VistA
The Veterans Information Systems and Technology Architecture (VistA) is a nationwide information system and Electronic Health Record (EHR) developed by the U.S. Department of Veterans Affairs (VA) throughout the U.S. to all 1200+ healthcare sites of the Veterans Health Administration (VHA).[1] The VHA manages the largest integrated healthcare network in the United States,[2] providing care to over 8 million veterans, employing 180,000 medical personnel and operating 163 hospitals, over 800 clinics, and 135 nursing homes throughout the continental U.S., Alaska, and Hawaii on a single electronic healthcare information network.[3]
VISTA consists of nearly 180 applications for clinical, financial, administrative, and infrastructure needs in VA integrated into a single, common database, permitting all VA applications to share one single, authoritative data source for all veteran-related care and services. The U.S. Congress has mandated the VA keep all veterans health information in one single authoritative system, and has mandated VISTA as this role.
Over 60% of all physicians trained in the U.S. rotate through the VHA on clinical electives, making VistA the most familiar and widely used EHR in the U.S. Nearly half of all U.S. hospitals that have a complete inpatient/outpatient enterprise-wide implementation of an EHR are VA hospitals using VistA.[4][5]
Features
The Department of Veterans Affairs (VA) has had automated data processing systems, including extensive clinical and administrative capabilities, within its medical facilities since before 1985.[6] Initially called the Decentralized Hospital Computer Program (DHCP) information system, DHCP was enshrined as a recipient of the Computerworld Smithsonian Award for best use of Information Technology in Medicine in 1995.
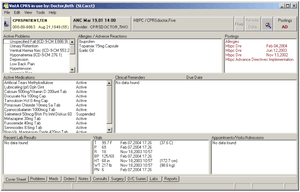
VistA supports both ambulatory and inpatient care, and includes several significant enhancements to the original DHCP system. The most significant is a graphical user interface for clinicians known as the Computerized Patient Record System (CPRS), which was released in 1997. In addition, VistA includes computerized order entry, bar code medication administration, electronic prescribing, and clinical guidelines.
CPRS provides a client–server interface that allows health care providers to review and update a patient's electronic medical record. This includes the ability to place orders, including those for medications, special procedures, X-rays, nursing interventions, diets, and laboratory tests. CPRS provides flexibility in a wide variety of settings so that a consistent, event-driven, Windows-style interface is presented to a broad spectrum of health care workers.
Clinical Functions
- Admission Discharge Transfer (ADT)
- Ambulatory Care Reporting
- Anticoagulation Management Tool (AMT)
- Automated Service Connected Designation (ASCD)
- Beneficiary Travel
- Blind Rehabilitation
- Care Management
- Clinical Case Registries
- Clinical Procedures
- Clinical/Health Data Repository (CHDR)
- Computerized Patient Record System (CPRS)
- CPRS: Adverse Reaction Tracking (ART)
- CPRS: Authorization Subscription Utility (ASU)
- CPRS: Clinical Reminders
- CPRS: Consult/Request Tracking
- CPRS: Health Summary
- CPRS: Problem List
- CPRS: Text Integration Utility (TIU)
- Dentistry
- Electronic Wait List Pharm: National Drug File (NDF)
- Emergency Department Integration Software (EDIS)
- Functional Independence Measurement (FIM)
- Group Notes Primary Care Management Module (PCMM)
- HDR – Historical (HDR-Hx)
- Home Based Primary Care (HBPC)
- Home Telehealth
- Immunology Case Registry (ICR)
- Incomplete Records Tracking (IRT)
- Intake and Output Scheduling
- Laboratory Shift Handoff Tool
- Laboratory: Anatomic Pathology
- Laboratory: Blood Bank
- Laboratory: Blood Bank Workarounds
- Laboratory: Electronic Data Interchange (LEDI)
- Laboratory: Emerging Pathogens Initiative (EPI)
- Laboratory: Howdy Computerized Phlebotomy Login Process
- Laboratory: National Laboratory Tests (NLT) Documents and LOINC Request Form
- Laboratory: Point of Care (POC)
- Laboratory: Universal Interface
- Laboratory: VistA Blood Establishment Computer Software (VBECS)
- Lexicon Utility
- Medicine
- Mental Health (YS)
- Methicillin Resistant Staph Aurerus (MRSA)
- Mobile Electronic Documentation (MED)
- Nationwide Health Information Network Adapter (NHIN)
- Nursing
- Nutrition and Food Service (NFS)
- Oncology
