Pectus excavatum
| Pectus excavatum | |
|---|---|
 | |
| An example of a severe case | |
| Classification and external resources | |
| Specialty | Orthopedics |
| ICD-10 | Q67.6 |
| ICD-9-CM | 754.81 |
| OMIM | 169300 |
| DiseasesDB | 29401 |
| MedlinePlus | 003320 |
| eMedicine | ped/2558 |
| MeSH | D005660 |
Pectus excavatum is a congenital deformity of the anterior thoracic wall in which the sternum and rib cage grow abnormally. This produces a caved-in or sunken appearance of the chest.[1] It can either be present at birth or not develop until puberty.
Pectus excavatum is sometimes considered to be cosmetic but depending on the severity, it can impair cardiac and respiratory function and cause pain in the chest and back.[2] People with the condition may experience negative psychosocial effects, and avoid activities that expose the chest.[3]
Pectus excavatum is from Latin meaning hollowed chest.[4] It is sometimes referred to as cobbler's chest or funnel chest.[5][6]
Signs and symptoms
The hallmark of the condition is a sunken appearance of the sternum. The most common form is a cup-shaped concavity, involving the lower end of the sternum; also a broader concavity involving the upper costal cartilages is possible.[7] The lower-most ribs may protrude ("flared ribs").[8] Pectus excavatum defects may be symmetric or asymmetric.
Patients may also experience chest and back pain, which is usually of musculoskeletal origin.[9]
In mild cases, cardiorespiratory function is normal, although the heart can be displaced and/or rotated.[10] In severe cases, mitral valve prolapse may be present and physical capability may be limited due to base lung capacity being decreased.[11]
Psychological symptoms manifest with feelings of embarrassment, social anxiety, shame, limited capacity for activities and communication, negativity, intolerance, frustration, and even depression.[12]
Causes
Researchers are unsure of the cause of pectus excavatum but assume that there is a genetic component for at least some of the cases. Approximately 37% of individuals with pectus excavatum have a first degree family member with the condition.[1] A number of genetic markers for pectus excavatum have also been discovered.[13] Physiologically, increased pressure in utero, rickets and increased traction on the sternum due to abnormalities of the diaphragm have been postulated as specific mechanisms.[1]
Pectus excavatum is also a relatively common symptom of Noonan syndrome, Marfan syndrome[14] and Loeys-Dietz syndrome and sometimes is found in other connective tissue disorders such as Ehlers–Danlos Syndrome.[15] Many children with spinal muscular atrophy develop pectus excavatum due to the diaphragmatic breathing that is common with the disease. Pectus excavatum also occurs in about 1% of persons diagnosed with celiac disease for unknown reasons.
Pathophysiology
Because the heart is located behind the sternum, and because individuals with pectus excavatum have been shown to have visible deformities of the heart (seen both on radiological imaging and after autopsies), it has been hypothesized that there is impairment of function of the cardiovascular system in individuals with pectus excavatum. While some studies have demonstrated decreased cardiovascular function in pectus excavatum, there has been no consensus reached based on newer physiological tests (such as echocardiography) of the presence or degree of impairment in cardiovascular function in people with pectus excavatum. Similarly, there is no consensus on the degree of functional improvement after corrective surgery;[1] a 2013 meta-analysis yielded conflicting results.[16]
Diagnosis
Pectus excavatum is initially suspected from visual examination of the anterior chest. Auscultation of the chest can reveal displaced heart beat and valve prolapse. There can be a heart murmur occurring during systole caused by proximity between the sternum and the pulmonary artery.[17] Lung sounds are usually clear yet diminished due to decreased base lung capacity.[18]
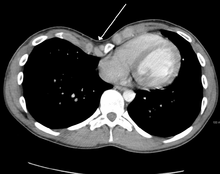
Many scales have been developed to determine the degree of deformity in the chest wall. Most of these are variants on the distance between the sternum and the spine. One such index is the Backer ratio which grades severity of deformity based on the ratio between the diameter of the vertebral body nearest to xiphosternal junction and the distance between the xiphosternal junction and the nearest vertebral body.[19] More recently the Haller index has been used based on CT scan measurements. An index over 3.25 is often defined as severe.[20] The Haller index is the ratio between the horizontal distance of the inside of the ribcage and the shortest distance between the vertebrae and sternum.[21]

Chest x-rays are also useful in the diagnosis. The chest x-ray in pectus excavatum can show an opacity in the right lung area that can be mistaken for an infiltrate (such as that seen with pneumonia).[22] Some studies also suggest that the Haller index can be calculated based on chest x-ray as opposed to CT scanning in individuals who have no limitation in their function.[23]
Pectus excavatum is differentiated from other disorders by a series of elimination of signs and symptoms. Pectus carinatum is excluded by the simple observation of a collapsing of the sternum rather than a protrusion. Kyphoscoliosis is excluded by diagnostic imaging of the spine, where in pectus excavatum the spine usually appears normal in structure.
