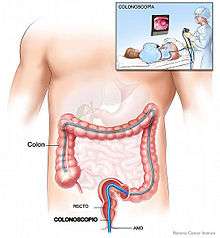
Colonoscopy
| Colonoscopy | |
|---|---|
| Intervention | |
 Colonoscopy being performed | |
| ICD-9-CM | 45.23 |
| MeSH | D003113 |
| OPS-301 code | 1-650 |
| MedlinePlus | 003886 |
Colonoscopy or coloscopy[1] is the endoscopic examination of the large bowel and the distal part of the small bowel with a CCD camera or a fiber optic camera on a flexible tube passed through the anus. It can provide a visual diagnosis (e.g. ulceration, polyps) and grants the opportunity for biopsy or removal of suspected colorectal cancer lesions. Colonoscopy can remove polyps as small as one millimetre or less. Once polyps are removed, they can be studied with the aid of a microscope to determine if they are precancerous or not. It can take up to 15 years for a polyp to turn cancerous.
Colonoscopy is similar to sigmoidoscopy—the difference being related to which parts of the colon each can examine. A colonoscopy allows an examination of the entire colon (1200–1500 mm in length). A sigmoidoscopy allows an examination of the distal portion (about 600 mm) of the colon, which may be sufficient because benefits to cancer survival of colonoscopy have been limited to the detection of lesions in the distal portion of the colon.[2][3][4]
A sigmoidoscopy is often used as a screening procedure for a full colonoscopy, often done in conjunction with a fecal occult blood test (FOBT). About 5% of these screened patients are referred to colonoscopy.[5]
Virtual colonoscopy, which uses 2D and 3D imagery reconstructed from computed tomography (CT) scans or from nuclear magnetic resonance (MR) scans, is also possible, as a totally non-invasive medical test, although it is not standard and still under investigation regarding its diagnostic abilities. Furthermore, virtual colonoscopy does not allow for therapeutic maneuvers such as polyp/tumour removal or biopsy nor visualization of lesions smaller than 5 millimeters. If a growth or polyp is detected using CT colonography, a standard colonoscopy would still need to be performed. Additionally, surgeons have lately been using the term pouchoscopy to refer to a colonoscopy of the ileo-anal pouch.
Medical uses
Conditions that call for colonoscopies include gastrointestinal hemorrhage, unexplained changes in bowel habit and suspicion of malignancy. Colonoscopies are often used to diagnose colon cancer, but are also frequently used to diagnose inflammatory bowel disease. In older patients (sometimes even younger ones) an unexplained drop in hematocrit (one sign of anemia) is an indication that calls for a colonoscopy, usually along with an esophagogastroduodenoscopy (EGD), even if no obvious blood has been seen in the stool (feces).
Fecal occult blood is a quick test which can be done to test for microscopic traces of blood in the stool. A positive test is almost always an indication to do a colonoscopy. In most cases the positive result is just due to hemorrhoids; however, it can also be due to diverticulosis, inflammatory bowel disease (Crohn's disease, ulcerative colitis), colon cancer, or polyps. However polypectomy has become a routine part of colonoscopy, allowing for quick and simple removal of polyps without invasive surgery.[6]
Colon cancer screening
Colonoscopy is one of the colorectal cancer screening tests available to people in the US who are over 50 years of age. The other screening tests include flexible sigmoidoscopy, double-contrast barium enema, computed tomographic (CT) colongraphy (virtual colonoscopy), guaiac-based fecal occult blood test (gFOBT), fecal immunochemical test (FIT), and multitarget stool DNA screening test (Cologuard).[7]
Subsequent rescreenings are then scheduled based on the initial results found, with a five- or ten-year recall being common for colonoscopies that produce normal results.[8] People with a family history of colon cancer are often first screened during their teenage years. Among people who have had an initial colonoscopy that found no polyps, the risk of developing colorectal cancer within five years is extremely low. Therefore, there is no need for those people to have another colonoscopy sooner than five years after the first screening.[9][10]
Medical societies recommend a screening colonoscopy every 10 years beginning at age 50 for adults without increased risk for colorectal cancer.[11] Research shows that the risk of cancer is low for 10 years if a high-quality colonoscopy does not detect cancer, so tests for this purpose are indicated every ten years.[11][12]
Colonoscopy screening prevents approximately two thirds of the deaths due to colorectal cancers on the left side of the colon, and is not associated with a significant reduction in deaths from right-sided disease.[2]
Colonoscopy reduces cancer rates by detecting some colon polyps and cancers on the left side of the colon early enough that they may be treated, and a smaller number on the right side; many of these left-sided growths would likewise have been detected by a safer sigmoidoscopy procedure.[2]
Since polyps often take 10 to 15 years to transform into cancer, in someone at average risk of colorectal cancer, guidelines recommend 10 years after a normal screening colonoscopy before the next colonoscopy. (This interval does not apply to people at high risk of colorectal cancer, or to those who experience symptoms of colorectal cancer.)[13][14]
