Venous thrombosis
| Venous thrombosis | |
|---|---|
 | |
| A deep vein thrombosis in the right leg. Note the swelling and redness. | |
| Classification and external resources | |
| Specialty | cardiology |
| ICD-10 | I80-I82 |
| ICD-9-CM | 453 |
| MeSH | D020246 |
A venous thrombus is a blood clot (thrombus) that forms within a vein. Thrombosis is a term for a blood clot occurring inside a blood vessel. A common type of venous thrombosis is a deep vein thrombosis (DVT), which is a blood clot in the deep veins of the leg. If the thrombus breaks off (embolizes) and flows towards the lungs, it can become a life-threatening pulmonary embolism (PE), a blood clot in the lungs.
When a blood clot breaks loose and travels in the blood, this is called a venous thromboembolism (VTE). The abbreviation DVT/PE refers to a VTE where a deep vein thrombosis (DVT) has moved to the lungs (PE or pulmonary embolism).[1]
An inflammatory reaction is usually present, mainly in the superficial veins and, for this reason this pathology is called most of the time thrombophlebitis. In fact, the inflammatory reaction and the white blood cells play a role in the resolution of venous clots.[2]
Classification
Superficial venous thromboses cause discomfort but generally not serious consequences, as do the deep venous thromboses (DVTs) that form in the deep veins of the legs or in the pelvic veins. Nevertheless, they can progress to the deep veins through the perforator veins or, they can be responsible for a lung embolism mainly if the head of the clot is poorly attached to the vein wall and is situated near the sapheno-femoral junction. Clinical trials suggest that fondaparinux, a factor Xa inhibitor, reduces extension and recurrence of superficial venous thrombosis, and progression to symptomatic embolism.[3]
Since the veins return blood to the heart, if a piece of a blood clot formed in a vein breaks off it can be transported to the right side of the heart, and from there into the lungs. A piece of thrombus that is transported in this way is an embolus: the process of forming a thrombus that becomes embolic is called a thromboembolism. An embolism that lodges in the lungs is a pulmonary embolism (PE). A pulmonary embolism is a very serious condition that can be fatal depending on the dimensions of the embolus. Venous thromboembolism (VTE) refers to both DVTs and PEs.
Systemic embolisms of venous origin can occur in patients with an atrial or ventricular septal defect, through which an embolus may pass into the arterial system. Such an event is termed a paradoxical embolism.
Causes
Venous thrombi are caused mainly by a combination of venous stasis and hypercoagulability—but to a lesser extent endothelial damage and activation.[4] The three factors of stasis, hypercoaguability, and alterations in the blood vessel wall represent Virchow's triad, and changes to the vessel wall are the least understood.[5] Various risk factors increase the likelihood of any one individual developing a thrombosis.
Risk factors
|
|
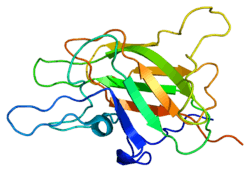 The factor V protein is mutated in carriers of factor V Leiden, which is the most common inherited DVT risk factor.[17] |
The overall absolute risk of venous thrombosis per 100.000 woman years in current use of combined oral contraceptives is approximately 60, compared to 30 in non-users.[18] The risk of thromboembolism varies with different types of birth control pills; Compared with combined oral contraceptives containing levonorgestrel (LNG), and with the same dose of estrogen and duration of use, the rate ratio of deep venous thrombosis for combined oral contraceptives with norethisterone is 0.98, with norgestimate 1.19, with desogestrel (DSG) 1.82, with gestodene 1.86, with drospirenone (DRSP) 1.64, and with cyproterone acetate 1.88.[18] Venous thromboembolism occurs in 100–200 per 100.000 pregnant women every year.[18]
Regarding family history, age has substantial effect modification. For individuals with two or more affected siblings, the highest incidence rates is found among those ≥70 years of age (390 per 100 000 in male and 370 per 100 000 in female individuals), whereas the highest incidence ratios compared to those without affected siblings occurred at much younger ages (ratio of 4.3 among male individuals 20 to 29 years of age and 5.5 among female individuals 10 to 19 years of age).[19]
Pathophysiology
In contrast to the understanding for how arterial thromboses occur, as with heart attacks, venous thrombosis formation is not well understood.[20] With arterial thrombosis, blood vessel wall damage is required for thrombosis formation, as it initiates coagulation,[20] but the majority of venous thrombi form without any injured epithelium.[4]