Treatment
Pectus excavatum requires no corrective procedures in mild cases.[24] Treatment of severe cases can involve either invasive or non-invasive techniques or a combination of both. Before an operation proceeds several tests are usually to be performed. These include, but are not limited to, a CT scan, pulmonary function tests, and cardiology exams (such as auscultation and ECGs).[2] After a CT scan is taken the Haller index is measured. The patient's Haller is calculated by obtaining the ratio of the transverse diameter (the horizontal distance of the inside of the ribcage) and the anteroposterior diameter (the shortest distance between the vertebrae and sternum).[25] A Haller Index of greater than 3.25 is generally considered severe, while normal chest has an index of 2.5.[21][26][27] The cardiopulmonary tests are used to determine the lung capacity and to check for heart murmurs.
Exercise
Physical exercise is not seen as a means to resolve the condition on its own, but has an important role in pectus excavatum treatment programs. It is used in order to halt or slow the progression of mild or moderate excavatum conditions[28][29] and as supplementary treatment to improve a poor posture, to prevent secondary complications, and to prevent relapse after treatment.[30]
Exercises are aimed at improving posture, strengthening back and chest muscles, and enhancing exercise capacity, ideally also increasing chest expansion.[31] Pectus exercises include deep breathing and breath holding exercises,[28] as well as strength training for the back and chest muscles. Additionally, aerobic exercises to improve cardiopulmonary function are employed.[29]
(In exception to this general approach, patients in whom a bar has been surgically implanted via the Nuss procedure are required to refrain from certain exercises for a number of weeks or months after the intervention in order to avoid a dislocation of the bar.)
Thoracic surgery
Surgical correction has been shown to repair any functional symptoms that may occur in the condition, such as respiratory problems or heart murmurs, provided that permanent damage has not already arisen from an extremely severe case.[2] Surgical correction of the pectus excavatum has been shown to significantly improve cardiovascular function;[32] there is inconclusive evidence so far as to whether it might also improve pulmonary function.[33] One of the most popular techniques for repair of pectus excavatum today is the minimally invasive operation, also known as MIRPE or Nuss technique.[34]
Ravitch technique
The Ravitch technique is an invasive surgery that was introduced in 1949[35] and developed in the 1950s to treat the condition. This procedure involves creating an incision along the chest through which the cartilage is removed and the sternum detached. A small bar is then inserted underneath the sternum to hold it up in the desired position. The bar is left implanted until the cartilage grows back, typically about six months. The bar is subsequently removed in a simple out-patient procedure.
The Ravitch technique is not widely practiced because it is so invasive. It is more often used in older patients, where the sternum has calcified, when the deformity is asymmetrical, or when the less invasive Nuss procedure has proven unsuccessful.[36] The Ravitch procedure is a two-stage procedure (two surgeries, some months apart).