Recommendations
The American Cancer Society recommends, beginning at age 50, both men and women follow one of these testing schedules for screening to find colon polyps and/or cancer:[15]
- Flexible sigmoidoscopy every 5 years, or
- Colonoscopy every 10 years, or
- Double-contrast barium enema every 5 years, or
- CT colonography (virtual colonoscopy) every 5 years
- Yearly guaiac-based fecal occult blood test (gFOBT)
- Yearly fecal immunochemical test (FIT)
- Stool DNA test (sDNA) every 3 years
Medicare coverage
In the United States, Medicare insurance covers the following colorectal-cancer screening tests:[16]
- Colonoscopy: average risk — every 10 years beginning at age 50, high risk — every 2 years with no age restriction
- Flexible sigmoidoscopy — every 4 years beginning at age 50
- Double-contrast barium enema: average risk — every 4 years beginning at age 50, high risk — every 2 years
- (CT) colongraphy: not covered by Medicare
- gFOBT: average risk — every year beginning at age 50
- FIT: average risk — every year beginning at age 50
- Cologuard: average risk — every 3 years beginning at age 50
Risks
1 in 200 people who have a colonoscopy have a serious complication.[17] Perforation of the colon occurs at a rate of about 1 in 1000 procedures, and death at a rate of 1 in 3300 to 1 in 333000; therefore, in some low-risk populations, screening in the absence of symptoms would not outweigh the risks of the procedure. For example, the odds of developing colorectal cancer between the ages of 20 and 40 are only 1 in 1250.[18] This procedure has a low (0.35%) risk of serious complications.[19][20] In a 2006 study of colonoscopies done from 1994 to 2002, Levin et al., found serious complications occurred in 1 of 200 colonoscopies,[17] comprising 1 in 1250 colonoscopies without biopsy or polypectomy, and a rate of 7.0 per 1000 for colonoscopies with biopsy or polypectomy; although McDonell and Loura criticize this rate as being unacceptably high.[21]
The rate of complications varies with the practitioner and institution performing the procedure, as well as a function of other variables.
The most serious complication generally is the gastrointestinal perforation, which is life-threatening and in most cases requires immediate major surgery for repair.[22] Fewer than 20% of cases may be successfully managed with a conservative (non-surgical) approach.[22] A 2003 summary study of 25,000 patients showed a perforation rate of 0.2%,[20] and a death rate of 0.006% on a total of 84,000 patients. The 2006 study by Levin et al. showed a perforation rate of 0.09%;[17] while a 2009 study quoted a similar perforation rate of 0.082%.[23] Appendicitis has been associated with either perforation or colonoscopy, in case reports in Korean, Italian and English journals.
According to a study published in the Annals of Internal Medicine, for which researchers reviewed colon cancer screening data from 1966 to 2001, the most severe complications from colonoscopy are perforation (that occurred in 0.029% to 0.72% of cases), heavy bleeding (occurring in 0.2% to 2.67% of colonoscopies) and death (occurring in 0.003% to 0.03% of colonoscopy patients).[24][25]
A 2003 analysis of the relative risks of sigmoidoscopy and colonoscopy, brought into attention that the risk of perforation after colonoscopy is approximately double that after sigmoidoscopy (consistent with the fact that colonoscopy examines a longer section of the colon), even though this difference appeared to be decreasing.[26]
Bleeding complications may be treated immediately during the procedure by cauterization via the instrument. Delayed bleeding may also occur at the site of polyp removal up to a week after the procedure and a repeat procedure can then be performed to treat the bleeding site. Even more rarely, splenic rupture can occur after colonoscopy because of adhesions between the colon and the spleen.
As with any procedure involving anaesthesia, other complications would include cardiopulmonary complications such as a temporary drop in blood pressure, and oxygen saturation usually the result of overmedication, and are easily reversed. Anesthesia can also increase the risk of developing blood clots and lead to pulmonary embolism or deep venous thrombosis. (DVT)[27] In rare cases, more serious cardiopulmonary events such as a heart attack, stroke, or even death may occur; these are extremely rare except in critically ill patients with multiple risk factors. In very rare cases, coma associated with anesthesia may occur.
Virtual colonoscopies carry risks that are associated with radiation exposure.
Severe dehydration caused by the laxatives that are usually administered during the bowel preparation for colonoscopy also may occur. Therefore, patients must drink large amounts of fluids during the days of colonoscopy preparation to prevent dehydration. Loss of electrolytes or dehydration is a potential risk that can even prove deadly.[27] In rare cases, severe dehydration can lead to kidney damage or renal dysfunction under the form of phosphate nephropathy.[28]
Colonoscopy preparation and colonoscopy procedure can cause inflammation of the bowels and diarrhea or even bowel obstruction.