- Patient Appointment Info. Transmission (PAIT)
- Patient Assessment Documentation Package (PADP)
- Patient Care Encounter (PCE)
- Patient Record Flags
- Pharm: Automatic Replenish / Ward Stock (AR/WS)
- Pharm: Bar Code Medication Administration (BCMA)
- Pharm: Benefits Management (PBM)
- Pharm: Consolidated Mail Outpatient Pharmacy
- Pharm: Consolidated Mail Outpatient Pharmacy
- Pharm: Controlled Substances
- Pharm: Data Management (PDM)
- Pharm: Drug Accountability
- Pharm: Inpatient Medications
- Pharm: Outpatient Pharmacy
- Pharm: Prescription Practices (PPP)
- Prosthetics
- Quality Audiology and Speech Analysis and Reporting (QUASAR)
- Radiology / Nuclear Medicine
- RAI/MDS
- Remote Order Entry System (ROES)
- Social Work
- Spinal Cord Dysfunction
- Standards & Terminology Services (STS)
- Surgery
- Traumatic Brain Injury (TBI)
- Virtual Patient Record
- VistA Imaging System
- VistAWeb
- Visual Impairment Service Team (VIST)
- Vitals / Measurements
- Women's Health
Financial-Administrative Functions
- Accounts Receivable (AR)
- Auto Safety Incident Surv Track System (ASISTS)
- Automated Information Collection System (AICS)
- Automated Medical Information Exchange (AMIE)
- Clinical Monitoring System Integrated Billing (IB)
- Compensation Pension Record Interchange (CAPRI)
- Current Procedural Terminology (CPT) Library
- Decision Support System (DSS) Extracts
- Diagnostic Related Group (DRG) Grouper
- Electronic Claims Management Engine (ECME)
- Engineering (AEMS / MERS) Police and Security
- Enrollment Application System Quality Management Integration Module
- Equipment / Turn-In Request
- Event Capture Release of Information (ROI) Manager
- Fee Basis
- Fugitive Felon Program (FFP)
- Generic Code Sheet (GCS)
- Health Eligibility Center (HEC)
- Hospital Inquiry (HINQ)
- ICD-9-CM
- Incident Reporting
- Income Verification Match (IVM)
- Integrated Patient Funds
- Occurrence Screen
- Patient Representative
- Personnel and Accounting Integrated Data (PAID)
- Record Tracking
- Veterans Identification Card (VIC/PICS)
- Voluntary Service System (VSS)
- WebHR
- Wounded Injured and Ill Warriors
Infrastructure Functions
- Capacity Management Tools
- Duplicate Record Merge: Patient Merge Name Standardization
- Electronic Error and Enhancement Reporting (E3R)
- Enterprise Exception Log Service (EELS)
- FatKAAT
- FileMan
- FileMan Delphi Components (FMDC)
- Health Data Informatics
- Health Level 7 (HL7) (VistA Messaging)
- Institution File Redesign (IFR)
- KAAJEE
- Kernel
- Kernel Delphi Components (KDC)
- Kernel Toolkit
- Kernel Unwinder
- List Manager
- M-to-M Broker
- MailMan
- Master Patient Index (MPI)
- Medical Domain Web Services (MDWS) (MWVS*2)
- National Online Information Sharing (NOIS)
- National Patch Module
- Network Health Exchange (NHE)
- Patient Data Exchange (PDX)
- Remote Procedure Call (RPC) Broker
- Resource Usage Monitor
- Single Signon/User Context (SSO/UC)
- SlotMaster (Kernel ZSLOT)
- SQL Interface (SQLI)
- Standard Files and Tables
- Statistical Analysis of Global Growth (SAGG)
- Survey Generator
- System Toolkit (STK)
- VistA Data Extraction Framework (VDEF)
- VistALink
- XML Parser (VistA)
Patient Web Portal Functions
- Clinical Information Support System (CISS)
- Electronic Signature (ESig) Person Services
- HealtheVet Web Services Client (HWSC) Registries
- My HealtheVet Spinal Cord Injury and Disorders Outcomes (SCIDO)
- National Utilization Management Integration (NUMI)
- Occupational Health Record-keeping System (OHRS)
- Patient Advocate Tracking System (PATS)
- VA Enrollment System (VES)
- Veterans Personal Finance System (VPFS)
Achievements
For its development of VistA, the United States Department of Veterans Affairs (VA) / Veterans Health Administration (VHA) was named the recipient of the prestigious Innovations in American Government Award presented by the Ash Institute of the John F. Kennedy School of Government at Harvard University in July, 2006. The VistA electronic medical records system is estimated to improve efficiency by 6% per year, and the monthly cost of the EHR is offset by eliminating the cost of even a few unnecessary tests or admissions.[7][8]
The adoption of VistA has allowed the VA to achieve a pharmacy prescription accuracy rate of 99.997%, and the VA outperforms most public sector hospitals on a variety of criteria, enabled by the implementation of VistA.[9]