Nuss procedure

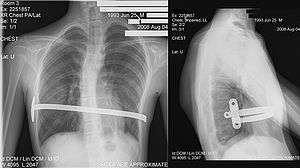
Dr. Donald Nuss, based at Children's Hospital of The King's Daughters in Norfolk, Virginia, performed the first minimally invasive repair of pectus excavatum (MIRPE) in 1987[37] and presented it much later at a conference in 1997.[37][38][39] His procedure, widely known as the Nuss procedure, involves slipping in one or more concave steel bars into the chest, underneath the sternum. The bar is flipped to a convex position so as to push outward on the sternum, correcting the deformity. The bar usually stays in the body for about two years, although many surgeons are now moving toward leaving them in for up to five years. When the bones have solidified into place, the bar is removed through outpatient surgery.
Although initially designed to be performed in younger patients (less than 10 years of age) whose sternum and cartilage is more flexible, there are successful series of Nuss treatment in patients well into their teens and twenties. The Nuss procedure is a two-stage procedure (two surgeries, some years apart).
Robicsek technique
Dr. Francis Robicsek, based at Carolinas HealthCare System in Charlotte, North Carolina, developed the Robicsek procedure in 1965. Each time the procedure is performed, it is individually tailored based on the extent and location of the deformity in the patient. The operation begins with an incision, no more than 4–6 centimeters, to the sternum. The pectoralis major muscles are then detached from the sternum. Using the upper limit of the sternal depression as a guide, the deformed cartilages are removed one-by-one, using sharp and blunt dissection. The lower tip of the sternum is then grabbed with a towel-clip and, using blunt dissection, is freed of tissue connections with the pericardium and the pleura. The sternum is then forcefully bent forward into a corrected position. The Robicsek procedure is a single-stage procedure (one surgery only).
To keep the sternum elevated, a piece of mesh is placed under the mobilized sternum and sutured under moderate tension bilaterally to the stumps of the ribs. After appropriate hemostasis, the pectoralis muscles are united in front of the sternum and the wound is closed without additional drainage. Any pressure-dressing should be avoided. [40] The purported advantage of this technique is that it is less invasive than the Ravitch technique, but critics have suggested that the relapse rate may be high due to cartilage and bone displaying memory phenomenon. There has been controversy as to the best surgical approach for correction of pectus excavatum. It is important for the surgeon to select the appropriate operative approach based on each individual patient's characteristics.[41]
Conservative treatment
The chest wall is elastic, gradually stiffening over age.[42] Non-surgical treatments have been developed that aim at gradually alleviating the pectus excavatum condition, making use of the elasticity of the chest wall, including the costal cartilages, in particular in young patients.
Magnetic mini-mover procedure
The magnetic mini-mover procedure (3MP) is a technique used to correct pectus excavatum by using two magnets to realign the sternum with the rest of the chest and ribcage.[43] One magnet is inserted 1 cm into the patient's body on the lower end of the sternum, the other is placed externally onto a custom fitted brace. These two magnets generate around 0.04 tesla (T) in order to slowly move the sternum outwards over a number of years. The maximum magnetic field that can be applied to the body safely is around 4 T, making this technique safe from a magnetic viewpoint.[43] The 3MP technique's main advantages are that it is more cost-effective than major surgical approaches such as the Nuss procedure and it is considerably less painful postoperatively.
Its effectiveness is limited to younger children in early- to mid-puberty because older patients have less compliant (flexible) chest walls.[44] One potential adverse interaction with other medical devices is possible inactivation of artificial pacemakers if present.