During colonoscopies where a polyp is removed (a polypectomy), the risk of complications has been higher, although still very uncommon, at about 2.3 percent.[19] One of the most serious complications that may arise after colonoscopy is the postpolypectomy syndrome. This syndrome occurs due to potential burns to the bowel wall when the polyp is removed. It is however a very rare complication and as a result patients may experience fever and abdominal pain. The condition is treated with intravenous fluids and antibiotics while the patient is recommended to rest.
Bowel infections are a potential colonoscopy risk, although very rare. The colon is not a sterile environment as many bacteria live in the colon to ensure the well-functioning of the bowel and therefore the risk of infections is very low. Infections can occur during biopsies when too much tissue is removed and bacteria protrude in areas they do not belong to or in cases when the lining of the colon is perforated and the bacteria get into the abdominal cavity.[29] Infection may also be transmitted between patients if the colonoscope is not cleaned and sterilized properly between tests, although the risk of this happening is very low.[19]
Minor colonoscopy risks may include nausea, vomiting or allergies to the sedatives that are used. If medication is given intravenously, the vein may become irritated. Most localized irritations to the vein leave a tender lump lasting a number of days but going away eventually.[30] The incidence of these complications is less than 1%.
On very rare occasions, intracolonic explosion may occur.[31] A meticulous bowel preparation is the key to prevent this complication.[31]
Although complications after colonoscopy are uncommon, it is important for patients to recognize early signs of any possible complications. They include severe abdominal pain, fevers and chills, or rectal bleeding (more than half a cup).[32]
Procedure
Preparation
The colon must be free of solid matter for the test to be performed properly. For one to three days, the patient is required to follow a low fiber or clear-liquid only diet. Examples of clear fluids are apple juice, chicken and/or beef broth or bouillon, lemon-lime soda, lemonade, sports drink, and water. It is very important that the patient remain hydrated. Sports drinks contain electrolytes which are depleted during the purging of the bowel. Orange juice, prune juice, and milk containing fiber should not be consumed, nor should liquids dyed red, purple, orange, or sometimes brown; however, cola is allowed. In most cases, tea (no milk) or black coffee (no milk) are allowed.[33]
The day before the colonoscopy, the patient is either given a laxative preparation (such as Picosalax, Bisacodyl, phospho soda, sodium picosulfate, or sodium phosphate and/or magnesium citrate) and large quantities of fluid, or whole bowel irrigation is performed using a solution of polyethylene glycol and electrolytes. Often, the procedure involves both a pill-form laxative and a bowel irrigation preparation with the polyethylene glycol powder dissolved into any clear liquid, preferably a sports drink that contains electrolytes.

A typical procedure regimen then would be as follows: in the morning of the day before the procedure, a 238 g bottle of polyethylene glycol powder should be poured into 64 oz. (1.9 litres) of the chosen clear liquid, which then should be mixed and refrigerated. Two (2) bisacodyl 5 mg tablets are taken 3 pm; at 5 pm, the patient starts drinking the mixture (approx. 8 oz. (0.5 litres) each 15-30 min. until finished); at 8 pm, take two (2) bisacodyl 5 mg tablets; continue drinking/hydrating into the evening until bedtime with clear permitted fluids. A common brand name of bisacodyl is Dulcolax, and store brands are available. A common brand name of polyethylene glycol powder is MiraLAX. It may be advisable to schedule the procedure early on a given day so the patient need not go without food and only limited fluids the morning of the procedure on top of having to go through the foregoing preparation procedures the preceding day.
Since the goal of the preparation is to clear the colon of solid matter, the patient should plan to spend the day at home in comfortable surroundings with ready access to toilet facilities. The patient may also want to have at hand moist towelettes or a bidet for cleaning the anus. A soothing salve such as petroleum jelly applied after cleaning the anus will improve patient comfort.
The patient may be asked to skip aspirin and aspirin-like products such as salicylate, ibuprofen, and similar medications for up to ten days before the procedure to avoid the risk of bleeding if a polypectomy is performed during the procedure. A blood test may be performed before the procedure.[34][35]
Some hospitals and clinics have begun to utilize a technique used in colon hydrotherapy as an alternative to the standard preparation methods described above. In this case, special equipment is used to gently flush the patient's colon with warm water, just prior to the colonoscopy procedure, in order to remove any bowel contents. This alleviates the patient from having to ingest large quantities of fluids, or risk nausea, vomiting, or anal irritation. The time required for preparation overall is significantly reduced, which often facilitates easier scheduling of the procedure.[36]
Investigation
During the procedure the patient is often given sedation intravenously, employing agents such as fentanyl or midazolam. Although meperidine (Demerol) may be used as an alternative to fentanyl, the concern of seizures has relegated this agent to second choice for sedation behind the combination of fentanyl and midazolam. The average person will receive a combination of these two drugs, usually between 25 and 100 µg IV fentanyl and 1–4 mg IV midazolam. Sedation practices vary between practitioners and nations; in some clinics in Norway, sedation is rarely administered.[37][38]
Some endoscopists are experimenting with, or routinely use, alternative or additional methods such as nitrous oxide[39][40] and propofol,[41] which have advantages and disadvantages relating to recovery time (particularly the duration of amnesia after the procedure is complete), patient experience, and the degree of supervision needed for safe administration. This sedation is called "twilight anesthesia". For some patients it is not fully effective, so they are indeed awake for the procedure and can watch the inside of their colon on the color monitor. Substituting propofol for midazolam, which gives the patient quicker recovery, is gaining wider use, but requires closer monitoring of respiration.
