Cornea
| Cornea | |
|---|---|
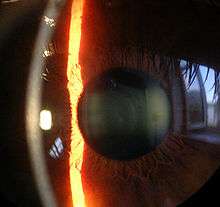
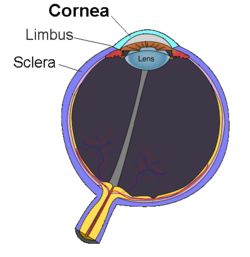 Schematic diagram of the human eye showing the cornea as separated from the sclera by the corneal limbus | |
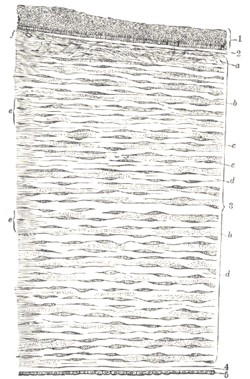 Vertical section of human cornea from near the margin. (Waldeyer.) Magnified.
| |
| Identifiers | |
| MeSH | D00331 |
| TA | A15.2.02.012 |
| FMA | 58238 |
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. The cornea, with the anterior chamber and lens, refracts light, with the cornea accounting for approximately two-thirds of the eye's total optical power.[1][2] In humans, the refractive power of the cornea is approximately 43 dioptres.[3] While the cornea contributes most of the eye's focusing power, its focus is fixed. The curvature of the lens, on the other hand, can be adjusted to "tune" the focus depending upon the object's distance. Medical terms related to the cornea often start with the prefix "kerat-" from the Greek word κέρας, horn.
Structure
The cornea has unmyelinated nerve endings sensitive to touch, temperature and chemicals; a touch of the cornea causes an involuntary reflex to close the eyelid. Because transparency is of prime importance the cornea does not have blood vessels; it receives nutrients via diffusion from the tear fluid through the outside surface and the aqueous humour through the inside surface, and also from neurotrophins supplied by nerve fibres that innervate it. In humans, the cornea has a diameter of about 11.5 mm and a thickness of 0.5–0.6 mm in the center and 0.6–0.8 mm at the periphery. Transparency, avascularity, the presence of immature resident immune cells, and immunologic privilege makes the cornea a very special tissue. The cornea has no blood supply; it gets oxygen directly through the air. Oxygen first dissolves in the tears and then diffuses throughout the cornea to keep it healthy.[4]
It borders with the sclera by the corneal limbus.
The most abundant soluble protein in mammalian cornea is albumin.[5]
In lampreys, the cornea is solely an extension of the sclera, and is separate from the skin above it, but in more advanced vertebrates it is always fused with the skin to form a single structure, albeit one composed of multiple layers. In fish, and aquatic vertebrates in general, the cornea plays no role in focusing light, since it has virtually the same refractive index as water.[6]
Layers
The human cornea has five (possibly six) layers.[7] Corneas of other primates have five known layers; the corneas of cats, dogs, wolves, and other carnivores only have four.[8] From the anterior to posterior the layers of the human cornea are:
- Corneal epithelium: an exceedingly thin multicellular epithelial tissue layer (non-keratinized stratified squamous epithelium) of fast-growing and easily regenerated cells, kept moist with tears. Irregularity or edema of the corneal epithelium disrupts the smoothness of the air/tear-film interface, the most significant component of the total refractive power of the eye, thereby reducing visual acuity. It is continuous with the conjunctival epithelium, and is composed of about 6 layers of cells which are shed constantly on the exposed layer and are regenerated by multiplication in the basal layer.