Vacuum bell

A relatively new alternative to surgery is the vacuum bell, also referred to as treatment by cup suction. It consists of a bowl shaped device which fits over the caved-in area; the air is then removed by the use of a hand pump.[45] The vacuum created by this lifts the sternum upwards, lessening the severity of the deformity.[46] It has been proposed as an alternative to surgery in less severe cases.[47] Once the defect visually disappears, two additional years of use of the vacuum bell is required to make what may be a permanent correction.[48][49] The treatment, in combination with physiotherapy exercises, has been judged by some as "a promising useful alternative" to surgery provided the thorax is flexible; the duration of treatment that is required has been found to be "directly linked to age, severity and the frequency of use".[50] Long-term results are still lacking.[47][50]
The vacuum bell can also be used in preparation to surgery.[47]
Orthoses
Brazilian orthopedist Sydney Haje developed a non-surgical protocol for treating pectus carinatum as well as pectus excavatum. The method involves wearing a compressive orthosis and adhering to an exercise protocol.[51]
Mild cases have also reportedly been treated with corset-like orthopedic support vests and exercise.[52][53]
Plastic surgery
Custom-made implants
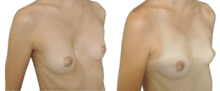

The implant allows pectus excavatum to be treated from a purely morphological perspective. Today it is used as a benchmark procedure as it is simple, reliable, minimally intrusive and without any risk of injury or complications, while offering aesthetically-pleasing results.[54] This procedure does not, however, claim to correct existing cardiac and respiratory problems which, in very rare cases, can be triggered by the pectus excavatum condition. For female sufferers, the potential resulting breast asymmetry can be partially or completely corrected by this procedure.[55]
The process of creating a plaster-cast model, directly on the skin of the patient’s thorax, can be used in the design of the implants. The evolution of medical imaging and CAD (computer-aided design)[56] now allows customised 3D implants to be designed directly from the ribcage, therefore being much more precise, easier to place sub-pectorally and perfectly adapted to the shape of each patient.[57] The implants are made of medical silicon rubber which is age-resistant and unbreakable (different to the silicon gel used in breast implants). They will last for life (apart from the rare case of an adverse reaction) and are not visible externally.
The surgery is performed under general anesthesia and takes an hour (a single procedure, where no material is removed). The surgeon makes an incision of approximately seven centimetres, prepares the customised space in the chest, inserts the implant deep beneath the muscle, then closes the incision in three steps without draining. Hospitalization is three days maximum.
The recovery after the surgery is not very painful and only requires mild pain relief. Post-operative care is minimal: a dressing is required for eight days and compression vest for a month following the procedure. A check-up appointment is carried out after eight days for puncture of seroma. The patient can resume normal activities relatively quickly – he can return to work after 15 days and participate in any sporting activities after three months.
Lipofilling
The "lipofilling" technique consists of sucking fat from the patient using a syringe with a large gauge needle (usually from the abdomen or the outer thighs), then after centrifugation, the fat cells are re-injected beneath the skin into whichever hollow it is needed to fill. This technique is primarily used to correct small defects which may persist after conventional surgical treatment.
Epidemiology
Pectus excavatum occurs in an estimated 1 in 150–1000 births, with male predominance (male-to-female ratio of 3:1). Occurrences of the condition in family members have been reported in 35% to 45% of cases.[18][58]
History
Leonardo da Vinci[59] and Jusepe de Ribera[60] may have exhibited pectus excavatum. American Olympic swimmer Cody Miller was diagnosed with pectus excavatum and opted not to have treatment.[61][62][63]
Other animals
Pectus excavatum is also known to occur in animals, e.g. the Munchkin breed of cat.[64] Some procedures used to treat the condition in animals have not been used in human treatments, such as the use of a cast with sutures wrapped around the sternum and the use of internal and external splints.[65][66] These techniques are generally used in immature animals with flexible cartilage.[67]
See also
References
- 1 2 3 4 Shamberger RC (1996). "Congenital chest wall deformities". Current Problems in Surgery (Review). 33 (6): 469–542. doi:10.1016/S0011-3840(96)80005-0. PMID 8641129.
- 1 2 3 Crump HW (1992). "Pectus excavatum". Am Fam Physician (Review). 46 (1): 173–9. PMID 1621629.
- ↑ "Pectus excavatum". MedLine Plus Medical Encyclopedia. U.S. National Library of Medicine and the National Institutes of Health. 2007-11-12.
- ↑ chief lexicographer: Douglas M. Anderson (2003). "Pectus Excavatum". Dorland's Medicla Dictionary (28 ed.). Philadelphia, Penns.: Saunders. ISBN 0-7216-0146-4.