Red blood cells and fibrin are the main components of venous thrombi,[4] and the thrombi appear to attach to the blood vessel wall endothelium, normally a non-thrombogenic surface, with fibrin.[20] Platelets in venous thrombi attach to downstream fibrin, while in arterial thrombi, they compose the core.[20] As a whole, platelets constitute less of venous thrombi when compared to arterial ones.[4] The process is thought to be initiated by tissue factor-affected thrombin production, which leads to fibrin deposition.[5]
The valves of veins are a recognized site of VT initiation. Due to the blood flow pattern, the base of the valve sinus is particularly deprived of oxygen (hypoxic). Stasis excacerbates hypoxia, and this state is linked to the activation of white blood cells (leukocytes) and the endothelium. Specifically, the two pathways of hypoxia-inducible factor-1 (HIF-1) and early growth response 1 (EGR-1) are activated by hypoxia, and they contribute to monocyte and endothelial activation. Hypoxia also causes reactive oxygen species (ROS) production that can activate HIF-1, EGR-1, and nuclear factor-κB (NF-κB), which regulates HIF-1 transcription.[5]
HIF-1 and EGR-1 pathways lead to monocyte association with endothelial proteins, such as P-selectin, prompting monocytes to release tissue factor filled microvesicles, which presumably initiate fibrin deposition (via thrombin) after binding the endothelial surface.[5]
Prevention
Evidence supports the use of heparin in people following surgery who have a high risk of thrombosis to reduce the risk of DVTs; however, the effect on PEs or overall mortality is not known.[21] In hospitalized non-surgical patients, mortality decreased but not statistically significant.[22][23] It does not appear however to decrease the rate of symptomatic DVTs.[22] Using both heparin and compression stockings appears better than either one alone in reducing the rate of DVT.[24]
In hospitalized people who have had a stroke and not had surgery, mechanical measures (compression stockings) resulted in skin damage and no clinical improvement.[22] Data on the effectiveness of compression stockings among hospitalized non-surgical patients without stroke is scarce.[22]
The American College of Physicians (ACP) gave three strong recommendations with moderate quality evidence on VTE prevention in non-surgical patients: that hospitalized patients be assessed for their risk of thromboembolism and bleeding before prophylaxis (prevention); that heparin or a related drug is used if potential benefits are thought to outweigh potential harms; and that graduated compression stockings not be used.[25] As an ACP policy implication, the guideline stated a lack of support for any performance measures that incentivize physicians to apply universal prophylaxis without regard to the risks.[25] Goldhaber recommends that people should be assessed at their hospital discharge for persistent high-risk of venous thrombosis, and that people who adopt a heart-healthy lifestyle might lower their risk of venous thrombosis.[26]
In those with cancer who are still walking about yet receiving chemotherapy LMWH decreases the risk of VTE.[27] Due to concerns of bleeding its routine use is not recommended.[27] In adults who have had their low leg casted or placed in a brace for more than a week, LMWH decreased VTE risk.[28] Following the completion of warfarin in those with prior VTE, long term aspirin is beneficial.[29]
Treatment
Evidence-based clinical guidelines from the American College of Chest Physicians were published in February 2012 for the treatment of VTE.[30] Medications used to treat this condition include anticoagulants such as heparin, fondaparinux and more recently dabigatran has shown promise.[31] Vitamin K antagonists such as warfarin are also commonly used.
See also
References
- ↑ National Clinical Guideline Centre – Acute and Chronic Conditions (UK) (2010). "Venous Thromboembolism: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital.". PMID 23346611.
- ↑ Saha P, Humphries J, Modarai B, et al. (2011). "Leukocytes and the natural history of deep vein thrombosis: Current concepts and future directions". Arterioscler Thromb Vasc Biol. 31 (3): 506–12. doi:10.1161/ATVBAHA.110.213405. PMC 3079895
 . PMID 21325673.
. PMID 21325673. - ↑ Di Nisio, Marcello; Middeldorp (February 19, 2014). "Treatment of Lower Extremity Superficial Thrombophlebitis". JAMA. 311 (7): 729–30. doi:10.1001/jama.2014.520. PMID 24549553. Retrieved 24 February 2014.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Martinelli I, Bucciarelli P, Mannucci PM (2010). "Thrombotic risk factors: basic pathophysiology". Crit Care Med. 38 (suppl 2): S3–9. doi:10.1097/CCM.0b013e3181c9cbd9. PMID 20083911.
