Pigmented villonodular synovitis
| Pigmented villonodular synovitis | |
|---|---|
 | |
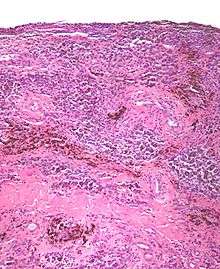
| Micrograph of pigmented villonodular synovitis. H&E stain. | |
| Classification and external resources | |
| Specialty | rheumatology |
| ICD-10 | M12.2 |
| ICD-9-CM | 719.20 |
| DiseasesDB | 29902 |
| MedlinePlus | 3 |
| eMedicine | article/394649 |
| MeSH | D013586 |
Pigmented villonodular synovitis (PVNS) is a joint disease characterized by inflammation and overgrowth of the joint lining. It usually affects the hip or knee. It can also occur in the shoulder, ankle, elbow, hand or foot. In PVNS the lining of the joint, called the synovium, becomes swollen and grows. This growth harms the bone next to the joint. The lining also makes extra fluid that can cause swelling and make movement painful. PVNS is idiopathic, it doesn't seem to run in families or be caused by certain jobs or activities. Surgery can help but, even with treatment, PVNS comes back about half the time. If the pain remains then radiation therapy may help. In the worst cases the joint must be replaced.[1]
Classification
Pigmented villonodular synovitis, described distinctly in 1941 by Charles J. Sutro, L. Lichtenstein, and H.L. Jafe,[2] comes in two forms: localized and diffuse. Diffuse PVNS affects the entire synovium and typically occurs in large joints such as the knee or hip. Localized, or nodular, PVNS is less common than the diffuse form and typically occurs in smaller joints such as the hands and feet. Localized PVNS often arises in the form of a large benign tumour on the tendon sheaths of the joint.[3] As the tumor grows in the joint, it damages the surrounding bone and tissues.[4] Localized PVNS is predominantly found in females and is frequently found in the fingers. Although rare, localized PVNS may develop in large joints. In either case, the knee is the most commonly affected joint (80% of cases), followed by the hip, and less commonly the ankles and shoulders.[3] PVNS is generally found more in men than women.[5] 2 cases per million population; incidence of the localized form is 9 cases per million.
Clinical presentation
In general, pigmented villonodular synovitis often manifests initially as sudden onset, unexplained joint swelling and pain; the joint swelling is disproportionate to the amount of pain the patient feels at first. Decreased motion and increased pain occur as the disorder progresses as well as locking of the joint. The localized form often manifests initially as a painless, slow-growing mass and progresses to the other common symptoms of PVNS. The swelling often feels warm to the touch.[3] Diffuse PVNS symptoms are often confused with those of Rheumatoid arthritis.[4] While pigmented villonodular synovitis can occur in both pediatric and geriatric patients, it is more common with ages 20–50.[3]
Causes
The exact cause is unknown. Some doctors believe it is caused by abnormal metabolism of fat. Others think it may be caused by repetitive inflammation. Some feel that blood within the joint may cause the inflammatory change.[6] Risk factors for PVNS developing are not yet understood. Very little research has been carried out. However, a common theme in patients is a trauma experienced to the joint prior to the onset of symptoms.[7]
Complications
PVNS is locally aggressive and can spread to surrounding tissues, causing bone erosion and tissue damage. If not treated early, it can spread to areas outside the joint, and potentially cause permanent loss of range as well as intense pain.[8][9] The disorder also has, on average, a 45% rate of recurrence.[2]
Diagnosis
PVNS is radiologically diagnosed by magnetic resonance imaging (MRI). The disorder is difficult to identify and is often not diagnosed for four years or more after presentation due to nonspecific symptoms or a general paucity of symptoms.[2]
Pathology
The synovial fluid of the joint is often grossly hemorrhagic.[10]
PVNS, under the microscope, looks as the name of the condition suggests; it is composed on nodules and/or villi and has an abundant number of (pigmented) hemosiderin-laden macrophages.
Treatment
Once PVNS is confirmed by biopsy of the synovium of an affected joint, a synovectomy of the affected area is the most common treatment. Bone lesions caused by the disorder are removed and bone grafting is performed as needed. Because diffuse PVNS has a relatively high rate of recurrence, radiation therapy may be considered as a treatment option. In some cases, a total joint replacement is needed to relieve symptoms when PVNS causes significant joint destruction.[11]
See also
References
- ↑ HAMLIN, BRIAN R.; DUFFY, GAVAN P.; TROUSDALE, ROBERT T.; MORREY, BERNARD F. (1998). "Total Knee Arthroplasty in Patients Who Have Pigmented Villonodular Synovitis". The Journal of Bone & Joint Surgery. 80 (1): 76–82.
- 1 2 3 Frassica FJ, Bhimani MA, McCarthy EF, Wenz J (October 1999). "Pigmented villonodular synovitis of the hip and knee". Am Fam Physician. 60 (5): 1404–10; discussion 1415. PMID 10524485.
- 1 2 3 4 Pigmented Villonodular Synovitis at eMedicine
- 1 2 "Mayclinic". Mayo Clinic. Archived from the original on 2007-06-10. Retrieved 2007-07-15.
- ↑ "Family Doctor.org: PVNS" (web journal). Retrieved 2007-07-15.
- ↑ "A Patient's Guide to Pigmented Villonodular Synovitis (PVNS) of the Knee" (website). Medical MultiMEDIA Group. Retrieved 2013-06-30.
- ↑ Chang, Chong Dr. "Pigmented Villo-Nodular Synovitis (PVNS) of the Knee" (web blog). HC Chang Orthopaedic Surgery. Retrieved 2013-06-29.
- ↑ "Clinical Study". The Stone Clinic. Archived from the original (web journal) on 2007-07-01. Retrieved 2007-08-07.
- ↑ Jabalameli, M; Jamshidi, K; Radi, M; Hadi, H; Bagherifard, A (2014). "Surgical outcomes of 26 patients with pigmented villonodular synovitis (PVNS) of the knee at a mean follow-up of 4 years: Introducing a novel technique". Medical Journal of the Islamic Republic of Iran. 28: 123. PMC 4313448
 . PMID 25679002.
. PMID 25679002. - ↑ Aalberg JR, Hansen P (September 1989). "[Pigmented villonodular synovitis]". Ugeskrift for Læger (in Danish). 151 (38): 2413–6. PMID 2800012.
- ↑ FRANK J. FRASSICA, M.D