VA hospitals using VistA are one of only thirteen hospital systems that have achieved the qualifications for HIMSS stage 7, the highest level of electronic health record integration,[10][11] while a non-VA hospital using VistA is one of only 42 US hospitals that has achieved HIMSS stage 6.[12][13]
Licensing and dissemination
The VistA system is public domain software, available through the Freedom Of Information Act directly from the VA website[14] or through a growing network of distributors, such as the OSEHRA VistA-M.git tree.
VistA modules and projects
Database backend
VistA was developed using the M or MUMPS language/database. The VA currently runs a majority of VistA systems on the proprietary InterSystems Caché version of MUMPS, but an open source MUMPS database engine, called GT.M, for Linux and Unix computers has also been developed. Although initially separate releases, publicly available VistA distributions are now often bundled with the GT.M database in an integrated package. This has considerably eased installation. The free, open source nature of GT.M allows redundant and cost-effective failsafe database implementations, increasing reliability for complex installations of VistA.
Database projections
An open source project called EsiObjects has also allowed the (ANSI- Standard) MUMPS language and database technology to evolve into a modern object-oriented language (and persistent-object store) that can be integrated into mainstream, state-of-the-art technologies. For the Caché MUMPS database, a similar object-oriented extension to MUMPS called Caché ObjectScript has been developed. Both of these have allowed development of the MUMPS database environment (by programmers) using modern object-oriented tools.
M2Web is an open source web gateway to MUMPS for use with VistA.
A free open source module from M/Gateway called MGWSI has been developed to act as a gateway between GT.M, Cache, or M21 MUMPS databases and programming tools such as PHP, ASP.NET, or Java, in order to create a web-based interface.
Patient Web Portal
MyHealtheVet is a web portal that allows veterans to access and update their personal health record, refill prescriptions, and schedule appointments. This also allows veterans to port their health records to institutions outside the VA health system or keep a personal copy of their health records, a Personal Health Record (PHR).
VistA Imaging
The Veterans Administration has also developed VistA Imaging, a coordinated system for communicating with PACS (radiology imaging) systems and for integrating others types of image-based information, such as EKGs, pathology slides, and scanned documents, into the VistA electronic medical records system. This type of integration of information into a medical record is critical to efficient utilization.[15]
It can be used independently or integrated into the VistA electronic health record system (as is done in VA health facilities).
Deployments and uses
Role in development of a national healthcare network
The VistA electronic healthcare record has been widely credited for reforming the VA healthcare system, improving safety and efficiency substantially. The results have spurred a national impetus to adopt electronic medical records similar to VistA nationwide.
VistA Web collectively describes a set of protocols that in 2007 was being developed and used by the VHA to transfer data (from VistA) between hospitals and clinics within the pilot project. This is the first effort to view a single patient record so that VistA becomes truly interoperable among the more than 128 sites running VistA today.
BHIE enables real-time sharing of electronic health information between DoD and VA for shared patients of allergy, outpatient pharmacy, demographic, laboratory, and radiology data. This became a priority during the Second Iraq War, when a concern for the transition of healthcare for soldiers as they transferred from active military status to veteran status became a national focus of attention.[16]
A Clinical Data Repository/Health Data Repository (CHDR) allows interoperability between the DoD's Clinical Data Repository (CDR) & the VA's Health Data Repository (HDR). Bidirectional real time exchange of computable pharmacy, allergy, demographic and laboratory data occurred in phase 1. Phase 2 involved additional drug–drug interaction and allergy checking. Initial deployment of the system was completed in March 2007 at the El Paso, Augusta, Pensacola, Puget Sound, Chicago, San Diego, and Las Vegas facilities.
