Peliosis hepatis
| Peliosis hepatis | |
|---|---|
| Classification and external resources | |
| Specialty | gastroenterology |
| ICD-10 | K76.4 |
| MeSH | D010382 |
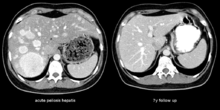
Peliosis hepatis is an uncommon vascular condition characterised by multiple randomly distributed blood-filled cavities throughout the liver. The size of the cavities usually ranges between a few millimetres to 3 cm in diameter.[1] In the past it was a mere histological curiosity occasionally found at autopsies but has been increasingly recognised with wide ranging conditions from AIDS to the use of anabolic steroids. It also occasionally affects spleen, lymph nodes, lungs, kidneys, adrenal glands, bone marrow and other parts of gastrointestinal tract.[2]
Peliosis hepatis is often erroneously written "peliosis hepatitis", despite its not being one of the hepatitides. The correct term arises from the Greek pelios, i.e. discoloured by extravasated blood, livid,[3] and the Latinized genitive case (hepatis[4]) of the Greek hepar, liver.[5]
Pathophysiology
The pathogenesis of peliosis hepatis is unknown. There are several hypotheses, such as, it arises from sinusoidal epithelial damage,[6] increased sinusoidal pressure due to obstruction in blood outflow from the liver, or hepatocellular necrosis.[1]
Two morphologic patterns of hepatic peliosis were described by Yanoff and Rawson.[7] In the phlebectatic type, the blood-filled spaces are lined with endothelium and are associated with aneurysmal dilatation of the central vein; in the parenchymal type, the spaces have no endothelial lining and they usually are associated with haemorrhagic parenchymal necrosis. Some consider both patterns to be one process, initiated by focal necrosis of liver parenchyma, observed in parenchymal type, progressing into formation of fibrous wall and endothelial lining around haemorrhage of phlebectatic type. Fibrosis, cirrhosis, regenerative nodules, and tumours may also be seen.
Disease associations
- Infections: HIV, Bacillary peliosis (caused by genus Bartonella, bacteria responsible for cat-scratch disease which are identified histologically adjacent to the peliotic lesions[8]), Staphylococcus aureus[9]
- Chronic conditions: End stage renal failure, Kwashiorkor, tuberculosis and other chronic infections.
- Malignancy: Monoclonal gammopathies (multiple myeloma and Waldenstrom macroglobulinemia), Hodgkin disease, malignant histiocytosis, seminoma, hepatocellular adenoma and hepatocarcinoma,[10]
- Renal transplants: It can be found in up to 20% patients, can be related to azathioprine or cyclosporine use and may be associated with increased risk of transplant rejection.[11][12]
- Drugs and toxins: Corticosteroids, androgens, azathioprine, tamoxifen[13]
Clinical features
The condition is typically asymptomatic and is discovered following evaluation of abnormal liver function test. However, when severe it can manifest as jaundice, hepatomegaly, liver failure and haemoperitoneum.
Treatment
Usually directed towards management of underlying cause. Withdrawal of azathioprine leads to remission in renal transplant, bacillary peliosis responds to antibiotics. In rare circumstances partial resection of liver or transplant may be required.
Other cystic conditions of liver
- Polycystic liver disease
- Solitary congenital cysts
- Congenital hepatic fibrosis
- Hydatid cyst
- Von Meyenburg complexes
- Caroli disease (type V choledochal cyst)
- Type IV choledochal cysts
References
- 1 2 Sleisenger, Marvin (2006). Sleisenger and Fordtran's Gastrointestinal and Liver Disease. Philadelphia: W.B. Saunders Company. ISBN 1-4160-0245-6. Chapter 80
- ↑ Ichijima K, Kobashi Y, Yamabe H, Fujii Y, Inoue Y (1980). "Peliosis hepatis. An unusual case involving multiple organs". Acta Pathol. Jpn. 30 (1): 109–20. doi:10.1111/j.1440-1827.1980.tb01308.x. PMID 7361545.
- ↑ "Henry George Liddell, Robert Scott, A Greek-English Lexicon". Retrieved 2007-06-11.
- ↑ "Charlton T. Lewis, Charles Short, A Latin Dictionary". Retrieved 2007-07-02.
- ↑ "Henry George Liddell, Robert Scott, A Greek-English Lexicon". Retrieved 2007-07-02.
- ↑ Gushiken FC (2000). "Peliosis hepatis after treatment with 2-chloro-3'-deoxyadenosine". South. Med. J. 93 (6): 625–6. doi:10.1097/00007611-200006000-00020. PMID 10881786.
- ↑ YANOFF M, RAWSON AJ (1964). "PELIOSIS HEPATIS. AN ANATOMIC STUDY WITH DEMONSTRATION OF TWO VARIETIES". Archives of pathology. 77: 159–65. PMID 14088761.
- ↑ Koehler JE, Sanchez MA, Garrido CS, Whitfeld MJ, Chen FM, Berger TG, Rodriguez-Barradas MC, LeBoit PE, Tappero JW (1997). "Molecular epidemiology of bartonella infections in patients with bacillary angiomatosis-peliosis". N. Engl. J. Med. 337 (26): 1876–83. doi:10.1056/NEJM199712253372603. PMID 9407154.
- ↑ Perkocha LA, Geaghan SM, Yen TS, Nishimura SL, Chan SP, Garcia-Kennedy R, Honda G, Stoloff AC, Klein HZ, Goldman RL (1990). "Clinical and pathological features of bacillary peliosis hepatis in association with human immunodeficiency virus infection". N. Engl. J. Med. 323 (23): 1581–6. doi:10.1056/NEJM199012063232302. PMID 2233946.
- ↑ Haboubi NY, Ali HH, Whitwell HL, Ackrill P (1988). "Role of endothelial cell injury in the spectrum of azathioprine-induced liver disease after renal transplant: light microscopy and ultrastructural observations". Am. J. Gastroenterol. 83 (3): 256–61. PMID 3278593.
- ↑ Izumi S, Nishiuchi M, Kameda Y, Nagano S, Fukunishi T, Kohro T, Shinji Y (1994). "Laparoscopic study of peliosis hepatis and nodular transformation of the liver before and after renal transplantation: natural history and aetiology in follow-up cases". J. Hepatol. 20 (1): 129–37. doi:10.1016/S0168-8278(05)80479-9. PMID 8201214.
- ↑ Cavalcanti R, Pol S, Carnot F, Campos H, Degott C, Driss F, Legendre C, Kreis H (1994). "Impact and evolution of peliosis hepatis in renal transplant recipients". Transplantation. 58 (3): 315–6. doi:10.1097/00007890-199408150-00011. PMID 8053054.
- ↑ Goldman, Lee (2003). Cecil Textbook of Medicine -- 2-Volume Set, Text with Continually Updated Online Reference. Philadelphia: W.B. Saunders Company. ISBN 0-7216-4563-1.