- ↑ "Pectus Excavatum".
- ↑ Spence, Roy A. J.; Patrick J. Morrison (2005). Genetics for Surgeons. Remedica Publishing. ISBN 1-901346-69-2.
- ↑ Blanco FC, Elliott ST, Sandler AD (2011). "Management of congenital chest wall deformities". Seminars in Plastic Surgery (Review). 25 (1): 107–16. doi:10.1055/s-0031-1275177. PMC 3140238
 . PMID 22294949.
. PMID 22294949. - ↑ See for example Bosgraaf RP, Aronson DC (2010). "Treatment of flaring of the costal arch after the minimally invasive pectus excavatum repair (Nuss procedure) in children". Journal of Pediatric Surgery. 45 (9): 1904–6. doi:10.1016/j.jpedsurg.2010.05.037. PMID 20850643.
- ↑ Pectus Excavatum Clinical Presentation: History, Medscape (30 June 2015, retrieved 07 September 2016).
- ↑ Fokin AA, Steuerwald NM, Ahrens WA, Allen KE (2009). "Anatomical, histologic, and genetic characteristics of congenital chest wall deformities". Seminars in Thoracic and Cardiovascular Surgery (Review). 21 (1): 44–57. doi:10.1053/j.semtcvs.2009.03.001. PMID 19632563.
- ↑
- ↑ Brandon, Mike (2016-02-04). "Orthopedic approach to pectus deformities: 32 years of studies". Pectus Excavatum Info. Pediatric Orthopedist and Physiatrist, Orthopectus Clinical Center and Asa Norte Regional Hospital. 2Doctor in Orthopedics, School of Medicine, University de Sāo Paulo, Ribeirāo Preto, SP. Pediatric Orthopedist, Orthopectus Clinical Center. Preceptor, Adult Foot and Pediatric Orthopedics, Federal District Hospital, Brasilia, DF. Retrieved 2016-02-04.
- ↑ Dean C, Etienne D, Hindson D, Matusz P, Tubbs RS, Loukas M (2012). "Pectus excavatum (funnel chest): a historical and current prospective". Surgical and Radiologic Anatomy : SRA. 34 (7): 573–9. doi:10.1007/s00276-012-0938-7. PMID 22323132.
- ↑ "eMedicine — Marfan Syndrome". Harold Chen.
- ↑ Creswick HA1, Stacey MW, Kelly RE Jr, Gustin T, Nuss D, Harvey H, Goretsky MJ, Vasser E, Welch JC, Mitchell K, Proud VK (October 2006). "Family study of the inheritance of pectus excavatum". Journal of Pediatric Surgery. 41 (10): 1699–703. doi:10.1016/j.jpedsurg.2006.05.071. PMID 17011272.
- ↑ Jayaramakrishnan K, Wotton R, Bradley A, Naidu B (2013). "Does repair of pectus excavatum improve cardiopulmonary function?". Interact Cardiovasc Thorac Surg (Review). 16 (6): 865–70. doi:10.1093/icvts/ivt045. PMC 3653464
 . PMID 23449664.
. PMID 23449664. - ↑ Guller B, Hable K (1974). "Cardiac findings in pectus excavatum in children: review and differential diagnosis". Chest. 66 (2): 165–71. doi:10.1378/chest.66.2.165. PMID 4850886.
- 1 2 "eMedicine — Pectus Excavatum". Andre Hebra.
- ↑ BACKER OG, BRUNNER S, LARSEN V (1961). "The surgical treatment of funnel chest. Initial and follow-up results". Acta chirurgica Scandinavica. 121: 253–61. PMID 13685690.
- ↑ Jeannette Diana-Zerpa; Nancy Thacz Browne; Laura M. Flanigan; Carmel A. McComiskey; Pam Pieper (2006). Nursing Care of the Pediatric Surgical Patient (Browne, Nursing Care of the Pediatric Surgical Patient). Sudbury, Mass: Jones & Bartlett Publishers. p. 253. ISBN 0-7637-4052-7.
