Alcohol tolerance

Alcohol tolerance refers to the bodily responses to the functional effects of ethanol in alcoholic beverages. This includes direct tolerance, speed of recovery from insobriety and resistance to the development of alcoholism.
Consumption-induced tolerance
Alcohol tolerance is increased by regular drinking.[1] This reduced sensitivity requires that higher quantities of alcohol be consumed in order to achieve the same effects as before tolerance was established. Alcohol tolerance may lead to (or be a sign of) alcohol dependency.[1]
Heavy alcohol consumption over a period of years can lead to "reverse tolerance". A liver can be damaged by chronic alcohol use, leading to a buildup of fat and scar tissue. The reduced ability of such a liver to metabolize or break down alcohol means that small amounts can lead to a high blood alcohol concentration (BAC) and more rapid intoxication.
Physiology of alcohol tolerance
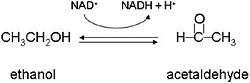
Direct alcohol tolerance is largely dependent on body size. Large-bodied people will require more alcohol to reach insobriety than lightly built people. Thus men, being larger than women on average, will have a higher alcohol tolerance. The alcohol tolerance is also connected with activity of alcohol dehydrogenases (a group of enzymes responsible for the breakdown of alcohol) in the liver, and in the bloodstream.
High level of alcohol dehydrogenase activity results in fast transformation of ethanol to more toxic acetaldehyde. Such atypical alcohol dehydrogenase levels are less frequent in alcoholics than in nonalcoholics and, alongside other symptoms, can indicate various forms of liver disease. Furthermore, among alcoholics, the carriers of this atypical enzyme consume lower ethanol doses, compared to the individuals without the allele.
Alcohol tolerance in different ethnic groups
The tolerance to alcohol is not equally distributed throughout the world's population, and genetics of alcohol dehydrogenase indicate resistance has arisen independently in different cultures.[2] In North America, Native Americans have the highest probability of developing alcoholism compared to Europeans and Asians.[3][4][5][6]
Higher body masses and the prevalence of high levels of alcohol dehydrogenase in an individual increase alcohol tolerance.[7][8]
Not all differences in tolerance can be traced to biochemistry.[9] Differences in tolerance levels are also influenced by socio-economic and cultural difference including diet, average body weight and patterns of consumption.[10][11]
An estimated one out of twenty people have an alcohol flush reaction. It is not in any way an indicator for the drunkenness of an individual.[12][13] It is colloquially known as "face flush", a condition where the body metabolizes alcohol nearly 100-times more efficiently into acetaldehyde, a toxic metabolite.[14][15] Flushing, or blushing, is associated with the erythema (reddening caused by dilation of capillaries) of the face, neck, and shoulder, after consumption of alcohol.[16]
Footnotes
- 1 2 "Alcohol and Tolerance". National Institute on Alcohol Abuse and Alcoholism (NIAAA), Alcohol Alert (28). April 1995. Retrieved 2009-08-13.
- ↑ Osier, Michael V.; Pakstis, Andrew J.; Soodyall, Himla; Comas, David; Goldman, David; Odunsi, Adekunle; Okonofua, Friday; Parnas, Josef; et al. (2002). "A Global Perspective on Genetic Variation at the ADH Genes Reveals Unusual Patterns of Linkage Disequilibrium and Diversity". American Journal of Human Genetics. 71 (1): 84–99. doi:10.1086/341290. PMC 384995
 . PMID 12050823.
. PMID 12050823. - ↑ "Alcohol Use Disorder". NY Times. 2013. Retrieved July 21, 2016.
- ↑ Mail & al. (eds., 2002): Alcohol Use Among American Indians and Alaska Natives: Multiple Perspectives on a Complex Problem. NIAAA Research Monograph No. 37. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism
- ↑ Caetano, Raul; Clark, Catherine L (1998). "Trends in Alcohol-Related Problems among Whites, Blacks, and Hispanics: 1984-1995". Alcoholism: Clinical and Experimental Research. 22 (2): 534. doi:10.1111/j.1530-0277.1998.tb03685.x.
- ↑ Karen Chartier; Raul Caetano. "Ethnicity and Health Disparities in Alcohol Research".
- ↑ Yin, S. -J.; Cheng, T. -C.; Chang, C. -P.; Chen, Y. -J.; Chao, Y. -C.; Tang, H. -S.; Chang, T. -M.; Wu, C. -W. (1988). "Human stomach alcohol and aldehyde dehydrogenases (ALDH): A genetic model proposed for ALDH III isozymes". Biochemical Genetics. 26 (5–6): 343–60. doi:10.1007/BF00554070. PMID 3214414.
- ↑ Fenna, D; Schaefer, O; Mix, L; Gilbert, JA (1971). "Ethanol metabolism in various racial groups". Canadian Medical Association journal. 105 (5): 472–5. PMC 1931291
 . PMID 5112118.
. PMID 5112118. - ↑ Bennion L.; Li T. K. (1976). "Alcohol metabolism in American Indians and whites". New England Journal of Medicine. 294 (1): 9–13. doi:10.1056/nejm197601012940103. PMID 1244489.
