Venous ulcer
| Venous ulcer | |
|---|---|
 | |
| Venous ulcer on the back of the right leg. | |
| Classification and external resources | |
| Specialty | dermatology |
| ICD-10 | I83.0, I83.2, L97 |
| ICD-9-CM | 454.0 |
| DiseasesDB | 29114 |
| MedlinePlus | 000834 |
| MeSH | D014647 |
Venous ulcers (venous insufficiency ulceration, stasis ulcers, stasis dermatitis, varicose ulcers, or ulcus cruris) are wounds that are thought to occur due to improper functioning of venous valves, usually of the legs (hence leg ulcers).[1]:846 They are the major occurrence of chronic wounds, occurring in 70% to 90% of leg ulcer cases.[2] Venous ulcers develop mostly along the medial distal leg, and can be very painful.
Signs and symptoms
Edema and fibrinous exudate leads to fibrosis of subcutaneous tissues with localized pigment loss and dilation of capillary loops. This is called atrophic blanche. This can occur around ankles and gives an appearance of inverted champagne bottle to legs. Large ulcers may encircle the leg. Lymphedema results from obliteration of superficial lymphatics. There is hypertrophy of overlying epidermis giving polypoid appearance, known as lipodermatosclerosis.
- Venous ulcer before surgery
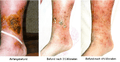 Healing process of a chronic venous stasis ulcer of the lower leg
Healing process of a chronic venous stasis ulcer of the lower leg Healing venous ulcer after one month
Healing venous ulcer after one month
Pathophysiology
The exact cause of venous ulcers is not certain, but they are thought to arise when venous valves that exist to prevent backflow of blood do not function properly, causing the pressure in veins to increase.[3][4][5][6] The body needs the pressure gradient between arteries and veins in order for the heart to pump blood forward through arteries and into veins. When venous hypertension exists, arteries no longer have significantly higher pressure than veins, and blood is not pumped as effectively into or out of the area.[3][4][5][6]
Venous hypertension may also stretch veins and allow blood proteins to leak into the extravascular space, isolating extracellular matrix (ECM) molecules and growth factors, preventing them from helping to heal the wound.[3][6] Leakage of fibrinogen from veins as well as deficiencies in fibrinolysis may also cause fibrin to build up around the vessels, preventing oxygen and nutrients from reaching cells.[3] Venous insufficiency may also cause white blood cells (leukocytes) to accumulate in small blood vessels, releasing inflammatory factors and reactive oxygen species (ROS, free radicals) and further contributing to chronic wound formation.[3][6] Buildup of white blood cells in small blood vessels may also plug the vessels, further contributing to ischemia.[7] This blockage of blood vessels by leukocytes may be responsible for the "no reflow phenomenon," in which ischemic tissue is never fully reperfused.[7] Allowing blood to flow back into the limb, for example by elevating it, is necessary but also contributes to reperfusion injury.[4] Other comorbidities may also be the root cause of venous ulcers.[5]
It is in the crus that the classic venous stasis ulcer occurs. Venous stasis results from damage to the vein valvular system in the lower extremity and in extreme cases allows the pressure in the veins to be higher than the pressure in the arteries. This pressure results in transudation of inflammatory mediators into the subcutaneous tissues of the lower extremity and subsequent breakdown of the tissue including the skin.
Wounds of the distal lower extremities arising from causes not directly related to venous insufficiency (e.g., scratch, bite, burn, or surgical incision) may ultimately fail to heal if underlying (often undiagnosed) venous disease is not properly addressed.
Diagnosis
Classification
A clinical severity score has been developed to assess chronic venous ulcers. It is based on the CEAP (clinical, etiology, anatomy, and pathophysiology) classification system developed by an expert panel. A high score gives a poor prognosis.[8]
Distinction from arterial ulcer
A venous ulcer tends to occur on the medial side of the leg, typically around the medial malleolus in the 'gaiter area' whereas arterial ulcer tends to occur on lateral side of the leg and over bony prominences. A venous ulcer is typically shallow with irregular sloping edges whereas an arterial ulcer can be deep and has a 'punched out' appearance. Venous ulcers are typically 'wet' with a moderate to heavy exudate whereas. Arterial ulcers are typically 'dry' and scabbed. The skin surrounding a venous ulcer may be oedematous (swollen) and there may be evidence of varicose veins; the skin surrounding an arterial ulcer may be pale, cold, shiny and hairless. Both venous and arterial ulcers may be painful, however arterial ulcers tend to be more painful, especially with elevation of the leg, for example when in bed.
