Beta thalassemia
| Beta thalassemia | |
|---|---|
|
Beta thalassemia genetics | |
| Classification and external resources | |
| Specialty | Hematology |
| ICD-10 | D56.1 |
| ICD-9-CM | 282.44 |
| OMIM | 141900 |
| DiseasesDB | 3087 1373 |
| eMedicine | article/199534 |
| MeSH | D017086 |
Beta thalassemias (β thalassemias) are a group of inherited blood disorders. They are forms of thalassemia caused by reduced or absent synthesis of the beta chains of hemoglobin that result in variable outcomes ranging from severe anemia to clinically asymptomatic individuals. Global annual incidence is estimated at 1 in 100,000.[1] Beta thalassemias are caused by mutations in the HBB gene on chromosome 11, inherited in an autosomal recessive fashion. The severity of the disease depends on the nature of the mutation.[2]
HBB blockage over time leads to decreased beta-chain synthesis. The body's inability to construct new beta-chains leads to the underproduction of HbA.[3] Reductions in HbA available overall to fill the red blood cells in turn leads to microcytic anemia. Microcytic anemia ultimately develops in respect to inadequate HBB for sufficient red blood cell functioning.[4] Due to this factor, the patient may require blood transfusions to make up for the blockage in the beta-chains. Repeated blood transfusions can lead to build-up of iron overload, ultimately resulting in iron toxicity. This iron toxicity can cause various problems, including myocardial siderosis and heart failure leading to the patient’s death.[5]
Signs and symptoms
Three main forms have been described: thalassemia major, thalassemia intermedia and thalassemia minor. All people with thalassemia are susceptible to health complications that involve the spleen (which is often enlarged and frequently removed) and gallstones.[6] These complications are mostly found in thalassemia major and intermedia patients. Individuals with beta thalassemia major usually present within the first two years of life with severe anemia, poor growth and skeletal abnormalities during infancy. Untreated thalassemia major eventually leads to death, usually by heart failure; therefore, birth screening is very important.[7]
Excess iron causes serious complications within the liver, heart and endocrine glands. Severe symptoms include liver cirrhosis, liver fibrosis and in extreme cases, liver cancer.[8] Heart failure, growth impairment, diabetes and osteoporosis are life-threatening contributors brought upon by TM.[9] The main cardiac abnormalities seen to have resulted from thalassemia and iron overload include left ventricular systolic and diastolic dysfunction, pulmonary hypertension, valveulopathies, arrhythmias and pericarditis. Increased gastrointestinal iron absorption is seen in all grades of beta thalassemia and increased red blood cell destruction by the spleen due to ineffective erythropoiesis further releases additional iron into the bloodstream.[10]
Cause
Mutations
Two major groups of mutations can be distinguished:
- Nondeletion forms: These defects, in general, involve a single base substitution or small deletion or inserts near or upstream of the β globin gene. Most often, mutations occur in the promoter regions preceding the beta-globin genes. Less often, abnormal splice variants are believed to contribute to the disease.[11]
- Deletion forms: Deletions of different sizes involving the β globin gene produce different syndromes such as (βo) or hereditary persistence of fetal hemoglobin syndromes.[12]
| Name | Older synonyms | Description | Alleles |
|---|---|---|---|
| Thalassemia minor | Heterozygous form: Only one of β globin alleles bears a mutation. Individuals will suffer from microcytic anemia. Detection usually involves lower than normal MCV value (<80 fL).[13] | β+/β βo/β | |
| Thalassemia intermedia | Affected individuals can often manage a normal life but may need occasional transfusions, e.g., at times of illness or pregnancy, depending on the severity of their anemia.[14] | β+/β+ βo/β+ | |
| Thalassemia major | Mediterranean anemia; Cooley anemia | Homozygous form: Occurs when both alleles have thalassemia mutations. This is a severe microcytic, hypochromic anemia. Untreated, it causes anemia, splenomegaly and severe bone deformities. It progresses to death before age 20. Treatment consists of periodic blood transfusion; splenectomy for splenomegaly and chelation of transfusion-caused iron overload.[15] | βo/βo |
mRNA assembly
Beta thalassemia is a hereditary disease affecting hemoglobin. As with about half of all hereditary diseases,[16] an inherited mutation damages the assembly of the messenger-type RNA (mRNA) that is transcribed from a chromosome. DNA contains both the instructions (genes) for stringing amino acids together into proteins, as well as stretches of DNA that play important roles in regulating produced protein levels.[17]