The combination of VistA and the interoperable projects listed above in the VA/DoD systems will continue to expand to meet the objectives that all citizens will have an electronic record by 2014.
Because of the success of these programs, a national move to standardize healthcare data transmission across the country was started. Text-based information exchange is standardized using a protocol called HL7 (Health Level 7), which is approved by the American National Standards Institute. DICOM is an international image communications protocol standard. VistA is compliant with both.
VistA has been interfaced with commercial off-the-shelf products, as well. Standards and protocols used by VA are consistent with current industry standards and include HL7, DICOM, and other protocols.
Tools for CCR/CCD support have been developed for VistA, allowing VistA to communicate with other EHRs using these standardized information exchange protocols.[17] This includes the Mirth open source cross platform HL7 interface and NHIN Connect, the open source health information exchange adaptor.
In 2009, a project was undertaken to facilitate EHR communication between the VA (using VistA) and Kaiser Permanente (using Epic) using NHIN Connect.[18] (Both VistA and the commercial EHR Epic use a derivative of the MUMPS database, thereby facilitating data exchange.) When completed, two of the largest medical record systems in the US will be able to exchange health data. Public-domain VistA derivatives are also expected to be able to use NHIN Connect.
The VistA EHR has been used by the VA in combination with Telemedicine to provide surgical care to rural areas in Nebraska and Western Iowa over a 400,000-square-mile (1,000,000 km2) area.[19]
Usage in non-governmental hospitals
Under the Freedom of Information Act (FOIA), the VistA system, the CPRS graphical interface, and unlimited ongoing updates (500–600 per year) are provided as public domain software.[20]
This was done by the US government in an effort to make VistA available as a low cost Electronic Health Record (EHR) for non-governmental hospitals and other healthcare entities.
With funding from The Pacific Telehealth & Technology Hui, the Hui 7 produced a version of VistA that ran on GT.M in a Linux operating system, and that was suitable for use in private settings. VistA has since been adapted by companies such as Blue Cliff, DSS, Inc., Medsphere, and Sequence Managers Software to a variety of environments, from individual practices to clinics to hospitals, to regional healthcare co-ordination between far-flung islands. In addition, VistA has been adopted within similar provider environments worldwide. Universities, such as UC Davis and Texas Tech implemented these systems. A non-profit organization, WorldVistA, has also been established to extend and collaboratively improve the VistA electronic health record and health information system for use outside of its original setting.
VistA (and other derivative EMR/EHR systems) can be interfaced with healthcare databases not initially used by the VA system, including billing software, lab databases, and image databases (radiology, for example).
VistA implementations have been deployed (or are currently being deployed) in non-VA healthcare facilities in Texas,[21] Arizona,[22] Florida, Hawaii,[23] New Jersey,[24] Oklahoma,[23] West Virginia,[25][26] California,[27][28] New York,[29] and Washington, D.C.[23][30]
In one state, the cost of a multiple hospital VistA-based EHR network was implemented for one tenth the price of a commercial EHR network in another hospital network in the same state ($9 million versus $90 million for 7–8 hospitals each). (Both VistA and the commercial system used the MUMPS database).[31]
VistA has even been adapted into a Health Information System (VMACS) at the veterinary medical teaching hospital at UC Davis.[32]
International deployments
VistA software modules have been installed around the world, or are being considered for installation, in healthcare institutions such as the World Health Organization,[25] and in countries such as Mexico,[23][25][33] Samoa,[23] Finland, Jordan,[34] Germany,[35] Kenya,[25] Nigeria,[36] Egypt,[23] Malaysia, India,[37] Brazil, Pakistan,[30] and Denmark.[38]
In September 2009, Dell Computer bought Perot Systems, the company installing VistA in Jordan (the Hakeem project).[39]
History
The concept that eventually became VistA was initiated and planned at the beginning of the 1970s by the National Center for Health Services Research and Development of the U.S. Public Health Service (NCHSR&D/PHS). (The NCHSR&D is now known as the Agency for Healthcare Research and Quality (AHRQ).)
