Loop diuretic
Loop diuretics are diuretics that act at the ascending limb of the loop of Henle in the kidney. They are primarily used in medicine to treat hypertension and edema often due to congestive heart failure or renal insufficiency. While thiazide diuretics are more effective in patients with normal kidney function, loop diuretics are more effective in patients with impaired kidney function.[1]
Mechanism of action
Loop diuretics act on the Na+-K+-2Cl− symporter (cotransporter) in the thick ascending limb of the loop of Henle to inhibit sodium, chloride and potassium reabsorption. This is achieved by competing for the Cl− binding site. Because magnesium and calcium reabsorption in the thick ascending limb is dependent on the positive lumen voltage gradient set up by potassium recycling through renal outer medullary potassium channel, loop diuretics also inhibit their reabsorption. By disrupting the reabsorption of these ions, loop diuretics prevent the generation of a hypertonic renal medulla.[2] Without such a concentrated medulla, water has less of an osmotic driving force to leave the collecting duct system, ultimately resulting in increased urine production. Loop diuretics cause a decrease in the renal blood flow by this mechanism. This diuresis leaves less water to be reabsorbed into the blood, resulting in a decrease in blood volume.
A secondary effect of loop diuretics is to increase the production of prostaglandins, which results in vasodilation and increased blood supply to the kidney.[3][4] NSAIDs block the COX pathway that synthesizes prostaglandins, so NSAIDs can reduce the efficacy of loop diuretics.[5]
The collective effects of decreased blood volume and vasodilation decrease blood pressure and ameliorate edema.
Clinical use
Loop diuretics are principally used in the following indications:[6]
- edema associated with heart failure, liver cirrhosis, kidney impairment, nephrotic syndrome
- hypertension
- adjunct in cerebral/pulmonary edema where rapid diuresis is required (IV injection)
They are also sometimes used in the management of severe hypercalcemia in combination with adequate rehydration.[6]
On the other hand, in critically ill patients with acute renal failure, loop diuretics do not appear to reduce mortality, reduce length of intensive care unit or hospital stay, or hasten any recovery of renal function.[7]
A systematic review by the Cochrane Hypertension group assessing the anti-hypertensive effects of loop diuretics found only a modest reduction in blood pressure compared to placebo; the review highlights the need for more randomized control trials to be made available in order to construct a furnished assessment.[8]
Loop diuretic resistance
Renal insufficiency causes decreased bloodflow to the kidneys, which decreases the glomerular filtration rate (GFR) and reduces the ability of loop diuretics to reach their target organ, the loop of Henle. Similarly, non-steroidal anti-inflammatory drugs also decrease GFR with comparable results. In patients with reduced GFR, ceiling dosages of loop diuretics are increased proportional to the decrease in GFR. Simultaneous treatment with a thiazide diuretic such as hydrochlorothiazide (to inhibit sodium reabsorption at multiple sites in the nephron) is often successful. Newly emerging evidence shows that glucocorticoids may be used to reverse the loop diuretic resistance in heart failure.[9][10]
Patients with congestive heart failure tend to retain sodium, also necessitating an increase in dosage. The same is true for patients with increased sodium intake.
Adverse effects
The most common adverse drug reactions (ADRs) are dose-related and arise from the effect of loop diuretics on diuresis and electrolyte balance.
Common ADRs include: hyponatremia, hypokalemia, hypomagnesemia, dehydration, hyperuricemia, gout, dizziness, postural hypotension, syncope.[6] The loss of magnesium as a result of loop diuretics has also been suggested as a possible cause of pseudogout (chondrocalcinosis)[11]
Infrequent ADRs include: dyslipidemia, increased serum creatinine concentration, hypocalcemia, rash.
Ototoxicity (damage to the ear) is a serious, but rare ADR associated with use of loop diuretics. This may be limited to tinnitus and vertigo, but may result in deafness in serious cases.
Loop diuretics may also precipitate kidney failure in patients concurrently taking an NSAID and an ACE inhibitor—the so-called "triple whammy" effect.[12]
Because furosemide, torsemide and bumetanide are technically sulfa drugs, there is a theoretical risk that patients sensitive to sulfonamides may be sensitive to these loop diuretics. This risk is stated on drug packaging inserts. However, the actual risk of crossreactivity is largely unknown and there are some sources that dispute the existence of such cross reactivity.[13][14] In one study it was found that only 10% of patients with allergy to antibiotic sulfonamides were also allergic to diuretic sulfonamides, but it is unclear if this represents true cross reactivity or the nature of being prone to allergy.[15]
Ethacrynic acid is the only drug of this class that is not a sulfonamide. It has a distinct complication of being associated with gastrointestinal toxicity.[16]
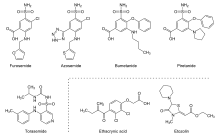
Examples of loop diuretics
| Loop Diuretic | Relative Potency |
|---|---|
| Furosemide | 40 mg |
| Bumetanide | 1 mg |
| Ethacrynic Acid | 50 mg |
| Torsemide | 20 mg |
References
- ↑ Wile, D (Sep 2012). "Diuretics: a review.". Annals of Clinical Biochemistry. 49 (Pt 5): 419–31. doi:10.1258/acb.2011.011281. PMID 22783025.