- 1 2 Haller JA, Kramer SS, Lietman SA (1987). "Use of CT scans in selection of patients for pectus excavatum surgery: a preliminary report". Journal of Pediatric Surgery. 22 (10): 904–6. doi:10.1016/S0022-3468(87)80585-7. PMID 3681619.
- ↑ Hoeffel JC, Winants D, Marcon F, Worms AM (1990). "Radioopacity of the right paracardiac lung field due to pectus excavatum (funnel chest)". Rontgenblatter. 43 (7): 298–300. PMID 2392647.
- ↑ Mueller C, Saint-Vil D, Bouchard S (2008). "Chest x-ray as a primary modality for preoperative imaging of pectus excavatum". Journal of Pediatric Surgery. 43 (1): 71–3. doi:10.1016/j.jpedsurg.2007.09.023. PMID 18206458.
- ↑ Klingman, RM (2011). Nelson Texbook of Pediatrics. Philadelphia, PA: Elsevier.
- ↑ "How the Haller is measured. Departament of Cardiology and Pulmonology of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo – Thoracic Surgery Sector" (PDF).
- ↑ "The Nuss procedure for pectus excavatum correction | AORN Journal". Barbara Swoveland, Clare Medrick, Marilyn Kirsh, Kevin G. Thompson, Nussm Donald. 2001.
- ↑ "Pectus Excavatum overview" (PDF). CIGNA.
- 1 2 Peter Mattei (15 February 2011). Fundamentals of Pediatric Surgery. Springer Science & Business Media. p. 315. ISBN 978-1-4419-6643-8.
- 1 2 Anton H. Schwabegger (15 September 2011). Congenital Thoracic Wall Deformities: Diagnosis, Therapy and Current Developments. Springer Science & Business Media. p. 118. ISBN 978-3-211-99138-1.
- ↑ George W. Holcomb III; Jerry D Murphy; Daniel J Ostlie (31 January 2014). Ashcraft's Pediatric Surgery. Elsevier Health Sciences. p. 270. ISBN 978-0-323-18736-7.
- ↑ Lewis Spitz; Arnold Coran (21 May 2013). Operative Pediatric Surgery, Seventh Edition. CRC Press. p. 251. ISBN 978-1-4441-1715-8.
- ↑ Malek MH, Berger DE, Housh TJ, Marelich WD, Coburn JW, Beck TW (2006). "Cardiovascular function following surgical repair of pectus excavatum: a metaanalysis". Chest (Meta-Analysis). 130 (2): 506–16. doi:10.1378/chest.130.2.506. PMID 16899852.
- ↑ Malek MH, Berger DE, Marelich WD, Coburn JW, Beck TW, Housh TJ (2006). "Pulmonary function following surgical repair of pectus excavatum: a meta-analysis". European Journal of Cardio-Thoracic Surgery (Meta-Analysis). 30 (4): 637–43. doi:10.1016/j.ejcts.2006.07.004. PMID 16901712.
- ↑ Hebra A (2009). "Minimally invasive repair of pectus excavatum". Semin Thorac Cardiovasc Surg (Review). 21 (1): 76–84. doi:10.1053/j.semtcvs.2009.04.005. PMID 19632566.
- ↑ Ravitch MM (April 1949). "The Operative Treatment of Pectus Excavatum". Ann Surg. 129 (4): 429–44. doi:10.1097/00000658-194904000-00002. PMC 1514034
 . PMID 17859324.
. PMID 17859324. - ↑ Theresa D. Luu MD (November 2009). "Surgery for Recurrent Pectus Deformities". The Annals of Thoracic Surgery. 88 (5): 1627–1631. doi:10.1016/j.athoracsur.2009.06.008. PMID 19853122.