- 1 2 3 4 5 6 7 Bovill EG, van der Vliet A (2011). "Venous valvular stasis-associated hypoxia and thrombosis: what is the link?". Annu Rev Physiol. 73: 527–45. doi:10.1146/annurev-physiol-012110-142305. PMID 21034220.
- 1 2 3 4 5 6 7 8 9 Rosendaal FR, Reitsma PH (2009). "Genetics of venous thrombosis". J. Thromb. Haemost. 7 (suppl 1): 301–4. doi:10.1111/j.1538-7836.2009.03394.x. PMID 19630821.
- ↑ Stein PD, Beemath A, Meyers FA, et al. (2006). "Incidence of venous thromboembolism in patients hospitalized with cancer". Am J Med. 119 (1): 60–8. doi:10.1016/j.amjmed.2005.06.058. PMID 16431186.
- ↑ Jackson E, Curtis KM, Gaffield ME (2011). "Risk of venous thromboembolism during the postpartum period: a systematic review". Obstet Gynecol. 117 (3): 691–703. doi:10.1097/AOG.0b013e31820ce2db. PMID 21343773.
- ↑ Varga EA, Kujovich JL (2012). "Management of inherited thrombophilia: guide for genetics professionals". Clin Genet. 81 (1): 7–17. doi:10.1111/j.1399-0004.2011.01746.x. PMID 21707594.
- ↑ Turpie AGG (March 2008). "Deep Venous Thrombosis". The Merck's Manuals Online Medical Library. Merck.
- ↑ Reitsma PH, Versteeg HH, Middeldorp S (2012). "Mechanistic view of risk factors for venous thromboembolism". Arterioscler Thromb Vasc Biol. 32 (3): 563–8. doi:10.1161/ATVBAHA.111.242818. PMID 22345594.
- ↑ Zöller B, Li X, Sundquist J, et al. (2012). "Risk of pulmonary embolism in patients with autoimmune disorders: a nationwide follow-up study from Sweden". Lancet. 379 (9812): 244–9. doi:10.1016/S0140-6736(11)61306-8. PMID 22119579.
- 1 2 3 4 5 6 Lijfering WM, Rosendaal FR, Cannegieter SC (2010). "Risk factors for venous thrombosis – current understanding from an epidemiological point of view". Br J Haematol. 149 (6): 824–33. doi:10.1111/j.1365-2141.2010.08206.x. PMID 20456358.
- ↑ Tang, Liang; Wu, Ying-Ying; Lip, Gregory Y H; Yin, Ping; Hu, Yu (December 2015). "Heart failure and risk of venous thromboembolism: a systematic review and meta-analysis". The Lancet Haematology. doi:10.1016/S2352-3026(15)00228-8.
- ↑ Dentali F, Sironi AP, Ageno W, et al. (2012). "Non-O Blood Type Is the Commonest Genetic Risk Factor for VTE: Results from a Meta-Analysis of the Literature". Semin. Thromb. Hemost. 38 (5): 535–48. doi:10.1055/s-0032-1315758. PMID 22740183.
- ↑ Jenkins PV, Rawley O, Smith OP, et al. (2012). "Elevated factor VIII levels and risk of venous thrombosis". Br J Haematol. 157 (6): 653–63. doi:10.1111/j.1365-2141.2012.09134.x. PMID 22530883.
- ↑ Rosendaal FR (2005). "Venous thrombosis: the role of genes, environment, and behavior". Hematology Am. Soc. Hematol. Educ. Program. 2005 (1): 1–12. doi:10.1182/asheducation-2005.1.1. PMID 16304352.
- 1 2 3 Eichinger, S.; Evers, J. L. H.; Glasier, A.; La Vecchia, C.; Martinelli, I.; Skouby, S.; Somigliana, E.; Baird, D. T.; Benagiano, G.; Crosignani, P. G.; Gianaroli, L.; Negri, E.; Volpe, A.; Glasier, A.; Crosignani, P. G. (2013). "Venous thromboembolism in women: A specific reproductive health risk". Human Reproduction Update. 19 (5): 471–482. doi:10.1093/humupd/dmt028. PMID 23825156.