- ↑ Rose, BD (Feb 1991). "Diuretics.". Kidney International. 39 (2): 336–52. doi:10.1038/ki.1991.43. PMID 2002648.
- ↑ Liguori, A.; A. Casini; M. Di Loreto; I. Andreini; C. Napoli (1999). "Loop diuretics enhance the secretion of prostacyclin in vitro, in healthy persons, and in patients with chronic heart failure". European Journal of Clinical Pharmacology. 55 (2): 117–124. doi:10.1007/s002280050605. ISSN 0031-6970. PMID 10335906.
- ↑ Miyanoshita, A.; M. Terada; H. Endou (1989). "Furosemide directly stimulates prostaglandin E2 production in the thick ascending limb of Henle's loop". The Journal of Pharmacology and Experimental Therapeutics. 251 (3): 1155–1159. ISSN 0022-3565. PMID 2600809.
- ↑ Nies, A. S. (1988). "Renal effects of nonsteroidal anti-inflammatory drugs". Agents and Actions. Supplements. 24: 95–106. doi:10.1007/978-3-0348-9160-8_9. ISSN 0379-0363. PMID 3142236.
- 1 2 3 Rossi S, ed. (2004). Australian Medicines Handbook 2004 (5th ed.). Adelaide, S.A.: Australian Medicines Handbook Pty Ltd. ISBN 0-9578521-4-2.
- ↑ Davis, A. (2006). "The use of loop diuretics in acute renal failure in critically ill patients to reduce mortality, maintain renal function, or avoid the requirements for renal support". Emergency Medicine Journal. 23 (7): 569–70. doi:10.1136/emj.2006.038513. PMC 2579558
 . PMID 16794108.
. PMID 16794108. - ↑ Musini, VM; Rezapour, P; Wright, JM; Bassett, K; Jauca, CD (2015). "Blood pressure-lowering efficacy of loop diuretics for primary hypertension". Cochrane Database of Systematic Reviews (5): CD003825. doi:10.1002/14651858.CD003825.pub4.
- ↑ Liu, C; Liu, G; Zhou, C; Ji, Z; Zhen, Y; Liu, K (September 2007). "Potent diuretic effects of prednisone in heart failure patients with refractory diuretic resistance.". The Canadian Journal of Cardiology. 23 (11): 865–8. doi:10.1016/s0828-282x(07)70840-1. PMC 2651362
 . PMID 17876376.
. PMID 17876376. - ↑ Massari, F; Mastropasqua, F; Iacoviello, M; Nuzzolese, V; Torres, D; Parrinello, G (March 2012). "The glucocorticoid in acute decompensated heart failure: Dr Jekyll or Mr Hyde?". The American Journal of Emergency Medicine. 30 (3): 517.e5–10. doi:10.1016/j.ajem.2011.01.023. PMID 21406321.
- ↑ Rho YH, Zhu Y, Zhang Y, Reginato AM, Choi HK. Risk factors for pseudogout in the general population. Rheumatology 2012;51:2070-2074 doi:10.1093/rheumatology/kes204
- ↑ Thomas MC (February 2000). "Diuretics, ACE inhibitors and NSAIDs--the triple whammy". Med. J. Aust. 172 (4): 184–5. PMID 10772593.
- ↑ Phipatanakul, Wanda; N. Franklin Adkinson (2000). "Cross-Reactivity Between Sulfonamides and Loop or Thiazide Diuretics: Is it a Theoretical or Actual Risk?". Allergy & Clinical Immunology International. 12 (1): 26–28. doi:10.1027/0838-1925.12.1.26. ISSN 1097-1424. PMC 3365608
 . PMID 22661885.
. PMID 22661885. - ↑ Rachoin, Jean-Sebastien; Elizabeth A. Cerceo (2011). "Four nephrology myths debunked". Journal of Hospital Medicine. 6 (5): –1–5. doi:10.1002/jhm.703. ISSN 1553-5606. PMID 21661096.
- ↑ Strom, Brian L.; Rita Schinnar; Andrea J. Apter; David J. Margolis; Ebbing Lautenbach; Sean Hennessy; Warren B. Bilker; Dan Pettitt (2003-10-23). "Absence of cross-reactivity between sulfonamide antibiotics and sulfonamide nonantibiotics". The New England Journal of Medicine. 349 (17): 1628–1635. doi:10.1056/NEJMoa022963. ISSN 1533-4406. PMID 14573734.
- ↑ Laragh, John H.; Paul J. Cannon; William B. Stason; Henry O. Heinemann (1966). "Physiologic and Clinical Observations on Furosemide and Ethacrynic Acid*". Annals of the New York Academy of Sciences. 139 (2): 453–465. doi:10.1111/j.1749-6632.1966.tb41219.x. ISSN 1749-6632. Retrieved 2015-01-09.
- ↑ al.], ed. Laurence L. Brunton ... [et (2011). Goodman & Gilman's pharmacological basis of therapeutics. (12th ed.). New York: McGraw-Hill. ISBN 978-0071624428.
External links
- Loop Diuretic, from the Family Practice Notebook
- Loop Diuretics at the US National Library of Medicine Medical Subject Headings (MeSH)