- 1 2 Adam J. Białas; Bogumiła Kempińska-Mirosławska (2013). "Minimally invasive repair of pectus excavatum (the Nuss procedure) in Poland and worldwide – a summary of 25 years of history" (PDF). Kardiochirurgia i Torakochirurgia Polska 2013. pp. 42–47. doi:10.5114/kitp.2013.34304. Retrieved 13 April 2016.
- ↑ Nuss D, Kelly RE Jr, Croitoru DP, Katz ME (April 1998). "A 10-year review of a minimally invasive technique for the correction of pectus excavatum". J Pediatr Surg. 33 (4): 545–52. doi:10.1016/S0022-3468(98)90314-1. PMID 9574749.
- ↑ Pilegaard, HK; Licht PB (February 2008). "Early results following the Nuss operation for pectus excavatum—a single-institution experience of 383 patients". Interactive Cardiovascular and Thoracic Surgery. Oxford University Press. 7 (1): 54–57. doi:10.1510/icvts.2007.160937. PMID 17951271. Retrieved 2008-04-18.
- ↑ Robiscek, Francis. "Marlex Mesh Support For The Correction Of Very Severe And Recurrent Pectus Excavatum". 26 (1): 80–83.
- ↑ Robicsek, Hebra (2009). "To Nuss or not to Nuss? Two opposing views". 21 (1): 85–88. doi:10.1053/j.semtcvs.2009.03.007. PMID 19632567.
- ↑ "Lung elasticity, thorax and age". Retrieved 14 April 2016.
- 1 2 Harrison MR, Estefan-Ventura D, et al. (January 2007). "Magnetic Mini-Mover Procedure for pectus excavatum: I. Development, design, and simulations for feasibility and safety" (PDF). Journal of Pediatric Surgery. 42 (1): 81–85. doi:10.1016/j.jpedsurg.2006.09.042. PMID 17208545. Retrieved 2008-04-23.
- ↑ Harrison, MR; Michael R. Harrison; Kelly D. Gonzales; Barbara J. Bratton; Darrell Christensen; Patrick F. Curran; Richard Fechter; Shinjiro Hirose (January 2012). "Magnetic mini-mover procedure for pectus excavatum III: safety and efficacy in a Food and Drug Administration-sponsored clinical trial". Journal of Pediatric Surgery. 47 (1): 154–9. doi:10.1016/j.jpedsurg.2011.10.039. PMID 22244409. Retrieved 2014-08-20.
- ↑ chkd, Children's Hospital of the King's Daughters
- ↑ Haecker, FM; Mayr J (April 2006). "The vacuum bell for treatment of pectus excavatum: an alternative to surgical correction?". European Journal of Cardio-Thoracic Surgery. 29 (4): 557–561. doi:10.1016/j.ejcts.2006.01.025. PMID 16473516.
- 1 2 3 Brochhausen C, Turial S, Müller FK, Schmitt VH, Coerdt W, Wihlm JM, Schier F, Kirkpatrick CJ (2012). "Pectus excavatum: history, hypotheses and treatment options". Interactive Cardiovascular and Thoracic Surgery (Review). 14 (6): 801–6. doi:10.1093/icvts/ivs045. PMC 3352718
 . PMID 22394989.
. PMID 22394989. - ↑ Non-surgical sunken chest treatment device may eliminate surgery, Mass Device, November 2012
- ↑ Raver-Lampman (November 2012), First patients in US receive non-surgical device of sunken chest syndrome, AAAS
- 1 2 Lopez M, Patoir A, Costes F, Varlet F, Barthelemy JC, Tiffet O (2016). "Preliminary study of efficacy of cup suction in the correction of typical pectus excavatum". Journal of Pediatric Surgery (Review). 51 (1): 183–7. doi:10.1016/j.jpedsurg.2015.10.003. PMID 26526206.
- ↑ Haje SA, de Podestá Haje D (2009). "Orthopedic Approach to Pectus Deformities: 32 Years of Studies". Revista Brasileira De Ortopedia. 44 (3): 191–8. doi:10.1016/S2255-4971(15)30067-7. PMC 4783668
 . PMID 27004171.