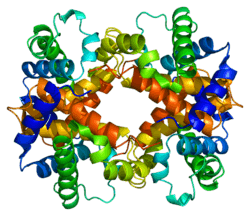
In thalassemia, an additional, contiguous length or a discontinuous fragment of non-coding instructions are included in the mRNA. This happens because the mutation obliterates the boundary between the intronic and exonic portions.[18] Because all the coding sections may still be present, normal hemoglobin may be produced and the added material, if it produces pathology, instead disrupts regulatory functions enough to produce anemia.Hemoblogin's normal alpha and beta subunits each have an iron-containing central portion (heme) that allows the protein chain of a subunit to fold around it. Normal adult hemoglobin contains 2 alpha and 2 beta subunits.[19] Thalassemias typically affect only the mRNAs for production of the beta chains (hence the name). Since the mutation may be a change in only a single base (a "Single Nucleotide Polymorphism"), on-going efforts seek gene therapies to make that single correction.[20][21]
Diagnosis
Abdominal pain due to hypersplenism and splenic infarction and right-upper quadrant pain caused by gallstones are major clinical manifestations. However, diagnosing thalassemiæ from symptoms alone is inadequate. Physicians note these signs as associative due to this disease's complexity.[22] The following associative signs can attest to the severity of the phenotype: pallor, poor growth, inadequate food intake, splenomegaly, jaundice, maxillary hyperplasia, dental malocclusion, cholelithiasis, systolic ejection murmur in the presence of severe anemia and pathologic fractures. Based on symptoms, tests are ordered for a differential diagnosis. These tests include complete blood count; hemoglobin electrophoresis; serum transferrin, ferritin, total iron-binding capacity; urine urobilin and urobilogen; peripheral blood smear, which may show codocytes, or target cells;[23] hematocrit; and serum bilirubin.[24][25]
DNA analysis
All beta thalassemias may exhibit abnormal red blood cells, a family history is followed by DNA analysis.[26] This test is used to investigate deletions and mutations in the alpha- and beta-globin-producing genes. Family studies can be done to evaluate carrier status and the types of mutations present in other family members. DNA testing is not routine, but can help diagnose thalassemia and determine carrier status. In most cases the treating physician uses a clinical prediagnosis assessing anemia symptoms: fatigue, breathlessness and poor exercise tolerance.[27] Further genetic analysis may include HPLC should routine electrophoresis prove difficult.[24]
Treatment
Beta thalassemia major

Affected children require regular lifelong blood transfusion and can have complications, which may involve the spleen. Bone marrow transplants can be curative for some children.[28] Patients receive frequent blood transfusions that lead to or potentiate iron overload.[29] Iron chelation treatment is necessary to prevent damage to internal organs. Advances in iron chelation treatments allow patients with thalassemia major to live long lives with access to proper treatment. Popular chelators include deferoxamine and deferiprone.[30][31]
The most common patient deferoxamine complaint is that they are painful and inconvenient. The oral chelator deferasirox was approved for use in 2005 in some countries,[32][33] it offers some hope with compliance at a higher cost. Bone marrow transplantation is the only cure and is indicated for patients with severe thalassemia major. Transplantation can eliminate a patient's dependence on transfusions. Absent a matching donor, a savior sibling can be conceived by preimplantation genetic diagnosis (PGD) to be free of the disease as well as to match the recipient's human leukocyte antigen (HLA) type.[34]
Scientists at Weill Cornell Medical College have developed a gene therapy strategy that could feasibly treat both beta-thalassemia and sickle cell disease. The technology is based on delivery of a lentiviral vector carrying both the human β-globin gene and an ankyrin insulator to improve gene transcription and translation, and boost levels of β-globin production.[35]
Beta thalassemia intermedia
Patients may require episodic blood transfusions. Transfusion-dependent patients develop iron overload and require chelation therapy[36] to remove the excess iron. Transmission is autosomal recessive; however, dominant mutations and compound heterozygotes have been reported. Genetic counseling is recommended and prenatal diagnosis may be offered.[37] Alleles without a mutation that reduces function are characterized as (β). Mutations are characterized as (βo) if they prevent any formation of β chains,[38] mutations are characterized as (β+) if they allow some β chain formation to occur.
