Thyroid hormone resistance
| Thyroid hormone resistance | |
|---|---|
| Classification and external resources | |
| Specialty | Endocrinology |
| ICD-10 | E07 |
| ICD-9-CM | 246.8 |
| OMIM | 274300 188570 |
| DiseasesDB | 31913 |
| MeSH | D018382 |
Thyroid hormone resistance (sometimes Refetoff syndrome) describes a rare syndrome in which the thyroid hormone levels are elevated but the thyroid stimulating hormone (TSH) level is not suppressed, or not completely suppressed as would be expected. The first report of the condition appeared in 1967.[1] Essentially this is decreased end organ responsiveness to thyroid hormones.[2] A new term "impaired sensitivity to thyroid hormone" has been suggested in March 2014 by Refetoff et al.[3]
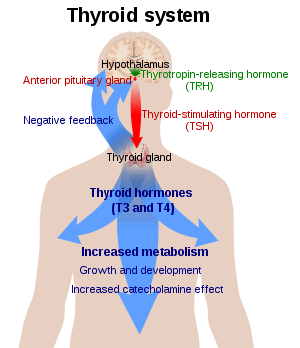
Regulation of thyroid hormone secretion
Hypothalamus secretes a hormone called thyrotropin releasing hormone (TRH) which in turn release thyroid stimulating hormone (TSH). TSH signals thyroid to secrete thyroid hormones thyroxine (T4) and triiodothyronine (T3). T4 gets converted to active T3 in peripheral tissues with the help of deiodinase enzymes. T3 negatively feedback on the pituitary and decreases TSH secretion.
Causes
Normal thyroid hormone function requires normal thyroid hormone transport across cell membrane, appropriate deiodination, thyroid hormone nuclear receptor, thyroid hormone response elements, co-activators, co-repressors, and normal histone acetylation. Any abnormalities in this chain can result in thyroid hormone resistance.
The most common cause of the syndrome are mutations of the β (beta) form (THRB gene) of the thyroid hormone receptor, of which over 100 different mutations have been documented.[4]
Mutations in MCT8 and SECISBP2 have also been associated with this condition.[5]
Incidence
Thyroid hormone resistance syndrome is rare, incidence is variously quoted as 1 in 50,000 or 1 in 40,000 live births.[6] More than 1000 individuals have been identified with thyroid hormone resistance, of which 85% had thyroid hormone beta receptor mutation.[5]
Presentation
The syndrome can present with variable symptoms, even between members of the same family harboring the same mutation.[1] Typically most or all tissues are resistant to thyroid hormone, so despite raised measures of serum thyroid hormone the individual may appear euthyroid (have no symptoms of over- or underactivity of the thyroid gland). The most common symptoms are goiter and tachycardia. It has also been linked to some cases of attention deficit hyperactivity disorder (ADHD), although the majority of people with that diagnosis have no thyroid problems.[7]
An association with depression has been proposed.[8]
Diagnosis
The characteristic blood test results for this disorder can also be found in other disorders (for example TSH-oma (pituitary adenoma), or other pituitary disorders). The diagnosis may involve identifying a mutation of the thyroid receptor, which is present in approximately 85% of cases.[9]
Yet, since discovery of resistance to thyroid hormones in the absence of thyroid hormone receptor beta mutations, lack of a mutation in a patient does not rule out resistance.[10]
References
- 1 2 Refetoff S, DeWind LT, DeGroot LJ (1967). "Familial syndrome combining deaf-mutism, stuppled epiphyses, goiter and abnormally high PBI: possible target organ refractoriness to thyroid hormone". J. Clin. Endocrinol. Metab. 27 (2): 279–94. doi:10.1210/jcem-27-2-279. PMID 4163616.
- ↑ Weiss RE, Dumitrescu A, Refetoff S (2010). "Approach to the patient with resistance to thyroid hormone and pregnancy". J. Clin. Endocrinol. Metab. 95: 3094–102. doi:10.1210/jc.2010-0409. PMC 2928892
 . PMID 20610605.
. PMID 20610605. - ↑ Refetoff, Samuel; Bassett, J.H.; Beck-Peccoz, Paolo; Bernal, Juan; Brent, Gregory; Chatterjee, Krishna; De Groot, Leslie J.; Dumitrescu, Alexandra M.; Jameson, J. Larry; Kopp, Peter A.; Murata, Yoshiharu; Persani, Luca; Samarut, Jacques; Weiss, Roy E.; Williams, Graham R.; Yen, Paul M. (March 2014). "Classification and Proposed Nomenclature for Inherited Defects of Thyroid Hormone Action, Cell Transport, and Metabolism". Eur Thyroid J. 24 (3): 407–409. doi:10.1159/000358180.
- ↑ "Thyroid hormone resistance caused by a novel deleterious variant of the thyroid hormone receptor beta gene". European Journal of Obstetrics. 167: 118–119. doi:10.1016/j.ejogrb.2012.11.001.
- 1 2 Refetoff S, Dumitrescu AM (2007). "Syndromes of reduced sensitivity to thyroid hormone: genetic defects in hormone receptors, cell transporters and deiodination". Best Pract. Res. Clin. Endocrinol. Metab. 21 (2): 277–305. doi:10.1016/j.beem.2007.03.005. PMID 17574009.
- ↑ LaFranchi SH, et al. (2003). "Follow-up of newborns with elevated screening T4 concentrations". Pediatr. 143 (3): 296–301. doi:10.1067/S0022-3476(03)00184-7. PMID 14517508.
- ↑ Hauser P, Zametkin AJ, Martinez P, et al. (1993). "Attention deficit-hyperactivity disorder in people with generalized resistance to thyroid hormone". N. Engl. J. Med. 328 (14): 997–1001. doi:10.1056/NEJM199304083281403. PMID 8450877.
- ↑ Fardella CE, Artigas RA, Gloger S, et al. (2007). "Refractory depression in a patient with peripheral resistance to thyroid hormone (RTH) and the effect of triiodothyronine treatment". Endocrine. 31 (3): 272–8. doi:10.1007/s12020-007-0042-7. PMID 17906375.
- ↑ Bottcher Y, Paufler T, Stehr T, Bertschat FL, Paschke R, Koch CA (2007). "Thyroid hormone resistance without mutations in thyroid hormone receptor beta". Med. Sci. Monit. 13 (6): CS67–70. PMID 17534237.
- ↑ Tjørve E, Tjørve KM, Olsen JO, Senum R, Oftebro H (2007). "On commonness and rarity of thyroid hormone resistance: a discussion based on mechanisms of reduced sensitivity in peripheral tissues". Med. Hypotheses. 69 (4): 913–21. doi:10.1016/j.mehy.2006.12.056. PMID 17383828.