A meta-analysis found that playing music improves patient tolerability of the procedure.[42]
The first step is usually a digital rectal examination, to examine the tone of the sphincter and to determine if preparation has been adequate. The endoscope is then passed through the anus up the rectum, the colon (sigmoid, descending, transverse and ascending colon, the cecum), and ultimately the terminal ileum. The endoscope has a movable tip and multiple channels for instrumentation, air, suction and light. The bowel is occasionally insufflated with air to maximize visibility (a procedure which gives one the false sensation of needing to take a bowel movement).[43] Biopsies are frequently taken for histology. Additionally in a procedure known as chromoendoscopy, a contrast-dye (such as Indigo carmine) may be sprayed via the endoscope onto the bowel wall to help visualise any abnormalities in the mucosal morphology. A Cochrane review updated in 2016 found strong evidence that chromoscopy enhances the detection of cancerous tumours in the colon and rectum[44]
In most experienced hands, the endoscope is advanced to the junction of where the colon and small bowel join up (cecum) in under 10 minutes in 95% of cases. Due to tight turns and redundancy in areas of the colon that are not "fixed", loops may form in which advancement of the endoscope creates a "bowing" effect that causes the tip to actually retract. These loops often result in discomfort due to stretching of the colon and its associated mesentery. Manoeuvres to "reduce" or remove the loop include pulling the endoscope backwards while torquing the instrument. Alternatively, body position changes and abdominal support from external hand pressure can often "straighten" the endoscope to allow the scope to move forward. In a minority of patients, looping is often cited as a cause for an incomplete examination. Usage of alternative instruments leading to completion of the examination has been investigated, including use of pediatric colonoscope, push enteroscope and upper GI endoscope variants.[45]
For screening purposes, a closer visual inspection is then often performed upon withdrawal of the endoscope over the course of 20 to 25 minutes. Lawsuits over missed cancerous lesions have recently prompted some institutions to better document withdrawal time as rapid withdrawal times may be a source of potential medical legal liability.[46] This is often a real concern in clinical settings where high caseloads could provide financial incentive to complete colonoscopies as quickly as possible.
Suspicious lesions may be cauterized, treated with laser light or cut with an electric wire for purposes of biopsy or complete removal polypectomy. Medication can be injected, e.g. to control bleeding lesions. On average, the procedure takes 20–30 minutes, depending on the indication and findings. With multiple polypectomies or biopsies, procedure times may be longer. As mentioned above, anatomic considerations may also affect procedure times.
After the procedure, some recovery time is usually allowed to let the sedative wear off. Outpatient recovery time can take an estimate of 30–60 minutes. Most facilities require that patients have a person with them to help them home afterwards (again, depending on the sedation method used).
One very common aftereffect from the procedure is a bout of flatulence and minor wind pain caused by air insufflation into the colon during the procedure.
An advantage of colonoscopy over x-ray imaging or other, less invasive tests, is the ability to perform therapeutic interventions during the test. A polyp is a growth of excess of tissue that can develop into cancer. If a polyp is found, for example, it can be removed by one of several techniques. A snare device can be placed around a polyp for removal. Even if the polyp is flat on the surface it can often be removed. For example, the following shows a polyp removed in stages:
 Polyp is identified.
Polyp is identified. A sterile solution is injected under the polyp to lift it away from deeper tissues.
A sterile solution is injected under the polyp to lift it away from deeper tissues.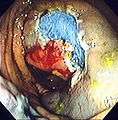 A portion of the polyp is now removed.
A portion of the polyp is now removed.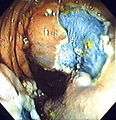 The polyp is fully removed.
The polyp is fully removed.
Pain management
The pain associated with the procedure is not caused by the insertion of the scope but rather by the inflation of the colon in order to do the inspection. The scope itself is essentially a long, flexible tube about a centimetre in diameter, i.e. as big around as the little finger, which is less than the diameter of an average stool.
The colon is wrinkled and corrugated, somewhat like an accordion or a clothes-dryer exhaust tube, which gives it the large surface area needed for water absorption. In order to inspect this surface thoroughly the physician blows it up like a balloon, using an air compressor, in order to get the creases out. The stomach, intestines and colon have a so-called "second brain" wrapped around them, which autonomously runs the chemical factory of digestion.[47] It uses complex hormone signals and nerve signals to communicate with the brain and the rest of the body. Normally a colon's job is to digest food and regulate the intestinal flora. The harmful bacteria in rancid food, for example, creates gas. The colon has distension sensors that can tell when there is unexpected gas pushing the colon walls out—thus the "second brain" tells the person that he or she is having intestinal difficulties by way of the sensation of nausea. Doctors typically recommend either total anaesthesia or a partial twilight sedative to either preclude or to lessen the patient's awareness of pain or discomfort, or just the unusual sensations of the procedure. Once the colon has been inflated, the doctor inspects it with the scope as it is slowly pulled backwards. If any polyps are found they are then cut out for later biopsy.