- ↑ Eikelboom, J. W.; Weitz, J. I. (2011). "Importance of family history as a risk factor for venous thromboembolism". Circulation. 124 (9): 996–7. doi:10.1161/CIRCULATIONAHA.111.048868. PMID 21875920.
- 1 2 3 4 López JA, Chen J (2009). "Pathophysiology of venous thrombosis". Thromb Res. 123 (Suppl 4): S30–4. doi:10.1016/S0049-3848(09)70140-9. PMID 19303501.
- ↑ Roderick, P; Ferris, G; Wilson, K; Halls, H; Jackson, D; Collins, R; Baigent, C (December 2005). "Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis". Health technology assessment (Winchester, England). 9 (49): iii–iv, ix–x, 1–78. PMID 16336844.
- 1 2 3 4 Lederle, FA; Zylla, D; Macdonald, R; Wilt, TJ (2011-11-01). "Venous thromboembolism prophylaxis in hospitalized medical patients and those with stroke: a background review for an american college of physicians clinical practice guideline". Annals of Internal Medicine. 155 (9): 602–15. doi:10.1059/0003-4819-155-9-201111010-00008. PMID 22041949.
- ↑ Alikhan, R; Cohen, AT (2009-07-08). Alikhan, Raza, ed. "Heparin for the prevention of venous thromboembolism in general medical patients (excluding stroke and myocardial infarction)". Cochrane database of systematic reviews (Online) (3): CD003747. doi:10.1002/14651858.CD003747.pub2. PMID 19588346.
- ↑ Zareba, P; Wu, C; Agzarian, J; Rodriguez, D; Kearon, C (Aug 2014). "Meta-analysis of randomized trials comparing combined compression and anticoagulation with either modality alone for prevention of venous thromboembolism after surgery.". The British journal of surgery. 101 (9): 1053–62. doi:10.1002/bjs.9527. PMID 24916118.
- 1 2 Qaseem A, Chou R, Humphrey LL, Starkey M, Shekelle P, Clinical Guidelines Committee of the American College of Physicians (2011). "Venous thromboembolism prophylaxis in hospitalized patients: a clinical practice guideline from the American College of Physicians". Ann Intern Med. 155 (9): 625–32. doi:10.7326/0003-4819-155-9-201111010-00011. PMID 22041951.
- ↑ Goldhaber, Samuel Z. (2010). "Risk Factors for Venous Thromboembolism". Journal of the American College of Cardiology. 56 (1): 1–7. doi:10.1016/j.jacc.2010.01.057. PMID 20620709.
- 1 2 Di Nisio, M; Porreca, E; Otten, HM; Rutjes, AW (Aug 29, 2014). "Primary prophylaxis for venous thromboembolism in ambulatory cancer patients receiving chemotherapy.". The Cochrane database of systematic reviews. 8: CD008500. doi:10.1002/14651858.CD008500.pub3. PMID 25171736.
- ↑ Testroote, M; Stigter, WA; Janssen, L; Janzing, HM (Apr 25, 2014). "Low molecular weight heparin for prevention of venous thromboembolism in patients with lower-leg immobilization.". The Cochrane database of systematic reviews. 4: CD006681. doi:10.1002/14651858.CD006681.pub3. PMID 24771319.
- ↑ Simes, J; Becattini, C; Agnelli, G; Eikelboom, JW; Kirby, AC; Mister, R; Prandoni, P; Brighton, TA; INSPIRE Study Investigators (International Collaboration of Aspirin Trials for Recurrent Venous, Thromboembolism) (23 September 2014). "Aspirin for the prevention of recurrent venous thromboembolism: the INSPIRE collaboration.". Circulation. 130 (13): 1062–71. doi:10.1161/circulationaha.114.008828. PMID 25156992.
- ↑ Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ, and for the American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel (February 2012). "Executive Summary: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines". Chest. 141 (2 suppl): 7S–47S. doi:10.1378/chest.1412S3. PMC 3278060
 . PMID 22315257.
. PMID 22315257. - ↑ Schulman S, Kearon C, Kakkar AK; et al. (2009). "Dabigatran versus warfarin in the treatment of acute venous thromboembolism". N Engl J Med. 361 (24): 2342–52. doi:10.1056/NEJMoa0906598. PMID 19966341.