Beta thalassemia minor
Patients are often monitored without treatment. While many of those with minor status do not require transfusion therapy, they still risk iron overload, particularly in the liver. A serum ferritin test checks iron levels and can point to further treatment.[39] Although not life-threatening on its own, it can affect quality of life due to the anemia. Minor often coexists with other conditions such as asthma and can cause iron overload of the liver and in those with non-alcoholic fatty liver disease, lead to more severe outcomes.[40]
Epidemiology
The beta form of thalassemia is particularly prevalent among the Mediterranean peoples and this geographical association is responsible for its naming: thalassa (θάλασσα) is the Greek word for sea and haema (αἷμα) is the Greek word for blood. In Europe, the highest concentrations of the disease are found in Greece and the Turkish coastal regions. The major Mediterranean islands (except the Balearics) such as Sicily, Sardinia, Corsica, Cyprus, Malta and Crete are heavily affected in particular.[41][42] Other Mediterranean peoples, as well as those in the vicinity of the Mediterranean, also have high incidence rates, including people from West Asia and North Africa. The data indicate that 15% of the Greek and Turkish Cypriots are carriers of beta-thalassaemia genes, while 10% of the population carry alpha-thalassaemia genes.[43]
Evolutionary adaptation
The thalassemia trait may confer a degree of protection against malaria,[44] which is or was prevalent in the regions where the trait is common, thus conferring a selective survival advantage on carriers (known as heterozygous advantage), thus perpetuating the mutation. In that respect, the various thalassemias resemble another genetic disorder affecting hemoglobin, sickle-cell disease.[45]
See also
References
- ↑ Galanello, Renzo; Origa, Raffaella (21 May 2010). "Beta-thalassemia". Orphanet J Rare Dis. Orphanet Journal of Rare Diseases. 5: 11. doi:10.1186/1750-1172-5-11. PMC 2893117
 . PMID 20492708.
. PMID 20492708. - ↑ Goldman, Lee; Schafer, Andrew I. (2015-04-21). Goldman-Cecil Medicine: Expert Consult - Online. Elsevier Health Sciences. ISBN 9780323322850.
- ↑ Carton, James (2012-02-16). Oxford Handbook of Clinical Pathology. OUP Oxford. ISBN 9780191629938.
- ↑ Perkin, Ronald M.; Newton, Dale A.; Swift, James D. (2008). Pediatric Hospital Medicine: Textbook of Inpatient Management. Lippincott Williams & Wilkins. ISBN 9780781770323.
- ↑ Galanello, Renzo; Origa, Raffaella (2010-05-21). "Beta-thalassemia". Orphanet Journal of Rare Diseases. 5 (1): 11. doi:10.1186/1750-1172-5-11. ISSN 1750-1172. PMC 2893117
 . PMID 20492708.
. PMID 20492708. - ↑ "Beta thalassemia". Genetics Home Reference. Retrieved 2015-05-26.
- ↑ Introduction to Pathology for the Physical Therapist Assistant. Jones & Bartlett Publishers. 2011. ISBN 9780763799083.
- ↑ Anderson, Gregory J.; McLaren, Gordon D. (2012-01-16). Iron Physiology and Pathophysiology in Humans. Springer Science & Business Media. ISBN 9781603274845.
- ↑ Barton, James C.; Edwards, Corwin Q.; Phatak, Pradyumna D.; Britton, Robert S.; Bacon, Bruce R. (2010-07-22). Handbook of Iron Overload Disorders. Cambridge University Press. ISBN 9781139489393.