Some doctors prefer to work with totally anesthetized patients inasmuch as the lack of any perceived pain or discomfort allows for a leisurely examination. Twilight sedation is, however, inherently safer than general anesthesia; it also allows the patients to follow simple commands and even to watch the procedure on a closed-circuit monitor. Tens of millions of adults annually need to have colonoscopies, and yet many don't because of concerns about the procedure.
It is worth noting that in many hospitals (for instance St. Mark's Hospital, London, which specialises in intestinal and colorectal medicine) colonoscopies are carried out without any sedation. This allows the patient to shift his or her body position to help the doctor carry out the procedure and significantly reduces recovery time and side-effects. Although there is some discomfort when the colon is distended with air, this is not usually particularly painful and it passes relatively quickly. Patients can then be released from hospital on their own very swiftly without any feelings of nausea.
Ultrasound
Duodenography and colonography are performed like a standard abdominal examination using B-mode and color flow Doppler ultrasonography using a low frequency transducer — for example a 2.5 MHz — and a high frequency transducer, for example a 7.5 MHz probe. Detailed examination of duodenal walls and folds, colonic walls and haustra was performed using a 7.5 MHz probe. Deeply located abdominal structures were examined using 2.5 MHz probe. All ultrasound examinations are performed after overnight fasting (for at least 16 hours) using standard scanning procedure. Subjects are examined with and without water contrast. Water contrast imaging is performed by having adult subjects take at least one liter of water prior to examination. Patients are examined in the supine, left posterior oblique, and left lateral decubitus positions using the intercostal and subcostal approaches. The liver, gall bladder, spleen, pancreas, duodenum, colon, and kidneys are routinely evaluated in all patients. With patient lying supine, the examination of the duodenum with high frequency ultrasound duodenography is performed with 7.5 MHz probe placed in the right upper abdomen, and central epigastric successively; for high frequency ultrasound colonography, the ascending colon, is examined with starting point usually midway of an imaginary line running from the iliac crest to the umbilicus and proceeding cephalid through the right mid abdomen; for the descending colon, the examination begins from the left upper abdomen proceeding caudally and traversing the left mid abdomen and left lower abdomen, terminating at the sigmoid colon in the lower pelvic region. Color flow Doppler sonography is used to examine the localization of lesions in relation to vessels. All measurements of diameter and wall thickness are performed with built-in software. Measurements are taken between peristaltic waves.[48]
 The abdominal regions scanned in the order.
The abdominal regions scanned in the order. The duodenal tri-band wall with folds of Kerckring, showing floaters with water contrast.
The duodenal tri-band wall with folds of Kerckring, showing floaters with water contrast. A high resolution view of colonic haustration.
A high resolution view of colonic haustration.
Economics
Researchers have found that older patients with three or more significant health problems, like dementia or heart failure, had high rates of repeat colonoscopies without medical indications. These patients are less likely to live long enough to develop colon cancer. Gordon states, "At about $1,000 per procedure, there’s clearly an economic incentive".[14]
The Hemoccult II FOBT (combined with follow-up colonoscopy if indicated by the test) is over 5 times as cost effective as other screening strategies, but has only about 85% as sensitive. Because of this relatively low sensitivity, US guidelines advocate the over 5 times more expensive procedures instead, because even the relatively small increase in lives saved and 5-fold cost increase is seen as worth choosing, given US living standards.[49]
History
In the 1960s, Dr. Niwa and Dr Yamagata at Tokyo University developed the device. After 1968, Dr. William Wolff and Dr. Hiromi Shinya became pioneered the development of the colonoscope.[50] Their invention, in 1969 in Japan, was an advance over the barium enema and the flexible sigmoidoscope because it allowed for the visualization and removal of polyps from the entire large intestine. Wolff and Shinya advocated for their invention and published much of the early evidence needed to overcome skepticism about the device’s safety and efficacy. Colonoscopy with CCD invention and market is led by Fuji film, Olympus and Hoya in Japan. [51]
Etymology
The terms colonoscopy[52][53][54] or coloscopy[53] are derived from[53] the ancient Greek noun κόλον, same as English colon,[55] and the verb σκοπεῖν, look (in)to, examine.[55] The term colonoscopy is however ill-constructed,[56] as this form supposes that the first part of the compound consists of a possible root κολωv- or κολοv-, with the connecting vowel -o, instead of the root κόλ- of κόλον.[56] A compound such as κολωνοειδής, like a hill,[55] (with the additional -on-) is derived from the ancient Greek word κολώνη or κολωνός, hill.[55] Similarly, colonoscopy (with the additional -on-) can literally be translated as examination of the hill,[56] instead of the examination of the colon.
