas D., and Sheryl WuDunn. Half the Sky: Turning Oppression into Opportunity for Women Worldwide. New York: Alfred A. Knopf, 2009. Print.
- 1 2 3 4 5 6 7 8 9 McKinney Timothy; et al. (2010). "The Fistula Crisis In Sub-Saharan Africa: An Ongoing Struggle In Education And Awareness". Urologic Nursing. 30 (6): 341–346.
- ↑ Rai, Devkumari Shrestha. "Women Living with Obstetric Fistula and Nurses’ Role in Preventive Measures." International Journal of Nursing and Midwifery 3.9 (2011): 150-53.
- ↑ Kenya Ministry of Health and UNFPA. Needs assessment of obstetric fistula in selected districts of Kenya; 2004.
- ↑ "A Tragic Failure to Deliver Maternal Care". UNFPA. Retrieved 17 April 2012.
- ↑ United Nations Population Fund, Campaign to End Fistula. The Maternal Health Thematic Fund Annual Report 2010: Campaign to End Fistula. http://www. endfistula.org/publications.htm. Accessed November 2012.
- ↑ Wegner MN, Runinjo J, Sinclair E, et al. Improving community knowledge of obstetric fistula prevention and treatment. Int J Gynaecol Obstet 2007; 99(suppl 1): S108–S111.
- ↑ Hamlin EC, Muleta M, Kennedy RC. "Providing an obstetric fistula service. BJU Int 2002; 89(suppl 1): 50–53.
- ↑ Miller S, Lester F, Webster M, Cowan B (2005). "Obstetric fistula: a preventable tragedy". J Midwifery Womens Health. 50 (4): 286–94. doi:10.1016/j.jmwh.2005.03.009. PMID 15973264.
- ↑ Wall L, Arrowsmith SD, Briggs ND, et al. (2005). "The obstetric vesicovaginal fistula in the developing world". Obstet Gynecol Surv. 60 (7 suppl 1): S3–51.
- ↑ "Removing Obstacles to Increased Treatment". The Fistula Foundation. Retrieved 17 April 2012.
- ↑ Nathan, L.M., Rochat, C.H., Grigorescu, B., & Banks, E. (2009). Obstetric fistulae in West Africa: Patient perspectives. American Journal of Obstetrics & Gynecology 200(5), e40-e42.
- ↑ Galandiuk S, Kimberling J, Al-Mishlab TG, et al. (2005). "Perianal Crohn disease: predictors of need for permanent diversion". Ann. Surg. 241 (5): 796–801. doi:10.1097/01.sla.0000161030.25860.c1.
- ↑ Johnson KA, Turan JM, Hailemariam L, Mengsteab E, Jena D, Polan ML (2010). "The role of counseling for obstetric fistula patients: Lessons learned from Eritrea". Patient Education and Counseling. 80 (2): 262–265. doi:10.1016/j.pec.2009.11.010.
- 1 2 3 United Nations Population Fund (UNPFA) & EngenderHealth (2003). Obstetric fistula needs assessment report: Findings from nine African countries. Retrieved from www.unfpa.org/fistula/docs/fistula-needsassessment. pdf
- ↑ UNFPA (2002) The second meeting of the working group for the prevention and treatment of obstetric fistula, Addis Ababa, 30 October–1 November 2002. Available: http://www.unfpa.org/upload/lib_pub_fi le/146_fi lename_fi stula_kgroup02.pdf. Accessed 9 August 2004.
- 1 2 Waaldjik K (1998) Evaluation report XIV on VVF projects in northern Nigeria and Niger. Katsina (Nigeria): Babbar Ruga Fistula Hospital. 27 p.
- ↑ "Fast Facts & FAQs". Fistula Foundation. Retrieved 17 April 2012.
- ↑ Catherine Hamlin, The Hospital by the River, Bolinda Publishing, ISBN 9781742676661
- ↑ "Sadar, Pina, Waweru, Wambui: Alive Again (2010)". Deutsche Welle Akademie. Retrieved 23 August 2012.
- ↑ Obstetric Fistulae: A Review of Available Information, 1991; WHO/MCH/MSM/91.5
- ↑ Abou Zahr C. Global burden of maternal death and disability. Br Med Bull 2003;67(1):1 – 11.
- ↑ "Report of the ICPD (94/10/18)". Retrieved 17 April 2012.
- ↑ "Obstetric Fistula". UNFPA. Retrieved 17 April 2012.
- ↑ Kristof, Nicholas (16 May 2003). "Alone and Ashamed". The New York Times. Retrieved 17 April 2012.
- ↑ UNFPA Campaign to End Fistula: "Fast Facts" (www.unfpa.org/fi stula/facts. htm).
- ↑ UNFPA. The second meeting of the Working Group for the Prevention and Treatment of obstetric fistula. New York: UNFPA; 2003.
- ↑ https://www.fistulafoundation.org/team-members/kate-grant/
- 1 2 http://www.fistulafoundation.org
- ↑ K. Ramsey, Z. Iliyasu, L. Idoko, Fistula Fortnight: Innovative partnership brings mass treatment and public awareness towards ending obstetric fistula, International Journal of Gynecology & Obstetrics, Volume 99, Supplement 1, November 2007, Pages S130-S136, ISSN 0020-7292, 10.1016/j.ijgo.2007.06.034.
- ↑ Sankare I. Contribution to the development of a mechanism for autonomous social for women with fistula in the region of Mopti. Proceedings of the meeting making motherhood safer by addressing obstetric fistula. Johannesburg, South Africa, 23—26 October; 2005.
- ↑ Kadiatou K. Prevention of obstetric fistula and support to women identified in Se´gou, Mali. proceedings of the meeting making motherhood safer by addressing obstetric fistula. Johannesburg, South Africa, 23—26 October; 2005.
- ↑ http://www.fistulafoundation.org/financials/grantees/
External links
- Fistula Foundation www.fistulafoundation.org
- Obstetric fistula at DMOZ
- Worldwide Fistula Fund homepage
- Fistula Care
- Nicholas D. Kristof reporting from the Danja Fistula Center, Niger, New York Times, 14 July 2013 (retrieved 16 July 2013)
- "James Marion Sims (1813-1883)" by A. Andrei at the Embryo Project Encyclopedia