- ↑ Waldram, J. B.; Herring, A. & Young, K. (1995). Aboriginal Health in Canada: Historical, Cultural, and Epidemiological Perspectives. Toronto: University of Toronto Press.
- ↑ Saggers, S. & Gray, D. (1998b). Dealing with Alcohol: Indigenous Usage in Australia, New Zealand and Canada. Cambridge: Cambridge University Press
- ↑ "Myth or reality? The Asian alcohol 'gene' explained". Difford's Guide. September 10, 2013.
- ↑ "Identifying the Signs of Intoxication" (PDF). Government of Western Australia. December 2010. Archived from the original (PDF) on March 27, 2011.
- ↑ Eng, MY; Luczak, SE; Wall, TL (2007). "ALDH2, ADH1B, and ADH1C genotypes: A literature review". Alcohol Research & Health. 30 (1): 22–7. PMID 17718397.
- ↑ Peng, Yi; Shi, Hong; Qi, Xue-bin; Xiao, Chun-jie; Zhong, Hua; Ma, Run-lin Z; Su, Bing (2010). "The ADH1B Arg47His polymorphism in farming populations and expansion of rice domestication in history". BMC Evolutionary Biology. 10: 15. doi:10.1186/1471-2148-10-15. PMC 2823730
 . PMID 20089146. Lay summary – ScienceNow (January 20, 2010).
. PMID 20089146. Lay summary – ScienceNow (January 20, 2010). - ↑ Ohta, Shigeo; Ohsawa, Ikuroh; Kamino, Kouzin; Ando, Fujiko; Shimokata, Hiroshi (2004). "Mitochondrial ALDH2 Deficiency as an Oxidative Stress". Annals of the New York Academy of Sciences. 1011: 36–44. doi:10.1196/annals.1293.004. PMID 15126281.
References
- Carroll, Charles R. Drugs in Modern Society . NY: McGraw-Hill, 2000 (fifth ed.).
- Chesher, G.; Greeley, J. (1992). "Tolerance to the effects of alcohol". Alcohol, Drugs and Driving. 8 (2): 93–106.
- Osier, M; Pakstis, AJ; Kidd, JR; Lee, JF; Yin, SJ; Ko, HC; Edenberg, HJ; Lu, RB; Kidd, KK (1999). "Linkage disequilibrium at the ADH2 and ADH3 loci and risk of alcoholism". American Journal of Human Genetics. 64 (4): 1147–57. doi:10.1086/302317. PMC 1377839
 . PMID 10090900.
. PMID 10090900. - Muramatsu, T; Wang, ZC; Fang, YR; Hu, KB; Yan, H; Yamada, K; Higuchi, S; Harada, S; Kono, H (1995). "Alcohol and aldehyde dehydrogenase genotypes and drinking behavior of Chinese living in Shanghai". Human Genetics. 96 (2): 151–4. doi:10.1007/BF00207371. PMID 7635462.
- Neumark, YD; Friedlander, Y; Thomasson, HR; Li, TK (1998). "Association of the ADH2*2 allele with reduced ethanol consumption in Jewish men in Israel: A pilot study". Journal of studies on alcohol. 59 (2): 133–9. PMID 9500299.
- Borinskaya, S. A.; Gasemianrodsari, F.; Kalyina, N. R.; Sokolova, M. V.; Yankovsky, N. K. (2005). "Polymorphism of Alcohol Dehydrogenase Gene ADH1B in Eastern Slavic and Iranian-Speaking Populations". Russian Journal of Genetics. 41 (11): 1291–4. doi:10.1007/s11177-005-0231-5. Translated from "Polymorphism of alcohol dehydrogenase gene ADH1B in eastern Slavic and Iranian-speaking populations". Genetika. 41 (11): 1563–6. 2005. PMID 16358724.
- Borinskaya, Svetlana; Kal'Ina, Nina; Marusin, Andrey; Faskhutdinova, Gulnaz; Morozova, Irina; Kutuev, Ildus; Koshechkin, Vladimir; Khusnutdinova, Elza; et al. (2009). "Distribution of the Alcohol Dehydrogenase ADH1B∗47His Allele in Eurasia". American Journal of Human Genetics. 84 (1): 89–92; author reply 92–4. doi:10.1016/j.ajhg.2008.12.007. PMC 2668054
 . PMID 19124091.
. PMID 19124091. - Li, Hui; Borinskaya, Svetlana; Yoshimura, Kimio; Kal’Ina, Nina; Marusin, Andrey; Stepanov, Vadim A.; Qin, Zhendong; Khaliq, Shagufta; et al. (2009). "Refined Geographic Distribution of the Oriental ALDH2*504Lys (nee 487Lys) Variant". Annals of Human Genetics. 73 (3): 335–45. doi:10.1111/j.1469-1809.2009.00517.x. PMC 2846302
 . PMID 19456322.
. PMID 19456322.
Further reading
- Caetano R, Clark CL, Tam T (1998). "Alcohol consumption among racial/ethnic minorities: theory and research" (PDF). Alcohol Health Res World. 22 (4): 233–41. PMID 15706749. Archived from the original (PDF) on June 16, 2015.