Prevention
Compression stockings appear to prevent the formation of new ulcers in people with a history of venous ulcers.[9]
Treatment
The main aim of the treatment is to create such an environment that allows skin to grow across an ulcer. In the majority of cases this requires finding and treating underlying venous reflux and National Institute for Health and Care Excellence (NICE) recommends referral to a vascular service for anyone with a leg ulcer that has not healed within 2 weeks or anyone with a healed leg ulcer.[10]
Most venous ulcers respond to patient education, elevation of foot, elastic compression and evaluation, called the Bisgaard regimen.[11] There is no evidence for intravenous or by mouth antibiotics for venous leg ulcers.[12] Silver products are also not typically useful while there is some evidence for cadexomer iodine creams.[12] There is a lack of quality evidence regarding the use of medical grade honey for venous leg ulcers.[13]
Compression Therapy
Non-elastic, ambulatory, below knee (BK) compression counters the impact of reflux on venous pump failure. Compression therapy is used for venous leg ulcers and can decrease blood vessel diameter and pressure, which increases their effectiveness, preventing blood from flowing backwards.[3] Compression is also used [3][14] to decrease release of inflammatory cytokines, lower the amount of fluid leaking from capillaries and therefore prevent swelling, and prevent clotting by decreasing activation of thrombin and increasing that of plasmin.[2] Compression is applied using elastic bandages or boots specifically designed for the purpose.[3]
Regarding effectiveness, compression dressings improve healing.[15] It is not clear whether non-elastic systems are better than a multilayer elastic system.[15] Patients should wear as much compression as is comfortable.[16] The type of dressing applied beneath the compression does not seem to matter, and hydrocolloid is not better than simple low adherent dressings.[17][18] Recently there have been clinical studies on a multi-functional botanical-based ointment in combination with compression therapy in the treatment of difficult-to-heal wounds, including venous leg ulcers.[19]
Intermittent pneumatic compression devices may be used, but it is not clear that they are superior to simple compression dressings.[20]
It is not clear if interventions that are aimed to help people adhere to compression therapy are effective.[21] More research is needed in this field.
Medications
Pentoxifylline is a useful add on treatment to compression stockings and may also help by itself.[22] It works by reducing platelet aggregation and thrombus formation. Gastrointestinal disturbances were reported as a potential adverse effect.[22]
Sulodexide, which reduces the formation of blood clots and reduces inflammation, may improve the healing of venous ulcers when taken in conjunction with proper local wound care.[23] Further research is necessary to determine potential adverse effects, the effectiveness, and the dosing protocol for sulodexide treatment.
An oral dose of aspirin is being investigated as a potential treatment option for people with venous ulcers. A 2016 Cochrane systematic review concluded that further research is necessary before this treatment option can be confirmed to be safe and effective.[24]
Oral zinc supplements have not been proven to be effective in aiding the healing of venous ulcers, however more research is necessary to confirm these results.[25]
Skin grafts and artificial skin
Two layers of skin created from animal sources as a skin graft has been found to be useful in venous leg ulcers.[26]
Artificial skin, made of collagen and cultured skin cells, is also used to cover venous ulcers and excrete growth factors to help them heal.[27] A systematic review found that bilayer artificial skin with compression bandaging is useful in the healing of venous ulcers when compared to simple dressings.[26]
Surgery
A randomized controlled trial found that surgery "reduces the recurrence of ulcers at four years and results in a greater proportion of ulcer free time".[28]
Local anaesthetic endovenous surgery using the thermoablation (endovenous laser ablation or radiofrequency), perforator closure (TRLOP) and foam sclerotherapy showed an 85% success rate of healing, with no recurrence of healed ulcers at an average of 3.1 years, and a clinical improvement in 98% in a selected group of venous leg ulcers.[29]
Prognosis
Venous ulcers are costly to treat, and there is a significant chance that they will recur after healing;[2][3] one study found that up to 48% of venous ulcers had recurred by the fifth year after healing.[3] However treatment with local anaesthetic endovenous techniques suggests a reduction of this high recurrence rate is possible.[29]
Without proper care, the ulcer may get infected leading to cellulitis or gangrene and eventually may need amputation of the part of limb in future.