In English, multiple words exist that are derived from κόλον, such as colectomy,[53][57] colocentesis,[53] colopathy,[53] and colostomy[53] among many others, that actually lack the incorrect additional -on-. It must be noted that a few compounds have doublets with -on- inserted, like colonopathy.[53][54]
See also
- Bow and arrow sign
- Esophagogastroduodenoscopy
- Polypectomy
- Rectal examination
- Sigmoidoscopy
- Virtual colonoscopy
References
- ↑ American Heritage Medical Dictionary
- 1 2 3 Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L (January 2009). "Association of colonoscopy and death from colorectal cancer". Ann. Intern. Med. 150 (1): 1–8. doi:10.1059/0003-4819-150-1-200901060-00306. PMID 19075198. as PDF Archived January 18, 2012, at the Wayback Machine.
- ↑ Singh H, Nugent Z, Mahmud SM, Demers AA, Bernstein CN (March 2010). "Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies". Am J Gastroenterol. 105 (3): 663–673. doi:10.1038/ajg.2009.650. PMID 19904239.
- ↑ Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Alterhofen L, Haug U (January 2010). "Protection from right- and left-sided colorectal neoplasms after colonoscopy: population-based study". J Natl Cancer Inst. 102 (2): 89–95. doi:10.1093/jnci/djp436. PMID 20042716.
- ↑ Atkin WS, Edwards R, Kralj-Hans I, et al. (May 2010). "Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial". Lancet. 375 (9726): 1624–33. doi:10.1016/S0140-6736(10)60551-X. PMID 20430429. as PDF Archived March 24, 2012, at the Wayback Machine.
- ↑ Sivak Jr., Michael V. (December 2004). "Polypectomy: Looking Back". Gastrointestinal Endoscopy. 60 (6): 977–982. doi:10.1016/S0016-5107(04)02380-6. PMID 15605015.
- ↑ "Colorectal Cancer Prevention and Early Detection" (PDF). American Cancer Society. February 5, 2015. pp. 16–24. Retrieved 2015-12-25.
- ↑ Rex, Douglas K.; Bond,John H.; Winawer,Sidney; Levin,Theodore R.; Burt,Randall W.; Johnson,David A.; Kirk,Lynne M.; Litlin,Scott; Lieberman,David A.; Waye,Jerome D.; Church,James; Marshall,John B.; Riddell,Robert H. (June 2002). "Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer". The American Journal of Gastroenterology. 97 (6): 1296–1308. doi:10.1111/j.1572-0241.2002.05812.x. PMID 12094842.
- ↑ Gmperiale, Thomas F.; Glowinski, Elizabeth A.; Lin-Cooper, Ching; Larkin, Gregory N.; Rogge, James D.; Ransohoff, David F. (2008). "Five-Year Risk of Colorectal Neoplasia after Negative Screening Colonoscopy". N Engl J Med. 359 (12): 1218–1224. doi:10.1056/NEJMoa0803597. PMID 18799558. Retrieved 2008-09-17.
- ↑ No Need to Repeat Colonoscopy Until 5 Years After First Screening Newswise, Retrieved on September 17, 2008.
- 1 2 Winawer, S.; Fletcher, R.; Rex, D.; Bond, J.; Burt, R.; Ferrucci, J.; Ganiats, T.; Levin, T.; Woolf, S.; Johnson, D.; Kirk, L.; Litin, S.; Simmang, C.; Gastrointestinal Consortium, P. (2003). "Colorectal cancer screening and surveillance: Clinical guidelines and rationale—Update based on new evidence". Gastroenterology. 124 (2): 544–560. doi:10.1053/gast.2003.50044. PMID 12557158.
- ↑ American Gastroenterological Association, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American Gastroenterological Association, archived from the original (PDF) on August 9, 2012, retrieved August 17, 2012
- ↑ Cancerconnect, Interval between Colonoscopies May be Shorter than Recommended (accessed 2 June 2011)
- 1 2 Goodwin JS, Singh A, Reddy N, Riall TS, Kuo YF (August 2011). "Overuse of screening colonoscopy in the medicare population". Arch. Intern. Med. 171 (15): 1335–43. doi:10.1001/archinternmed.2011.212. PMID 21555653.
- ↑ "American Cancer Society Guidelines for the Early Detection of Cancer"
- ↑ "Your Medicare Coverage: Colorectal cancer screenings". Medicare.gov. Retrieved 2015-12-25.
- 1 2 3 Levin TR, Zhao W, Conell C, et al. (December 2006). "Complications of colonoscopy in an integrated health care delivery system". Ann. Intern. Med. 145 (12): 880–6. doi:10.7326/0003-4819-145-12-200612190-00004. PMID 17179057.