- Bowman's layer (also known as the anterior limiting membrane): when discussed in lieu of a subepithelial basement membrane, Bowman's Layer is a tough layer composed of collagen (mainly type I collagen fibrils), laminin, nidogen, perlecan and other HSPGs that protects the corneal stroma. When discussed as a separate entity from the subepithelial basement membrane, Bowman's Layer can be described as an acellular, condensed region of the apical stroma, composed primarily of randomly organized yet tightly woven collagen fibrils. These fibrils interact with and attach onto each other. This layer is eight to 14 micrometres (μm) thick[9] and is absent or very thin in non-primates.[8][10]
- Corneal stroma (also substantia propria): a thick, transparent middle layer, consisting of regularly arranged collagen fibers along with sparsely distributed interconnected keratocytes, which are the cells for general repair and maintenance.[9] They are parallel and are superimposed like book pages. The corneal stroma consists of approximately 200 layers of mainly type I collagen fibrils. Each layer is 1.5-2.5 μm. Up to 90% of the corneal thickness is composed of stroma.[9] There are 2 theories of how transparency in the cornea comes about:
- The lattice arrangements of the collagen fibrils in the stroma. The light scatter by individual fibrils is cancelled by destructive interference from the scattered light from other individual fibrils.[11]
- The spacing of the neighboring collagen fibrils in the stroma must be < 200 nm for there to be transparency. (Goldman and Benedek)
- Descemet's membrane (also posterior limiting membrane): a thin acellular layer that serves as the modified basement membrane of the corneal endothelium, from which the cells are derived. This layer is composed mainly of collagen type IV fibrils, less rigid than collagen type I fibrils, and is around 5-20 μm thick, depending on the subject's age. Just anterior to Descemet's membare, a very thin and strong layer, the Dua's Layer, 15 microns thick and able to withstand 1.5 to 2 bars of pressure, may exist according to one study,[12] but to date (November 2014) this has not been replicated in another laboratory.
- Corneal endothelium: a simple squamous or low cuboidal monolayer, approx 5 μm thick, of mitochondria-rich cells. These cells are responsible for regulating fluid and solute transport between the aqueous and corneal stromal compartments.[13] (The term endothelium is a misnomer here. The corneal endothelium is bathed by aqueous humor, not by blood or lymph, and has a very different origin, function, and appearance from vascular endothelia.) Unlike the corneal epithelium, the cells of the endothelium do not regenerate. Instead, they stretch to compensate for dead cells which reduces the overall cell density of the endothelium, which affects fluid regulation. If the endothelium can no longer maintain a proper fluid balance, stromal swelling due to excess fluids and subsequent loss of transparency will occur and this may cause corneal edema and interference with the transparency of the cornea and thus impairing the image formed.[13] Iris pigment cells deposited on the corneal endothelium can sometimes be washed into a distinct vertical pattern by the aqueous currents - this is known as Krukenberg's Spindle.
Mnemonic for the Layers
(Anterior to Posterior)
ABCDE
A: Anterior corneal epithelium B : Bowman's layer C : Corneal stroma D : Descemet's membrane E : Endothelium
Innervation
The cornea is one of the most sensitive tissues of the body, as it is densely innervated with sensory nerve fibres via the ophthalmic division of the trigeminal nerve by way of 70–80 long ciliary nerves and short ciliary nerves. Research suggests the density of pain receptors in the cornea is 300-600 times greater than skin and 20-40 times greater than dental pulp,[14] making any injury to the structure excruciatingly painful.[15]
The ciliary nerves run under the endothelium and exit the eye through holes in the sclera apart from the optic nerve (which transmits only optic signals).[9] The nerves enter the cornea via three levels; scleral, episcleral and conjunctival. Most of the bundles give rise by subdivision to a network in the stroma, from which fibres supply the different regions. The three networks are, midstromal, subepithelial/sub-basal, and epithelial. The receptive fields of each nerve ending are very large, and may overlap.
