Blunt trauma
| Blunt trauma | |
|---|---|
 | |
| Classification and external resources |
Blunt trauma, blunt injury, non-penetrating trauma or blunt force trauma refers to physical trauma to a body part, either by impact, injury or physical attack. The latter is usually referred to as blunt force trauma. The term refers to the initial trauma, from which develops more specific types such as contusions, abrasions, lacerations, and/or bone fractures. Blunt trauma is contrasted with penetrating trauma, in which an object such as a bullet enters the body.
Variations
Blunt abdominal trauma
Blunt abdominal trauma (BAT) comprises 75% of all blunt trauma and is the most common example of this injury.[1] The majority occurs in motor vehicle accidents, in which rapid deceleration may propel the driver into the steering wheel, dashboard, or seatbelt[2] causing contusions in less serious cases, or rupture of internal organs from briefly increased intraluminal pressure in the more serious, dependent on the force applied.
There are two basic physical mechanisms at play with the potential of injury to intra-abdominal organs — compression and deceleration.[3] The former occurs from a direct blow, such as a punch, or compression against a non-yielding object such as a seat belt or steering column. This force may deform a hollow organ thereby increasing its intra-luminal or internal pressure, leading to rupture. Deceleration, on the other hand, causes stretching and shearing at the points at which mobile structures, such as the bowel, are anchored. This can cause tearing of the mesentery of the bowel, and injury to the blood vessels that travel within the mesentery. Classic examples of these mechanisms are a hepatic tear along the ligamentum teres and injuries to the renal arteries.
When blunt abdominal trauma is complicated by 'internal injury', the liver and spleen (see blunt splenic trauma) are most frequently involved, followed by the small intestine.
In rare cases, this injury has been attributed to medical techniques such as the Heimlich Maneuver,[4] attempts at cardiopulmonary resuscitation, and manual thrusts to clear an airway. Although these are rare examples, it has been suggested that they are caused by applying unnecessary pressure when administering such techniques. Finally, the occurrence of splenic rupture with mild blunt abdominal trama in those convalescing from infectious mononucleosis is well reported.[5]
Diagnosis
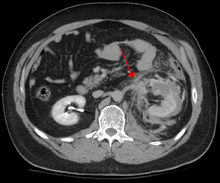
In all but the most obviously trivial injuries, the first concern is to exclude anything that might be quickly or immediately life-threatening. This is resolved by ascertaining that the subject's airway is open and competent, that breathing is unlabored, and that circulation — i.e. pulses that can be felt, is present. This is sometimes described as the "A, B, C's" — Airway, Breathing, and Circulation – and is the first step in any resuscitation or triage. Then, the history of the accident or injury is amplified with any medical, dietary (timing of last oral intake) and past history, from whatever sources such as family, friends, previous treating physicians that might be available. This method is sometimes given the mnemonic "SAMPLE". The amount of time spent on diagnosis should be minimized and expedited by a combination of clinical assessment and appropriate use of technology,[6] such as diagnostic peritoneal lavage (DPL), or bedside ultrasound examination (FAST)[7] before proceeding to laparotomy if required. If time and the patient's stability permits, CT examination may be carried out if available.[8] Its advantages include superior definition of the injury, leading to grading of the injury and sometimes the confidence to avoid or postpone surgery. Its disadvantages include the time taken to acquire images, although this gets shorter with each generation of scanners, and the removal of the patient from the immediate view of the emergency or surgical staff.
Recently, criteria have been defined that might allow patients with blunt abdominal trauma to be discharged safely without further evaluation. The characteristics of such patients would include:
- absence of intoxication
- no evidence of lowered blood pressure or raised pulse rate
- no abdominal pain or tenderness
- no blood in the urine.
To be considered low risk, patients would need to meet all low-risk criteria.[9]
Blunt abdominal trauma in sports
The majority of contact-collision injuries, usually blunt trauma, should have been witnessed in high school or collegiate games where the athletic training staff are trained to keep their eyes on the play. This may allow some departure from Advanced Trauma Life Support guidelines in the initial assessment, although the principles always apply. The major priority then becomes separating contusions and musculo-tendinous injuries from injuries to solid organs and the gut and recognizing potential or developing blood loss, and reacting accordingly. Blunt injuries to the kidney from helmets, shoulder pads, and knees are also described in football,[10] and in soccer, martial arts, and all-terrain vehicle accidents.