- ↑ McCance, Kathryn L.; Huether, Sue E. (2013-12-13). Pathophysiology: The Biologic Basis for Disease in Adults and Children. Elsevier Health Sciences. ISBN 9780323088541.
- ↑ Leonard, Debra G. B. (2007-11-25). Molecular Pathology in Clinical Practice. Springer Science & Business Media. ISBN 9780387332277.
- ↑ Bowen, Juan M.; Mazzaferri, Ernest L. (2012-12-06). Contemporary Internal Medicine: Clinical Case Studies. Springer Science & Business Media. ISBN 9781461567134.
- ↑ Disorders, National Organization for Rare (2003). NORD Guide to Rare Disorders. Lippincott Williams & Wilkins. ISBN 9780781730631.
- ↑ Barton, James C.; Edwards, Corwin Q. (2000-01-13). Hemochromatosis: Genetics, Pathophysiology, Diagnosis and Treatment. Cambridge University Press. ISBN 9780521593809.
- ↑ Wilkins, Lippincott Williams & (2009). Professional Guide to Diseases. Lippincott Williams & Wilkins. ISBN 9780781778992.
- ↑ Ward, Amanda J; Cooper, Thomas A (2009). "The pathobiology of splicing". The Journal of Pathology. 220 (2): 152–63. doi:10.1002/path.2649. PMC 2855871
 . PMID 19918805.
. PMID 19918805. - ↑ "the definition of dna". Dictionary.com. Retrieved 2015-05-26.
- ↑ Okpala, Iheanyi (2008-04-15). Practical Management of Haemoglobinopathies. John Wiley & Sons. ISBN 9781405140201.
- ↑ Vasudevan, D. M.; Sreekumari, S.; Vaidyanathan, Kannan (2011-11-01). Textbook of Biochemistry for Dental Students. JP Medical Ltd. ISBN 9789350254882.
- ↑ Taeusch, H. William; Ballard, Roberta A.; Gleason, Christine A.; Avery, Mary Ellen (2005). Avery's Diseases of the Newborn. Elsevier Health Sciences. ISBN 0721693474.
- ↑ Beta Thalassemia: New Insights for the Healthcare Professional: 2013 Edition: ScholarlyBrief. ScholarlyEditions. 2013-07-22. ISBN 9781481663472.
- ↑ "How Are Thalassemias Diagnosed? - NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 2015-05-26.
- ↑ Target Cells, Imperial College of London Department of Medicine
- 1 2 Orkin, Stuart H.; Nathan, David G.; Ginsburg, David; Look, A. Thomas; Fisher, David E.; Lux, Samuel (2009). Nathan and Oski's Hematology of Infancy and Childhood (7th ed.). Philadelphia: Saunders. ISBN 978-1-4160-3430-8.
- ↑ "What Are the Signs and Symptoms of Thalassemias? - NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 2015-05-26.
- ↑ McKinney, Emily Slone; James, Susan R.; Murray, Sharon Smith; Nelson, Kristine; Ashwill, Jean (2014-04-17). Maternal-Child Nursing. Elsevier Health Sciences. ISBN 9780323293778.
- ↑ Schrijver, Iris (2011-09-09). Diagnostic Molecular Pathology in Practice: A Case-Based Approach. Springer Science & Business Media. ISBN 9783642196775.
- ↑ Muncie, Herbert L.; Campbell, James S. (2009). "Alpha and Beta Thalassemia". American Family Physician. 80 (4): 339–44. PMID 19678601.
- ↑ Greer, John P.; Arber, Daniel A.; Glader, Bertil; List, Alan F.; Means, Robert T.; Paraskevas, Frixos; Rodgers, George M. (2013-08-29). Wintrobe's Clinical Hematology. Lippincott Williams & Wilkins. ISBN 9781469846224.
- ↑ Greer, John P.; Arber, Daniel A.; Glader, Bertil; List, Alan F.; Means, Robert T.; Paraskevas, Frixos; Rodgers, George M. (2013-08-29). Wintrobe's Clinical Hematology. Lippincott Williams & Wilkins. ISBN 9781469846224.