As a proof of concept, the U.S. Navy's clinic at the Brunswick Naval Air Station had used an early version of the system software to develop an operational, automated, clinic-management and medical-record system that was "paperless".
The National Center for Health Sciences Research and Development then turned to an agency of the U.S. Department of Commerce, the National Bureau of Standards (NBS, reorganized in 1988 as the National Institute of Standards and Technology), to turn the systems-technology strategy into a systems-architecture design.
Under the farsighted leadership of the VA's Chief Medical Director, Dr. John Chase, the VA's Department of Medicine and Surgery (now known as the Veterans Health Administration (VHA)), then agreed to deploy the system at the largest medical system of that time, the VA hospitals.
Both Dr. Robert Kolodner (National Health Information Technology Coordinator)[40] and George Timson (an architect of VistA who has been involved with it since the early years) date VistA's actual architecture genesis, then, to 1977.[41][42] The program was launched in 1978 with the deployment of the initial modules in about twenty VA Medical Centers. The program was named the Decentralized Hospital Computer Program (DHCP) in 1981.
The physicians in VA Medical Centers, with leadership from the National Association of VA Physicians (NAVAP, renamed NAVAPD in 1989 when Dentists were added) and its Executive Director, Dr. Paul Shafer, made sure that the VA understood the importance of clinician-directed development and refinement of this new clinical-information system.
In December 1981, Congressman Sonny Montgomery of Mississippi arranged for the Decentralized Hospital Computer Program (DHCP) to be written into law as the medical-information systems development program of the VA. VA Administrator Robert P. Nimmo signed an Executive Order in February 1982 describing how the DHCP was to be organized and managed within the VA's Department of Medicine and Surgery.
In consultation with F. Whitten Peters and Vincent Fuller of the Williams and Connolly law firm, it was established at the beginning of the 1980s that the software existing in the VA (derived from the PHS projects) was legally in the public domain and must be made available without proprietary or other restrictions to other government and private-sector organizations for their use.
In conjunction with the VA's DHCP development, the (IHS) Indian Health Service deployed a system built on and augmenting DHCP throughout its Federal and Tribal facilities as the Resource and Patient Management System (RPMS). This implementation emphasized the integration of outpatient clinics into the system, and many of its elements were soon re-incorporated into the VA system (through a system of technology sharing). Subsequent VistA systems therefore included elements from both RPMS and DHCP. Health IT sharing between VA and IHS continues to the present day.
The U.S. Department of Defense (DoD) then contracted with Science Applications International Corporation (SAIC) for a heavily modified and extended form of the DHCP system for use in DoD healthcare facilities, naming it the Composite Health Care System (CHCS).
Meanwhile, in the early 1980s, major hospitals in Finland[43] were the first institutions outside of the United States to adopt and adapt the VistA system to their language and institutional processes, creating a suite of applications called MUSTI and Multilab. (Since then, institutions in Germany, Egypt,[23] Nigeria,[36] and other nations abroad have adopted and adapted this system for their use, as well.)
The name "VistA" (Veterans Health Information System and Technology Architecture) was adopted by the VA in 1994, when the Under Secretary for Health of the U.S. Department of Veterans Affairs (VA), Dr. Ken Kizer, renamed what had previously been known as the Decentralized Hospital Computer Program (DHCP).
The four major adopters of VistA – VA (VistA), DoD (CHCS), IHS (RPMS), and the Finnish Musti consortium – each took VistA in a different direction, creating related but distinct "dialects" of VistA. VA VistA and RPMS exchanged ideas and software repeatedly over the years, and RPMS periodically folded back into its code base new versions of the VA VistA packages. These two dialects are therefore the most closely related. The Musti software drifted further away from these two but retained compatibility with the infrastructure of RPMS and VA VistA (while adding additional GUI and web capabilities to improve function). Meanwhile, the CHCS code base diverged from that of the VA's VistA in the mid-eighties and has never been reintegrated. The VA and the DoD had been instructed for years to improve the sharing of medical information between the two systems, but for political reasons made little progress toward bringing the two dialects back together. More recently, CHCS's development was brought to a complete stop by continued political opposition within the DoD, and it has now been supplanted by a related, but different, system called AHLTA. While AHLTA is the new system for DoD, the core systems beneath AHLTA (for Computerized Physician Order Entry, appointing, referral management, and creation of new patient registrations) remain those of the underlying CHCS system. (While some ongoing development has occurred for CHCS, the majority of funds are consumed by the AHLTA project.) Thus, the VistA code base was split four ways.