. PMID 27004171. - ↑ "LaceIT PE Brace". Advanced Orthotic Designs, Inc.
- ↑ "Orthopectus". Dr. Sydney A. Haje, Ortopedista.
- ↑ André, M. Dahan, E. Bozonnet, I. Garrido, J.-L. Grolleau, J.-P. Chavoin; Pectus excavatum : correction par la technique de comblement avec mise en place d’une prothèse en silicone sur mesure en position rétromusculaire profonde; Encycl Méd Chir, Elsevier Masson SAS - Techniques chirurgicales - Chirurgie plastique reconstructrice et esthétique, 45-671, Techniques chirurgicales - Thorax, 42-480, 2010.
- ↑ Ho Quoc Ch, Chaput B, Garrido I, André A, Grolleau JL, Chavoin JP; Management of breast asymmetry associated with primary funnel chest; Ann Chir Plast Esthet. Elsevier Masson SAS; 2012 Aug 8:1–6.
- ↑ http://www.anatomikmodeling.com/en
- ↑ J-P. Chavoin, A.André, E.Bozonnet, A.Teisseyre, J..Arrue, B. Moreno, D. Glangloff, J-L. Grolleau, I.Garrido; Mammary implant selection or chest implants fabrication with computer help; Ann.de chirurgie plastique esthétique (2010) 55,471-480.
- ↑ "Pectus Excavatum: Frequently Asked Questions: Surgery: UI Health Topics". Harold M. Burkhart and Joan Ricks-McGillin.
- ↑ Ashrafian, Hutan (2013). "Leonardo da Vinci and the first portrayal of pectus excavatum". Thorax. doi:10.1136/thoraxjnl-2013-203224.
- ↑ Davide Lazzeri; Fabio Nicoli (22 February 2016). "Pectus Excavatum in paintings by Jusepe de Ribera (1591–1652)". Thorax. doi:10.1136/thoraxjnl-2015-208236.
- ↑ {{ |url= http://www.raredr.com/news/rare-disease-rio-cm}}
- ↑ Cody Miller – National Team swimmer profile at USASwimming.org
- ↑ Woods, David (27 June 2016). "Cody Miller is IU's first U.S. Olympic swimmer in 40 years". Indianapolis Star. Retrieved 9 August 2016.
- ↑ "Genetic Anomalies of Cats".
- ↑ Fossum, TW; Boudrieau RJ; Hobson HP; Rudy RL (1989). "Surgical correction of pectus excavatum, using external splintage in two dogs and a cat". Journal of the American Veterinary Medical Association. 195 (1): 91–7. PMID 2759902.
- ↑ Risselada M, de Rooster H, Liuti T, Polis I, van Bree H (2006). "Use of internal splinting to realign a noncompliant sternum in a cat with pectus excavatum". Journal of the American Veterinary Medical Association. 228 (7): 1047–52. doi:10.2460/javma.228.7.1047. PMID 16579783.
- ↑ McAnulty JF, Harvey CE (1989). "Repair of pectus excavatum by percutaneous suturing and temporary external coaptation in a kitten". Journal of the American Veterinary Medical Association. 194 (8): 1065–7. PMID 2651373.
Further reading
- Tocchioni F, Ghionzoli M, Messineo A, Romagnoli P (2013). "Pectus excavatum and heritable disorders of the connective tissue". Pediatric Reports (Review). 5 (3): e15. doi:10.4081/pr.2013.e15. PMC 3812532
 . PMID 24198927.
. PMID 24198927. - Jaroszewski D, Notrica D, McMahon L, Steidley DE, Deschamps C (2010). "Current management of pectus excavatum: a review and update of therapy and treatment recommendations". Journal of the American Board of Family Medicine : JABFM (Review). 23 (2): 230–9. doi:10.3122/jabfm.2010.02.090234. PMID 20207934.
External links
| Wikimedia Commons has media related to Pectus excavatum. |
| Look up pectus in Wiktionary, the free dictionary. |