Corneal nerves of the subepithelial layer terminate near the superficial epithelial layer of the cornea in a logarithmic spiral pattern.[16] The density of epithelial nerves decreases with age, especially after the seventh decade.[17]
Refractive nature
The optical component is concerned with producing a reduced inverted image on the retina. The eye's optical system consists of not only two but four surfaces—two on the cornea, two on the lens. Rays are refracted toward the midline. Distant rays, due to their parallel nature, converge to a point on the retina. The cornea admits light at the greatest angle. The aqueous and vitreous humors both have a refractive index of 1.336-1.339, whereas the cornea has a refractive index of 1.376. Because the change in refractive index between cornea and aqueous humor is relatively small compared to the change at the air–cornea interface, it has a negligible refractive effect, typically -6 dioptres.[9] The cornea is considered to be a positive meniscus lens.[18]
Keeping the cornea transparent
Upon death or removal of an eye the cornea absorbs the aqueous humor, thickens, and becomes hazy. Transparency can be restored by putting it in a warm, well-ventilated chamber at 31 °C (88 °F, the normal temperature), allowing the fluid to leave the cornea and become transparent. The cornea takes in fluid from the aqueous humor and the small blood vessels of the limbus, but a pump ejects the fluid immediately upon entry. When energy is deficient the pump may fail, or works too slowly to compensate, causing swelling. This could arise at death, but a dead eye can be placed in a warm chamber and the reservoirs of sugar and glycogen can keep the cornea transparent for at least 24 hours. The endothelium controls this pumping action, and as discussed above, damage thereof is more serious, and is a cause of opaqueness and swelling. When damage to the cornea occurs, such as in a viral infection, the collagen used to repair the process is not regularly arranged, leading to an opaque patch (leukoma). When a cornea is needed for transplant, as from an eye bank, the best procedure is to remove the cornea from the eyeball, preventing the cornea from absorbing the aqueous humor.[9]
Diseases and disorders
The most common corneal disorders are the following:
- Corneal abrasion - a medical condition involving the loss of the surface epithelial layer of the eye's cornea as a result of trauma to the surface of the eye.
- Corneal dystrophy - a condition in which one or more parts of the cornea lose their normal clarity due to a buildup of cloudy material.
- Corneal ulcer - an inflammatory or infective condition of the cornea involving disruption of its epithelial layer with involvement of the corneal stroma.
- Corneal neovascularization - excessive ingrowth of blood vessels from the limbal vascular plexus into the cornea, caused by deprivation of oxygen from the air.
- Fuchs' dystrophy - cloudy morning vision.
- Keratitis - inflammation of the cornea.
- Keratoconus - a degenerative disease, the cornea thins and changes shape to be more like a cone.
Treatment and management
Surgical procedures
Various refractive eye surgery techniques change the shape of the cornea in order to reduce the need for corrective lenses or otherwise improve the refractive state of the eye. In many of the techniques used today, reshaping of the cornea is performed by photoablation using the excimer laser.
If the corneal stroma develops visually significant opacity, irregularity, or edema, a cornea of a deceased donor can be transplanted. Because there are no blood vessels in the cornea, there are also few problems with rejection of the new cornea.
There are also synthetic corneas (keratoprostheses) in development. Most are merely plastic inserts, but there are also those composed of biocompatible synthetic materials that encourage tissue ingrowth into the synthetic cornea, thereby promoting biointegration. Other methods, such as magnetic deformable membranes[19] and optically coherent transcranial magnetic stimulation of the human retina[20] are still in very early stages of research.
Non-surgical procedures
Orthokeratology is a method using specialized hard or rigid gas-permeable contact lenses to transiently reshape the cornea in order to improve the refractive state of the eye or reduce the need for eyeglasses and contact lenses.
In 2009, researchers at the University of Pittsburgh Medical center demonstrated that Stem cell collected from human corneas can restore transparency without provoking a rejection response in mice with corneal damage.[21] For corneal epithelial diseases such as Stevens Johnson Syndrome, Persistent corneal ulcer etc., the autologous contralateral (normal) suprabasal limbus derived in vitro expanded corneal limbal stem cells are found to be effective[22] as Amniotic membrane based expansion is controversial.[23] For endothelial diseases, such as bullous keratopathy, cadaver corneal endothelial precursor cells have been proven to be efficient. Recently emerging tissue engineering technologies are expected to be capable of making one cadaver-donor's corneal cells be expanded and be usable in more than one patient's eye.[24][25]
See also
- Corneal pachymetry
- Corneal reflex
- Corneal tattooing
- Corneal topography
- Eye disease
- List of keratins expressed in the human integumentary system
References
- ↑ Cassin, B.; Solomon, S. (1990). Dictionary of Eye Terminology. Gainesville, Florida: Triad Publishing Company.
