Paracentesis
| Paracentesis | |
|---|---|
| Intervention | |
| ICD-9-CM | 54.91 |
| MeSH | D019152 |
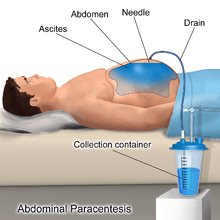
Paracentesis (from Greek κεντάω, "to pierce") is a form of body fluid sampling procedure, generally referring to peritoneocentesis (also called laparocentesis) in which the peritoneal cavity is punctured by a needle to sample peritoneal fluid.[1][2]
Indications
It is used for a number of reasons:
- to relieve abdominal pressure from ascites
- to diagnose spontaneous bacterial peritonitis and other infections (e.g. abdominal TB)
- to diagnose metastatic cancer
- to diagnose blood in peritoneal space in trauma
Paracentesis for ascites
The procedure is often performed in a doctor's office or an outpatient clinic. In an expert's hands it is usually very safe, although there is a small risk of infection, excessive bleeding or perforating a loop of bowel. These last two risks can be minimized greatly with the use of ultrasound guidance.
The patient is requested to urinate before the procedure; alternately, a Foley catheter is used to empty the bladder. The patient is positioned in the bed with the head elevated at 45-60 degrees to allow fluid to accumulate in lower abdomen. After cleaning the side of the abdomen with an antiseptic solution, the physician numbs a small area of skin and inserts a large-bore needle with a plastic sheath 2 to 5 cm (1 to 2 in) in length to reach the peritoneal (ascitic) fluid. The needle is removed, leaving the plastic sheath to allow drainage of the fluid. The fluid is drained by gravity, a syringe or by connection to a vacuum bottle. Several litres of fluid may be drained during the procedure; however, if more than two litres are to be drained it will usually be done over the course of several treatments. If fluid drainage is more than 5 litres, patients may receive intravenous serum albumin (25% albumin, 8g/L) to prevent hypotension (low blood pressure). After the desired level of drainage is complete, the plastic sheath is removed and the puncture site bandaged. The plastic sheath can be left in place with a flow control valve and protective dressing if further treatments are expected to be necessary.
The procedure generally is not painful and does not require sedation. The patient is usually discharged within several hours following post-procedure observation provided that blood pressure is otherwise normal and the patient experiences no dizziness.[1][3][4]
Ascitic fluid analysis
The serum-ascites albumin gradient can help determine the cause of the ascites. The ascitic white blood cell count can help determine if the ascites is infected.
Contraindications
Mild hematologic abnormalities do not increase the risk of bleeding.[5][6] The risk of bleeding may be increased if:[7]
- prothrombin time > 21 seconds
- international normalized ratio > 1.6
- platelet count < 50,000 per cubic millimeter.
Absolute contraindication is acute abdomen that requires surgery. Relative contraindications are:
- Pregnancy
- Distended urinary bladder
- Abdominal wall cellulitis
- Distended bowel
- Intra-abdominal adhesions.[1]
References
- 1 2 3 Paracentesis at eMedicine
- ↑ Farlex dictionary > paracentesis, citing:
- Gale Encyclopedia of Medicine. Copyright 2008
- The American Heritage Medical Dictionary Copyright 2007
- McGraw-Hill Concise Dictionary of Modern Medicine. Copyright 2002
- ↑ http://patients.dartmouth-hitchcock.org/gi/paracentesis.html[]
- ↑ http://apps.med.buffalo.edu/procedures/paracentesis.asp?p=15[]
- ↑ McVay, PA; Toy, PT (1991). "Lack of increased bleeding after paracentesis and thoracentesis in patients with mild coagulation abnormalities". Transfusion. 31 (2): 164–71. doi:10.1046/j.1537-2995.1991.31291142949.x. PMID 1996485.
- ↑ Moore, K P; Aithal, G. P. (2006). "Guidelines on the management of ascites in cirrhosis". Gut. 55: vi1–12. doi:10.1136/gut.2006.099580. PMC 1860002
 . PMID 16966752.
. PMID 16966752. - ↑ Ginès, Pere; Cárdenas, Andrés; Arroyo, Vicente; Rodés, Juan (2004). "Management of Cirrhosis and Ascites". New England Journal of Medicine. 350 (16): 1646–54. doi:10.1056/NEJMra035021. PMID 15084697.
External links
- Paracentesis - a step-by-step procedure guide. Clinical Notes.
- WebMD: Patient guide