- ↑ Cancer of the colon and rectum (invasive). SEER Cancer Statistics Review 1975-2009
- 1 2 3 "Colonoscopy Risks". Retrieved 2010-11-02.
- 1 2 J. A. Dominitz, et al., American Society for Gastrointestinal Endoscopy, ; "Complications of Colonsocopy", Gastrointestinal Endoscopy, Vol 57, No. 4, 2003, pp. 441-445
- ↑ McDonnell WM, Loura F (August 2007). "Complications of colonoscopy". Ann. Intern. Med. 147 (3): 212–3; author reply 213–4. doi:10.7326/0003-4819-147-3-200708070-00016. PMID 17679710.
- 1 2 Sartelli M, Viale P, Catena F, Ansaloni L, Moore E, Malangoni M, et al. (2013). "2013 WSES guidelines for management of intra-abdominal infections". World J Emerg Surg (Review). 8 (1): 3. doi:10.1186/1749-7922-8-3. PMC 3545734
 . PMID 23294512.
. PMID 23294512. - ↑ Arora G, Mannalithara A, Singh G, Gerson LB, Triadafilopoulos G (March 2009). "Risk of perforation from a colonoscopy in adults: a large population-based study". Gastrointest. Endosc. 69 (3 Pt 2): 654–64. doi:10.1016/j.gie.2008.09.008. PMID 19251006.
- ↑ Donna Myers (about.com). "Overview of Colonoscopy Risks". Retrieved 2011-06-02.
- ↑ Pignone, M; Rich M; Teutsch SM; Berg AO; Lohr KN (16 July 2002). "Screening for Colorectal Cancer in Adults at Average Risk: A Summary of the Evidence for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 137 (2): 132–41. doi:10.7326/0003-4819-137-2-200207160-00015. PMID 12118972. Retrieved 2012-08-30.
- ↑ Gatto, NM; Frucht H; Sundararajan V; Jacobson JS; Grann VR; Neugut AI (5 Feb 2003). "Risk of Perforation After Colonoscopy and Sigmoidoscopy: A Population-Based Study". Journal of the National Cancer Institute. 95 (3): 230–6. doi:10.1093/jnci/95.3.230. PMID 12569145. Retrieved 2012-08-30.
- 1 2 "What are the colonoscopy risks?: Colonoscopy Risks That Become Potential Colonoscopy Complications". Retrieved 2010-04-06.
- ↑ Lien YH (September 2008). "Is bowel preparation before colonoscopy a risky business for the kidney?". Nat Clin Pract Nephrol. 4 (11): 606–14. doi:10.1038/ncpneph0939. PMID 18797448.
- ↑ "Bowel Infections". Retrieved 2010-04-06.
- ↑ "What to expect after a colonoscopy?". Retrieved 2010-04-06.
- 1 2 Ladas SD, Karamanolis G, Ben-Soussan E (2007). "Colonic gas explosion during therapeutic colonoscopy with electrocautery". World J Gastroenterol (Review). 13 (40): 5295–8. PMC 4171316
 . PMID 17879396.
. PMID 17879396. - ↑ "Colonoscopy A Guide to the Procedure". Retrieved 2010-04-06.
- ↑ Waye, Jerome D.; Rex, Douglas K.; Williams, Christopher Beverley (2003). Colonoscopy: principles and practice. Wiley-Blackwell. pp. 210–211. ISBN 1-4051-1449-5.
- ↑ Decker, Joe (15 November 2006). "Preparation: Diet" (Blog). Colonoscopy Blog. Blogger.com. Retrieved 2007-06-12.
- ↑ "Colyte/Trilyte Colonoscopy Preparation" (PDF). Palo Alto Medical Foundation. June 2006. Archived from the original (PDF) on April 14, 2007. Retrieved 2007-06-12.
- ↑ Colon Hydrotherapy: New Method of Colonoscopy Prep, Healthy Beginnings Magazine, 11 September 2011
- ↑ Bretthauer, M; Hoff G; Severinsen H; Erga J; Sugar J; Huppertz-Hauss G (20 May 2004). "[Systematic quality control programme for colonoscopy in an endoscopy centre in Norway]". Tidsskrift for den Norske laegeforening (in Norwegian). 124 (10): 1402–5. PMID 15195182.
- ↑
- ↑ Rikshospitalet University Hospital (April 2006). "Clinical Trial: Nitrous Oxide for Analgesia During Colonoscopy". ClinicalTrials.gov. Retrieved 2007-06-12.
- ↑ Forbes, GM; Collins BJ (March 2000). "Nitrous oxide for colonoscopy: a randomized controlled study". Gastrointestinal Endoscopy. 51 (3): 271–7. doi:10.1016/S0016-5107(00)70354-3. PMID 10699770.
- ↑ Clarke, Anthony C; Louise Chiragakis; Lybus C Hillman; Graham L Kaye (18 February 2002). "Sedation for endoscopy: the safe use of propofol by general practitioner sedationists". Medical Journal of Australia. 176 (4): 158–161. PMID 11913915.