- ↑ Goldstein, E. Bruce (2007). Sensation & Perception (7th ed.). Canada: Thompson Wadsworth.
- ↑ Najjar, Dany. "Clinical optics and refraction". Archived from the original on 2008-03-23.
- ↑ "Why does the cornea need oxygen?". The Association of Contact Lens Manufacturers.
- ↑ Nees, David W.; Fariss, Robert N.; Piatigorsky, Joram (2003). "Serum Albumin in Mammalian Cornea: Implications for Clinical Application". Investigative Ophthalmology & Visual Science. 44 (8): 3339–45. doi:10.1167/iovs.02-1161. PMID 12882779.
- ↑ Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia: Holt-Saunders International. pp. 461–2. ISBN 0-03-910284-X.
- ↑ https://www.sciencedaily.com/releases/2013/06/130611084216.htm
- 1 2 Merindano Encina, María Dolores; Potau, J. M.; Ruano, D.; Costa, J.; Canals, M. (2002). "A comparative study of Bowman's layer in some mammals Relationships with other constituent corneal structures". European Journal of Anatomy. 6 (3): 133–40.
- 1 2 3 4 5 6 "eye, human."Encyclopædia Britannica from Encyclopædia Britannica 2006 Ultimate Reference Suite DVD 2009
- ↑ Hayashi, Shuichiro; Osawa, Tokuji; Tohyama, Koujiro (2002). "Comparative observations on corneas, with special reference to bowman's layer and descemet's membrane in mammals and amphibians". Journal of Morphology. 254 (3): 247–58. doi:10.1002/jmor.10030. PMID 12386895.
- ↑ Maurice, 1957
- ↑ Dua, Harminder S.; Faraj, Lana A.; Said, Dalia G.; Gray, Trevor; Lowe, James (2013). "Human Corneal Anatomy Redefined". Ophthalmology. 120 (9): 1778–85. doi:10.1016/j.ophtha.2013.01.018. PMID 23714320.
- 1 2 Yanoff, Myron; Cameron, Douglas (2012). "Diseases of the Visual System". In Goldman, Lee; Schafer, Andrew I. Goldman's Cecil Medicine (24th ed.). Elsevier Health Sciences. pp. 2426–42. ISBN 978-1-4377-1604-7.
- ↑ Belmonte, Carlos; Gallar Juana (1996). "6: Corneal Nociceptors". Neurobiology of Nociceptors. Oxford University Press. p. 146. ISBN 9780198523345. Retrieved 19 February 2013.
- ↑ Karmel, Miriam. "Addressing the Pain of Corneal Neuropathy". EyeNet. American Academy of Ophthalmology. Retrieved 19 February 2013.
- ↑ Yu, C. Q.; Rosenblatt, M. I. (2007). "Transgenic Corneal Neurofluorescence in Mice: A New Model for in Vivo Investigation of Nerve Structure and Regeneration". Investigative Ophthalmology & Visual Science. 48 (4): 1535–42. doi:10.1167/iovs.06-1192. PMID 17389482.
- ↑ He, Jiucheng; Bazan, Nicolas G.; Bazan, Haydee E.P. (2010). "Mapping the entire human corneal nerve architecture". Experimental Eye Research. 91 (4): 513–23. doi:10.1016/j.exer.2010.07.007. PMC 2939211
 . PMID 20650270.
. PMID 20650270. - ↑ Herman, Irving P. (2007). Physics of the human body with 135 tables. Berlin: Springer. p. 642. ISBN 3540296042.
- ↑ Jones, Steven M.; Balderas-Mata, Sandra E.; Maliszewska, Sylwia M.; Olivier, Scot S.; Werner, John S. (2011). "Performance of 97-elements ALPAO membrane magnetic deformable mirror in Adaptive Optics - Optical Coherence Tomography system for in vivo imaging of human retina". Photonics Letters of Poland. 3 (4): 147–9.