Treatment
In every case where the presumption of internal injury has been sufficient to trigger the diagnostic steps outlined above, intravenous access will be established and crystalloid solutions and/or blood will be administered at rates sufficient to maintain the circulation. Thereafter, further treatment will depend on the grade of organ damage estimated by the prior investigations and will vary from close observation with the ability to intervene quickly, or surgery, open or laparoscopic.[11] In the case of blunt adbominal trauma, there is no shown benefit from surgery unless active bleeding is present.[12]
See also
References
- ↑ Isenhour JL, Marx J (August 2007). "Advances in abdominal trauma". Emerg Med Clin North Am. 25 (3): 713–33, ix. doi:10.1016/j.emc.2007.06.002. PMID 17826214.
- ↑ Bansal V, Conroy C, Tominaga GT, Coimbra R (December 2009). "The utility of seat belt signs to predict intra-abdominal injury following motor vehicle crashes". Traffic Inj Prev. 10 (6): 567–72. doi:10.1080/15389580903191450. PMID 19916127.
- ↑ Mukhopadhyay M (October 2009). "Intestinal Injury from Blunt Abdominal Trauma: A Study of 47 Cases". Oman Med J. 24 (4): 256–259. doi:10.5001/omj.2009.52. PMC 3243872
 . PMID 22216378.
. PMID 22216378. - ↑ Mack L, Forbes TL, Harris KA (January 2002). "Acute aortic thrombosis following incorrect application of the Heimlich maneuver". Ann Vasc Surg. 16 (1): 130–3. doi:10.1007/s10016-001-0147-z. PMID 11904818.
- ↑ O'Connor TE, Skinner LJ, Kiely P, Fenton JE (August 2011). "Return to contact sports following infectious mononucleosis: the role of serial ultrasonography". Ear Nose Throat J. 90 (8): E21–4. PMID 21853428.
- ↑ Woods SD (February 1995). "Assessment of blunt abdominal trauma". Aust N Z J Surg. 65 (2): 75–6. doi:10.1111/j.1445-2197.1995.tb07263.x. PMID 7857232.
- ↑ Marco GG, Diego S, Giulio A, Luca S (October 2005). "Screening US and CT for blunt abdominal trauma: a retrospective study". Eur J Radiol. 56 (1): 97–101. doi:10.1016/j.ejrad.2005.02.001. PMID 16168270.
- ↑ Jansen JO, Yule SR, Loudon MA (April 2008). "Investigation of blunt abdominal trauma". BMJ. 336 (7650): 938–42. doi:10.1136/bmj.39534.686192.80. PMC 2335258
 . PMID 18436949.
. PMID 18436949. - ↑ Kendall JL, Kestler AM, Whitaker KT, Adkisson MM, Haukoos JS (November 2011). "Blunt abdominal trauma patients are at very low risk for intra-abdominal injury after emergency department observation". West J Emerg Med. 12 (4): 496–504. doi:10.5811/westjem.2010.11.2016. PMC 3236146
 . PMID 22224146.
. PMID 22224146. - ↑ Brophy RH, Gamradt SC, Barnes RP, et al. (January 2008). "Kidney injuries in professional American football: implications for management of an athlete with 1 functioning kidney". Am J Sports Med. 36 (1): 85–90. doi:10.1177/0363546507308940. PMID 17986635.
- ↑ D'Errico E, Goffre B, Mazza D (2009). "Blunt abdominal trauma: current management". Chir Ital. 61 (5-6): 601–6. PMID 20380265.
- ↑ Oyo-Ita, Angela; Ugare, Udey G.; Ikpeme, Ikpeme A. (November 14, 2012). "Surgical versus non-surgical management of abdominal injury". The Cochrane Database of Systematic Reviews. 11: CD007383. doi:10.1002/14651858.CD007383.pub2. ISSN 1469-493X. PMID 23152244.