- ↑ Hydroxamic Acids: Advances in Research and Application: 2011 Edition: ScholarlyPaper. ScholarlyEditions. 2012-01-09. ISBN 9781464952081.
- ↑ "NCBI - WWW Error Blocked Diagnostic". pubchem.ncbi.nlm.nih.gov. Retrieved 2015-05-26.
- ↑ "Deferoxamine". livertox.nih.gov. Retrieved 2015-05-26.
- ↑ Sabloff, Mitchell; Chandy, Mammen; Wang, Zhiwei; Logan, Brent R.; Ghavamzadeh, Ardeshir; Li, Chi-Kong; Irfan, Syed Mohammad; Bredeson, Christopher N.; Cowan, Morton J. (2011). "HLA-matched sibling bone marrow transplantation for β-thalassemia major". Blood. 117 (5): 1745–1750. doi:10.1182/blood-2010-09-306829. ISSN 0006-4971. PMC 3056598
 . PMID 21119108.
. PMID 21119108. - ↑ "Gene Therapy Shows Promise for Treating Beta-Thalassemia and Sickle Cell Disease". Retrieved 2015-10-15.
- ↑ Schwartz, M. William (2012). The 5 Minute Pediatric Consult. Lippincott Williams & Wilkins. ISBN 9781451116564.
- ↑ Porwit, Anna; McCullough, Jeffrey; Erber, Wendy N. (2011-05-27). Blood and Bone Marrow Pathology. Elsevier Health Sciences. ISBN 0702045357.
- ↑ Hemoglobinopathies. Jaypee Brothers Publishers. 2006. ISBN 9788180616693.
- ↑ Torre, Dario M.; Lamb, Geoffrey C.; Ruiswyk, Jerome Van; Schapira, Ralph M. (2009). Kochar's Clinical Medicine for Students. Lippincott Williams & Wilkins. ISBN 9780781766999.
- ↑ Brissot, Pierre; Cappellini, Maria Domenica (2014). "LIVER DISEASE".
- ↑ "WHO | Global epidemiology of haemoglobin disorders and derived service indicators". www.who.int. Retrieved 2015-05-26.
- ↑ Berg, Sheri; Bittner, Edward A. (2013-10-16). The MGH Review of Critical Care Medicine. Lippincott Williams & Wilkins. ISBN 9781451173680.
- ↑ Haematology Made Easy. AuthorHouse. 2013-02-06. ISBN 9781477246511.
- ↑ Abouelmagd, Ahmed; Ageely, Hussein M. (2013). Basic Genetics: A Primer Covering Molecular Composition of Genetic Material, Gene Expression and Genetic Engineering, and Mutations and Human Genetic. Universal-Publishers. ISBN 9781612331928.
- ↑ Weatherall, David J. Lichtman, MA,; Kipps, TJ,; Seligsohn, U,; Kaushansky, K,; Prchal, JT, eds. The Thalassemias: Disorders of Globin Synthesis. Williams Hematology (8 ed.).
Further reading
- Cao, Antonio; Galanello, Renzo (2010). "Beta-Thalassemia". In Pagon, Roberta A; Bird, Thomas D; Dolan, Cynthia R; Stephens, Karen; Adam, Margaret P. GeneReviews. PMID 20301599.
- Bahal, Raman; McNeer, Nicole Ali; Quijano, Elias; Liu, Yanfeng; Sulkowski, Parker; Turchick, Audrey; Lu, Yi-Chien; Bhunia, Dinesh C.; Manna, Arunava; Greiner, Dale L.; Brehm, Michael A.; Cheng, Christopher J.; López-Giráldez, Francesc; Ricciardi, Adele; Beloor, Jagadish; Krause, Diane S.; Kumar, Priti; Gallagher, Patrick G.; Braddock, Demetrios T.; Saltzman, W. Mark; Ly, Danith H.; Glazer, Peter M. (26 October 2016). "In vivo correction of anaemia in β-thalassemic mice by γPNA-mediated gene editing with nanoparticle delivery". Nature Communications. 7. doi:10.1038/ncomms13304. ISSN 2041-1723. Retrieved 26 October 2016.