Many VistA professionals then informally banded together as the "Hardhats" (a name the original VistA programmers used for themselves) to promote that the FOIA (Freedom of Information Act) release of VA VistA (that allows it to be in the public domain) be standardized for universal usage.
WorldVistA was formed from this group and was incorporated in March 2003 as a non-profit corporation. This allowed the WorldVistA board of directors to pursue certain activities (obtaining grants, creating contracts, and making formal alliances) that they otherwise could not pursue as an informal organization. It is, however, an organization independent of the VA system and its version of VistA therefore differs from that of the VA's. Nevertheless, it maintains as an objective that its public version be compatible (interoperable) with the VA's official version. It has developed packages of WorldVistA for multiple operating systems, including Linux (Debian/Ubuntu and Red Hat) -based and Microsoft Windows-based operating systems. Co-operation with the maintainers and vendors of OpenVistA, another widely deployed open source public version of VistA, helps maintain interoperability and a standardized framework.
In 2011 the Open Source Electronic Health Record Agent (OSEHRA) project was started (in cooperation with the Department of Veterans Affairs) to provide a common code repository for VistA (and other EHR and health IT) software.[44]
Therefore, it is through the joint achievement of thousands of clinicians and professional systems experts from the United States and other nations, many of them volunteers, that the VistA system has developed.
Supporters of VistA
There have been many champions of VistA as the electronic healthcare record system for a universal healthcare plan. VistA can act as a standalone system, allowing self-contained management and retention of healthcare data within an institution. Combined with BHIE (or other data exchange protocol) it can be part of a peer-to-peer model of universal healthcare. It is also scalable to be used as a centralized system (allowing regional or even national centralization of healthcare records). It is, therefore, the electronic records system most adaptable to a variety of healthcare models.
In addition to the unwavering support of congressional representatives such as Congressman Sonny Montgomery of Mississippi, numerous IT specialists, physicians, and other healthcare professionals have donated significant amounts of time in adapting the VistA system for use in non-governmental healthcare settings.
The ranking member of the House Veterans Affairs Committee's Oversight and Investigation Subcommittee, Rep. Ginny Brown-Waite of Florida, recommended that the Department of Defense (DOD) adopt VA's VistA system following accusations of inefficiencies in the DOD healthcare system. The DOD hospitals use Armed Forces Health Longitudinal Technology Application (AHLTA) which has not been as successful as VistA and has not been adapted to non-military environments (as has been done with VistA).[16]
In November 2005, the U.S. Senate passed the Wired for Health Care Quality Act, introduced by Sen. Enzi of Wyoming with 38 co-sponsors, that would require the government to use the VA's technology standards as a basis for national standards allowing all health care providers to communicate with each other as part of a nationwide health information exchange. The legislation would also authorize $280 million in grants, which would help persuade reluctant providers to invest in the new technology.[45] There has been no action on the bill since December 2005. Two similar House bills were introduced in late 2005 and early 2006; no action has been taken on either of them, either.[46]
In late 2008, House Ways and Means Health Subcommittee Chair Congressman Pete Stark (D-CA) introduced the Health-e Information Technology Act of 2008 (H.R. 6898) that calls for the creation of a low-cost public IT system for those providers who do not want to invest in a proprietary one.[47]
In April 2009, Sen. John D. Rockefeller of West Virginia introduced the Health Information Technology Public Utility Act of 2009 calling for the government to create an open source electronic health records solution and offer it at little or no cost to safety-net hospitals and small rural providers.[48][49]
VistA Derivatives
- Astronaut VistA – an installer suite for different versions of VistA, with multiple enhancements and bug fixes.
- WorldVistA or WorldVistA EHR
- OpenVistA (Medsphere)
- Osehra-Vista (OSEHRA)
- vxVistA (Document Storage Systems, Inc.)
An effort has been made by the Astronaut team, WorldVistA team, members of the VistA Software Alliance, and the OSEHRA to standardize structure between the platform derivatives to allow for future interoperability, as part of the vision for a national healthcare network record system.