Some topical drugs used to treat venous ulcer may cause venous eczema.[30]
Research
The current ‘best’ practice in the UK is to treat the underlying venous reflux once an ulcer has healed. It is questionable as to whether endovenous treatment should be offered before ulcer healing, as current evidence would not support this approach as standard care. EVRA (Early Venous Reflux Ablation) ulcer trial - A UK NIHR HTA funded randomised clinical trial to compare early versus delayed endovenous treatment of superficial venous reflux in patients with chronic venous ulceration opened for recruitment in October 2013. The study hopes to show an increase in healing rates from 60% to 75% at 24 weeks.[31]
Research from the University of Surrey and funded by the Leg Ulcer Charity is currently looking at the psychological impact of having a leg ulcer, on the relatives and friends of the affected person, and the influence of treatment.[32]
References
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- 1 2 3 Snyder RJ (2005). "Treatment of nonhealing ulcers with allografts". Clin. Dermatol. 23 (4): 388–95. doi:10.1016/j.clindermatol.2004.07.020. PMID 16023934.
- 1 2 3 4 5 6 7 8 9 10 Brem H, Kirsner RS, Falanga V (2004). "Protocol for the successful non-surgical treatment of venous ulcers". Am. J. Surg. 188 (1A Suppl): 1–8. doi:10.1016/S0002-9610(03)00284-8. PMID 15223495.
- 1 2 3 Mustoe T (2004). "Understanding chronic wounds: a unifying hypothesis on their pathogenesis and implications for therapy". Am. J. Surg. 187 (5A): 65S–70S. doi:10.1016/S0002-9610(03)00306-4. PMID 15147994.
- 1 2 3 Moreo K (2005). "Understanding and overcoming the challenges of effective case management for patients with chronic wounds". The Case manager. 16 (2): 62–3, 67. doi:10.1016/j.casemgr.2005.01.014. PMID 15818347.
- 1 2 3 4 Stanley AC, Lounsbury KM, Corrow K, et al. (2005). "Pressure elevation slows the fibroblast response to wound healing". J. Vasc. Surg. 42 (3): 546–51. doi:10.1016/j.jvs.2005.04.047. PMID 16171604.
- 1 2 "eMedicine - Reperfusion Injury in Stroke : Article by Wayne M Clark, MD". Retrieved 2007-08-05.
- ↑ Eklöf B, Rutherford RB, Bergan JJ, et al. (2004). "Revision of the CEAP classification for chronic venous disorders: consensus statement". J. Vasc. Surg. 40 (6): 1248–52. doi:10.1016/j.jvs.2004.09.027. PMID 15622385.
- ↑ Nelson, EA; Bell-Syer, SE (Sep 9, 2014). "Compression for preventing recurrence of venous ulcers.". The Cochrane database of systematic reviews. 9: CD002303. doi:10.1002/14651858.CD002303.pub3. PMID 25203307.
- ↑ NICE (July 23, 2013). "Varicose veins in the legs: The diagnosis and management of varicose veins. 1.2 Referral to a vascular service". National Institute for Health and Care Excellence. Retrieved August 25, 2014.
- ↑ "BMJ responses". Retrieved 3 May 2013.
- 1 2 O'Meara, S; Al-Kurdi, D; Ologun, Y; Ovington, LG; Martyn-St James, M; Richardson, R (10 January 2014). "Antibiotics and antiseptics for venous leg ulcers.". The Cochrane database of systematic reviews. 1: CD003557. doi:10.1002/14651858.CD003557.pub5. PMID 24408354.
- ↑ Jull AB, Cullum N, Dumville JC, Westby MJ, Deshpande S, Walker N (6 March 2015). "Honey as a topical treatment for wounds". Cochrane Database of Systematic Reviews. 3: CD005083. doi:10.1002/14651858.CD005083.pub4. PMID 25742878.
- ↑ Taylor JE, Laity PR, Hicks J, et al. (2005). "Extent of iron pick-up in deforoxamine-coupled polyurethane materials for therapy of chronic wounds". Biomaterials. 26 (30): 6024–33. doi:10.1016/j.biomaterials.2005.03.015. PMID 15885771.
- 1 2 Nelson EA, Cullum N, Jones J (2006). "Venous leg ulcers.". Clin Evid (15): 2607–26. PMID 16973096.
- ↑ Nelson EA, Harper DR, Prescott RJ, Gibson B, Brown D, Ruckley CV (2006). "Prevention of recurrence of venous ulceration: randomized controlled trial of class 2 and class 3 elastic compression". J. Vasc. Surg. 44 (4): 803–8. doi:10.1016/j.jvs.2006.05.051. PMID 17012004.