- ↑ Richter, Lars; Bruder, Ralf; Schlaefer, Alexander; Schweikard, Achim (2010). "Towards direct head navigation for robot-guided Transcranial Magnetic Stimulation using 3D laserscans: Idea, setup and feasibility". 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology. pp. 2283–86. doi:10.1109/IEMBS.2010.5627660. ISBN 978-1-4244-4123-5.
- ↑ Du, Yiqin; Carlson, Eric C.; Funderburgh, Martha L.; Birk, David E.; Pearlman, Eric; Guo, Naxin; Kao, Winston W.-Y.; Funderburgh, James L. (2009). "Stem Cell Therapy Restores Transparency to Defective Murine Corneas". Stem Cells. 27 (7): 1635–42. doi:10.1002/stem.91. PMC 2877374
 . PMID 19544455. Lay summary – Medical News Today (13 April 2009).
. PMID 19544455. Lay summary – Medical News Today (13 April 2009). - ↑ Sitalakshmi, G.; Sudha, B.; Madhavan, H.N.; Vinay, S.; Krishnakumar, S.; Mori, Yuichi; Yoshioka, Hiroshi; Abraham, Samuel (2009). "Ex Vivo Cultivation of Corneal Limbal Epithelial Cells in a Thermoreversible Polymer (Mebiol Gel) and Their Transplantation in Rabbits: An Animal Model". Tissue Engineering Part A. 15 (2): 407–15. doi:10.1089/ten.tea.2008.0041. PMID 18724830.
- ↑ Schwab, Ivan R.; Johnson, NT; Harkin, DG (2006). "Inherent Risks Associated with Manufacture of Bioengineered Ocular Surface Tissue". Archives of Ophthalmology. 124 (12): 1734–40. doi:10.1001/archopht.124.12.1734. PMID 17159033.
- ↑ Hitani, K; Yokoo, S; Honda, N; Usui, T; Yamagami, S; Amano, S (2008). "Transplantation of a sheet of human corneal endothelial cell in a rabbit model". Molecular vision. 14: 1–9. PMC 2267690
 . PMID 18246029.
. PMID 18246029. - ↑ Parikumar, Periyasamy; Haraguchi, Kazutoshi; Ohbayashi, Akira; Senthilkumar, Rajappa; Abraham, Samuel J. K. (2014). "Successful Transplantation of In Vitro Expanded Human Cadaver Corneal Endothelial Precursor Cells On to a Cadaver Bovine's Eye Using a Nanocomposite Gel Sheet". Current Eye Research. 39 (5): 522–6. doi:10.3109/02713683.2013.838633. PMID 24144454.
General references
- Daxer, Albert; Misof, Klaus; Grabner, Barbara; Ettl, Armin; Fratzl, Peter (1998). "Collagen fibrils in the human corneal stroma: Structure and aging". Investigative Ophthalmology & Visual Science. 39 (3): 644–8. PMID 9501878.
- Daxer, Albert; Fratzl, Peter (1997). "Collagen fibril orientation in the human corneal stroma and its implication in keratoconus". Investigative Ophthalmology & Visual Science. 38 (1): 121–9. PMID 9008637.
- Fratzl, Peter; Daxer, Albert (1993). "Structural transformation of collagen fibrils in corneal stroma during drying. An x-ray scattering study". Biophysical Journal. 64 (4): 1210–4. doi:10.1016/S0006-3495(93)81487-5. PMC 1262438
 . PMID 8494978.
. PMID 8494978.
External links
| Wikimedia Commons has media related to Cornea. |
| Wikimedia Commons has media related to Anatomy of the human eye. |
- Atlas image: eye_1 at the University of Michigan Health System - "Sagittal Section Through the Eyeball"
- Facts About The Cornea and Corneal Disease National Eye Institute (NEI)