See also
- Electronic health record
- Health informatics
- MUMPS
- Veterans Health Administration
- United States Department of Veterans Affairs
- FileMan
- VA Kernel
- GNUmed
- GNU Health
References
- ↑ "VA Health Care".
- ↑ "Nation's Largest Healthcare System Pledges Involvement in Healthy Hospital Initiative". US Environmental Protection Agency (Sep 2003).
- ↑ "Veterans Health Administration – Locations".
- ↑ "NEJM: VA VistA nearly doubles proportion of computerized hospitals.". LinuxMedNews (Mar 2009).
- ↑ "Use of Electronic Health Records in U.S. Hospitals". New England Journal of Medicine (March 25, 2009).
- ↑ Brown, Stephen H. (2003). "VistA, U.S. Department of Veterans Affairs national scale HIS" (PDF). International Journal of Medical Informatics. 69 (2–3): 135. doi:10.1016/S1386-5056(02)00131-4.
- ↑ "Effect of the implementation of an enterprise-wide Electronic Health Record on productivity in the Veterans Health Administration". Health Econ Policy Law. 1 (Pt 2): 163–9. April 2006. doi:10.1017/S1744133105001210. PMID 18634688.
- ↑ "VistA:Winner of the 2006 Innovations in American Government Award" (PDF). The Ash Institute for Democratic Governance and Innovation at Harvard University's John F. Kennedy School of Government.
- ↑ "The Best Medical Care in the U.S. How Veterans Affairs transformed itself – and what it means for the rest of us". BusinessWeek, Red Oak, IA (USA). July 16, 2006.
- ↑ VA Testimony of Roger Baker before Congress on July 14, 2009 – Congressional and Legislative Affairsva.gov. "Open Source Healthcare IT at a National Level". United States Department of Veterans Affairs (2009).
- ↑ HIMSS Analytics Stage 7 Hospitalshimssanalytics.org. "HIMSS Analytics Stage 7 Hospitals". HIMSS Analytics.
- ↑ "Honored for EMR Sophistication, HIMSS Analytics Announces Stage 6 Hospitals". HIMSS Analytics (Feb 2009).
- ↑ "Midland Memorial Hospital Uses OpenVista Clinical Framework to Improve Patient Care and Reduce Costs". Medsphere (Mar 2008).
- ↑ "VistA – VHA Office of Health Information".
- ↑ "PACS Lessons Learned at the Baltimore VA". Imaging Economics, Skokie, IL (USA). December 2002. (subscription required (help)).
- 1 2 Mosquera, Mary (May 9, 2007). "Full VA/DOD e-health sharing several years off". Government Health IT, Falls Church, VA (USA). Archived from the original on September 26, 2007.
- ↑ "Opensource CCR and CCD support for VistA based systems Project Update (Powerpoint slideshow)". WorldVistA.org (Feb 2010).
- ↑ "VA, Kaiser plan to link electronic medical records". Healthcare IT News (Nov 2009).
- ↑ "VA Telemedicine Program Expands Access to Bariatric Surgery". General Surgery News Vol. 36, Number 12 p.40 (Dec 2009).
- ↑ "Introduction to VistA software and the FTP site". US Department of Veterans Affairs.
- ↑ "Old code proves key to modern IT at Midland Memorial Hospital". Computerworld (Nov 2008).
- ↑ "Statement of Matthew King, M.D., Chief Medical Officer, Clinica Adelante, Inc, Surprise, Arizona". US Congress House Committee on Ways and Means (July 2008).
- 1 2 3 4 5 6 7 "VistA has been implemented in a variety of locations worldwide.". Vista Software Alliance.
- ↑ "Hoboken University Medical Center Selects Medsphere's OpenVista Solution". Medsphere (Oct 2009).
- 1 2 3 4 "VistA Tour Announcement (Oct 2008)".
- ↑ "VA's health record system cited as model for a national network". Nextgov (Mar 2009).
- ↑ "Oroville Hospital to Deploy Medsphere OpenVista Electronic Health Record". Businesswire, (Jan 2007).
- ↑ "Kern Medical Center Selects OpenVista". Medsphere, (Dec 2009).
- ↑ "Brooklyn's Lutheran Medical Center Selects Medsphere OpenVista for Electronic Health Record Deployment". BNET, (Jan 2007). January 8, 2007.