- ↑ Palfreyman SJ, Nelson EA, Lochiel R, Michaels JA (2006). Palfreyman, Simon SJ, ed. "Dressings for healing venous leg ulcers". Cochrane database of systematic reviews (Online). 3: CD001103. doi:10.1002/14651858.CD001103.pub2. PMID 16855958.
- ↑ Palfreyman S, Nelson EA, Michaels JA (2007). "Dressings for venous leg ulcers: systematic review and meta-analysis". BMJ. 335 (7613): 244. doi:10.1136/bmj.39248.634977.AE. PMC 1939774
 . PMID 17631512.
. PMID 17631512. - ↑ Reyzelman, Alexander; Bazarov, Irina (Dec 2012). "Initial clinical assessment of a novel multifunctional topical ointment for difficult-to-heal wounds: a case series.". Advances in Skin and Wound Care. 25 (12): 557–560. doi:10.1097/01.ASW.0000423441.00908.05. PMID 23151766.
- ↑ Nelson EA, Hillman A, Thomas K (2014). "Intermittent pneumatic compression for treating venous leg ulcers.". Cochrane Database Syst Rev. 5: CD001899. doi:10.1002/14651858.CD001899.pub4. PMID 24820100.
- ↑ Weller, Carolina D.; Buchbinder, Rachelle; Johnston, Renea V. (2016-03-02). "Interventions for helping people adhere to compression treatments for venous leg ulceration". The Cochrane Database of Systematic Reviews. 3: CD008378. doi:10.1002/14651858.CD008378.pub3. ISSN 1469-493X. PMID 26932818.
- 1 2 Jull, Andrew B.; Arroll, Bruce; Parag, Varsha; Waters, Jill (2012-12-12). "Pentoxifylline for treating venous leg ulcers". The Cochrane Database of Systematic Reviews. 12: CD001733. doi:10.1002/14651858.CD001733.pub3. ISSN 1469-493X. PMID 23235582.
- ↑ Wu, Bin; Lu, Jing; Yang, Ming; Xu, Ting (2016-06-02). "Sulodexide for treating venous leg ulcers". The Cochrane Database of Systematic Reviews (6): CD010694. doi:10.1002/14651858.CD010694.pub2. ISSN 1469-493X. PMID 27251175.
- ↑ de Oliveira Carvalho, Paulo Eduardo; Magolbo, Natiara G.; De Aquino, Rebeca F.; Weller, Carolina D. (2016-02-18). "Oral aspirin for treating venous leg ulcers". The Cochrane Database of Systematic Reviews. 2: CD009432. doi:10.1002/14651858.CD009432.pub2. ISSN 1469-493X. PMID 26889740.
- ↑ Wilkinson, Ewan A. J. (2014-09-09). "Oral zinc for arterial and venous leg ulcers". The Cochrane Database of Systematic Reviews (9): CD001273. doi:10.1002/14651858.CD001273.pub3. ISSN 1469-493X. PMID 25202988.
- 1 2 Jones, JE; Nelson, EA; Al-Hity, A (Jan 31, 2013). "Skin grafting for venous leg ulcers.". The Cochrane database of systematic reviews. 1: CD001737. doi:10.1002/14651858.CD001737.pub4. PMID 23440784.
- ↑ Mustoe T (March 17–18, 2005). Dermal ulcer healing: Advances in understanding. Tissue repair and ulcer/wound healing: molecular mechanisms, therapeutic targets and future directions. Paris, France.
- ↑ Gohel MS, Barwell JR, Taylor M, et al. (July 2007). "Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): randomised controlled trial". BMJ. 335 (7610): 83. doi:10.1136/bmj.39216.542442.BE. PMC 1914523
 . PMID 17545185.
. PMID 17545185. - 1 2 Thomas CA, Holdstock JM, Harrison CC, Price BA, Whiteley MS (April 2013). "Healing rates following venous surgery for chronic venous leg ulcers in an independent specialist vein unit". Phlebology. 28 (3): 132–9. doi:10.1258/phleb.2012.011097. PMID 22833505.
- ↑ Roxburgh's Common Skin Diseases (17th ed.). p. 127. ISBN 978-0-340-76232-5.
- ↑ http://www1.imperial.ac.uk/biosurgerysurgicaltechnology/clinical_trials_outcomes/vasculardisease/clinicaltrials/evra/[]
- ↑ Pippa Tollow (April 2014). "Impact of Leg Ulcers on Relatives and Carers of Affected Patients - A PhD Study funded by The Leg Ulcer Charity". The Leg Ulcer Charity. Retrieved August 25, 2014.