- ↑ Bechtold, ML.; Puli, SR.; Othman, MO.; Bartalos, CR.; Marshall, JB.; Roy, PK. (Jan 2009). "Effect of music on patients undergoing colonoscopy: a meta-analysis of randomized controlled trials". Dig Dis Sci. 54 (1): 19–24. doi:10.1007/s10620-008-0312-0. PMID 18483858.
- ↑ American Gastroenterological Association video
- ↑ Brown SR; Baraza W; Din S; Riley S (2016). "Chromoscopy versus conventional endoscopy for the detection of polyps in the colon and rectum". Cochrane Database of Systematic Reviews (4). doi:10.1002/14651858.CD006439.pub4.
- ↑ Lichtenstein, Gary R.; Peter D. Park; William B. Long; Gregory G. Ginsberg; Michael L. Kochman (18 August 1998). "Use of a Push Enteroscope Improves Ability to Perform Total Colonoscopy in Previously Unsuccessful Attempts at Colonoscopy in Adult Patients". The American Journal of Gastroenterology. 94 (1): 187–90. doi:10.1111/j.1572-0241.1999.00794.x. PMID 9934753. Note:Single use PDF copy provided free by Blackwell Publishing for purposes of Wikipedia content enrichment.
- ↑ Barclay RL, Vicari JJ, Doughty AS, et al. (2006). "Colonoscopic withdrawal times and adenoma detection during screening colonoscopy". New England Journal of Medicine. 355 (24): 2533–41. doi:10.1056/nejmoa055498.
- ↑ "Our Second Brain: The Stomach". May 1999. Retrieved 2010-06-29.
- ↑ Njemanze PC, Njemanze J, Skelton A, et al. (July 2008). "High-frequency ultrasound imaging of the duodenum and colon in patients with symptomatic giardiasis in comparison to amebiasis and healthy subjects". J. Gastroenterol. Hepatol. 23 (7 Pt 2): e34–42. doi:10.1111/j.1440-1746.2007.05056.x. PMID 17645477.
- ↑ PMID 20889076
- ↑ Wolff WI. (September 1989). "Colonoscopy: History and development.". Am J Gastroenterol. 84 (9): 1017–25. PMID 2672788.
- ↑ Wolff WI, Shinya H (September 1974). "Earlier diagnosis of cancer of the colon through colonic endoscopy (colonoscopy)". Cancer. 34 (Supplement S3): 912–931. doi:10.1002/1097-0142(197409)34:3+<912::AID-CNCR2820340720>3.0.CO;2-P. PMID 4851470.
- ↑ Dorland, W. A. N. & Miller, E.C.L. (1948). The American illustrated medical dictionary. (21st edition). Philadelphia/London: W.B. Saunders Company.
- 1 2 3 4 5 6 7 8 Dirckx, J.H. (Ed.) (1997).Stedman’s concise medical dictionary for the health professions. (3rd edition). Baltimore: Williams & Wilkins.
- 1 2 Anderson, D.M. (2000). Dorland’s illustrated medical dictionary (29th edition). Philadelphia/London/Toronto/Montreal/Sydney/Tokyo: W.B. Saunders Company.
- 1 2 3 4 Liddell, H.G. & Scott, R. (1940). A Greek-English Lexicon. revised and augmented throughout by Sir Henry Stuart Jones. with the assistance of. Roderick McKenzie. Oxford: Clarendon Press.
- 1 2 3 Anastassiades, C.P., Cremonini, F. & Hadjinicolaou, D. (2008). Colonoscopy and colonography: back to the roots. '’European Review for Medical and Pharmacological Sciences, 12’’, 345-347.
- ↑ Foster, F.D. (1891-1893). An illustrated medical dictionary. Being a dictionary of the technical terms used by writers on medicine and the collateral sciences, in the Latin, English, French, and German languages. New York: D. Appleton and Company.
External links
- LearnColoRectalSurgery.com — Colonoscopy pictures
- Colonoscopy. Based on public-domain NIH Publication No. 02-4331, dated February 2002.
- Patient Education Brochures. American Society for Gastrointestinal Endoscopy information
- colonoscopy app. Colonoscopy app is now available for android phones and IPhones.
- Preparing for a Colonoscopy American Gastroenterological Association video
- Colonoscopy walkthrough and risks
- What is Third Eye colonoscopy? Third Eye Colonoscopy
- Colonoscopy, procedure with video Colonoscopy, procedure with video
- Polypectomy Colonoscopy, procedure video with polypectomy
- Blood in the Toilet Promoting awareness of bower cancer prevention by polyp removal
- Colonoscopy information Gupta Gastroenterology Colonoscopy procedure information
- Colorectal Cancer Incidence and Screening — United States, 2008 and 2010 Centers for Disease Control and Prevention
- Endoscopic Full-Thickness Resection (eFTR) allows for the removal of lesions in the colon and rectum.