- 1 2 "Implementation of the Veterans Health Administration VistA Clinical Information System around the World". ElectronicHealthcare, 7(2) 2008: 83–89. Archived from the original on February 19, 2012.
- ↑ "Ten Fold (10X): Is There Really an Order of Magnitude Difference?". CrossOver Health (Jan 2009).
- ↑ "Demonstration of M2Web". UC Davis VMTH (Veterinary Medical Hospital) (Dec 2008).
- ↑ "VistA use continues to grow in Mexico". ModernHealthcare.com (Jan 2007).
- ↑ "Jordan picks Perot to help implement VistA". EHealth (Jan 2009).
- ↑ Implemented in 1992 at the Berlin Heart Institute, VistA is still in use there."VistA News – July 18, 2006 – Harvard Honors the VA, VistA". HardHats.
- 1 2 "MINPHIS: Nigeria's experience using VistA, MUSTI, and other technologies in building their own national health information system". Virtual Medical Worlds (August 2005).
- ↑ "Global Tender for Computerization and Hospital Information System Jai Prakash Narayan Apex Trauma Center" (PDF). Jai Prakash Narayan Apex Trauma Center.
- ↑ "Læge: Open source vil kunne løse Danmarks EPJ-problemer". Version 2 (August 2008).
- ↑ "Dell To Acquire Perot Systems For $3.9 Billion, Creating Comprehensive, Customer-Focused It-Solutions Company". Perot Systems (Sep 2009).
- ↑ http://www.hhs.gov/healthit/onc/mission/
- ↑ Robert Kolodner, MD (1997). Computerizing Large Integrated Health Networks: The VA Success.
- ↑ "The History of the Hardhats". Hardhats.org.
- ↑ Douglas E. Goldstein; et al. (2007). Medical informatics 20/20 (Case Studies of VistA Implementation United States and International) p. 276. Jones & Bartlett Learning. ISBN 978-0-7637-3925-6.
- ↑ "VistA Community Makes Major Strides Towards Code Unification". OpenHealth News (Jan 2012).
- ↑ "Senator Endorses VistA for EHR Standard". Linux MedNews. January 20, 2006.
- ↑ "Library of Congress: Thomas: Bills, resolutions: S.1418". Library of Congress. Retrieved June 10, 2007.
- ↑ "Representative Stark Introduces Health-e Information Technology Act of 2008". Medicare Update. September 16, 2008.
- ↑ Landro, Laura (April 30, 2009). "An Affordable Fix for Modernizing Medical Records". Wall Street Journal.
- ↑ "Rockefeller Introduced Legislation Calling For Universal Adoption of Electronic Health Records". United States Senator Jay Rockefeller. April 23, 2009.
External links
- Vistapedia: the WorldVistA Wiki
- Hardhats – a VistA user community
- Hardhats Google Group – a forum to discuss installation of WorldVistA
- VISTA Monograph (Veterans Administration)
- VistA Monograph wiki (OLPC project)
- VistA Software Alliance (VistA Software Vendor Trade Organization)
- OSEHRA – Open Source Electronic Health Record Agent, a code repository for VistA
- VistA / CPRS Demo site (Department of Veterans Affairs)
- VA VistA software FTP site (Department of Veterans Affairs)
- The Pacific Telehealth & Technology Hui
- VistA Imaging overview (Department of Veterans Affairs)
- BHIE – Bidirectional Health Information Exchange protocols of the Department of Veterans Affairs
- Why is VistA good?
- "Innovations Award" (PDF). Retrieved July 25, 2006. – Ash Institute News Release
- VistA Glossary LiuTiu Medical Administrative Lexicon (Brokenly translated into English from Russian)
- Ubuntu Doctors Guild Information about implementing VistA and other open source medical applications in Ubuntu Linux
Videos about VistA:
- VistA at the VA
- History of Vista Architecture Interview with Tom Munnecke
- Interview with Rob Kolodner regarding VistA's potential for the National Health Information Network
- Impact of VistA Interview with Dr. Ross Fletcher
- Interview with Philip Longman
- Events leading up to the development of VistA Interview with Henry Heffernan
- History of Vista Interview with Ruth Dayhoff
- Early development of the Decentralized Hospital Computer Program Interview with Marty Johnson
- Early days of the VA "Underground Railroad" Interview with Tom Munnecke