Haemophilia A
| Haemophilia A | |
|---|---|
|
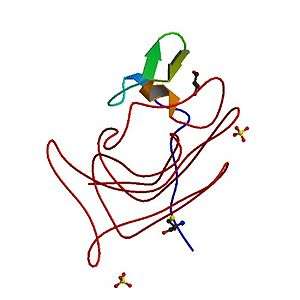
Deficiency in coagulation factor VIII is the cause of haemophilia A. | |
| Classification and external resources | |
| Specialty | Hematology |
| ICD-10 | D66 |
| ICD-9-CM | 286.0 |
| OMIM | 306700 |
| DiseasesDB | 5555 |
| MedlinePlus | 000538 |
| eMedicine | emerg/239 |
| Patient UK | Haemophilia A |
Haemophilia A is a genetic deficiency in clotting factor VIII, which causes increased bleeding and usually affects males. In the majority of cases it is inherited as an X-linked recessive trait, though there are cases which arise from spontaneous mutations.[1][2]
Signs and symptoms
In terms of the symptoms of Hemophilia A there are internal or external bleeding episodes. Individuals with more severe haemophilia suffer more severe and more frequent bleeding, while others with mild haemophilia typically suffer more minor symptoms except after surgery or serious trauma. Moderate haemophiliacs have variable symptoms which manifest along a spectrum between severe and mild forms.[3]
Prolonged bleeding from a venepuncture or heelprick is another common early sign of haemophilia, these signs may lead to blood tests which indicates haemophilia.[4] In other people, especially those with moderate or mild haemophilia any trauma will lead to the first serious bleed.Haemophilia leads to a severely increased risk of prolonged bleeding from common injuries, or in severe cases bleeding may be spontaneous and without obvious cause. Bleeding may occur anywhere in the body, superficial bleeding such as those caused by abrasions, or shallow lacerations may be prolonged and the scab may easily be broken up due to the lack of fibrin, which may cause re-bleeding.[3] While superficial bleeding is troublesome, some of the more serious sites of bleeding are:[5]
Muscle and joint haemorrhages - or haemarthrosis - are indicative of haemophilia,[6] while digestive tract and cerebral haemorrhages are also germane to other coagulation disorders.Though typically not life-threatening, joint bleeding is one of the most serious symptoms of haemophilia. Repeated bleeds into a joint capsule can cause permanent joint damage and disfigurement resulting in chronic arthritis and disability. Joint damage is not a result of blood in the capsule but rather the healing process. When blood in the joint is broken down by enzymes in the body, the bone in that area is also degraded, this exerts a lot of pain upon the person afflicted with the disease.
Genetics

Haemophilia A is inherited as an X-linked recessive trait, and occurs in males and in homozygous females (only possible in the offspring of a carrier female and a hemophilic male[7]). However, mild haemophilia A is known to occur in heterozygous females due to X-inactivation, so it is recommended that levels of factor VIII and IX be measured in all known/potential carriers prior to surgery and in the event of clinically significant bleeding.[3][8]
About 5-10% of people with haemophilia A are affected because they make a dysfunctional version of the factor VIII protein, while the remainder are affected because they produced factor VIII in insufficient amounts (quantitative deficiency).[8] Of those who have severe deficiency (defined as <1% activity of factor VIII), 45-50% have the same mutation, an inversion within the factor VIII gene that results in total elimination of protein production.[8]
Since both forms of haemophilia can be caused by a variety of different mutations, initial diagnosis and classification is done by measurement of protein activity rather than by genetic tests, though genetic tests are recommended for testing of family members once a known case of haemophilia is identified.[3][8] Approximately 30% of patients have no family history; their disease is presumably caused by new mutations.[9]
Diagnosis


The diagnosis of hemophilia A may be suspected as coagulation testing reveals an increased PTT in the context of a normal PT and bleeding time. PTT tests are the first blood test done when haemophilia is indicated.[10] However, the diagnosis is made in the presence of very low levels of Factor VIII.A family history is frequently present, although not essential. Recently, genetic testing has been made available to determine an individual's risk of attaining or passing on hemophilia.Diagnosis of haemophilia A also includes a severity level which can range from mild to severe based on the amount of active and functioning factor VIII detected in the blood. Factor VIII levels do not typically change throughout an individual's life. Severe haemophilia A is the most common form occurring in the majority of affected people. Individuals with mild haemophilia often experience few or no bleeding episodes except in the case of serious trauma (i.e. tooth extraction, or surgery).[3]
Severity
There are numerous different mutations which cause haemophilia A, due to differences in changes to the gene involved (and the resulting protein), individuals with haemophilia often have some level of active clotting factor. Individuals with less than 1% active factor are classified as having severe haemophilia, those with 1–5% active factor have moderate haemophilia, and those with mild haemophilia have between 5–40% of normal levels of active clotting factor.[11]
Differential diagnosis
Two of the most common differential diagnoses are haemophilia B which is a deficiency in Factor IX and von Willebrand Disease which is a deficiency in von Willebrand factor (needed for the proper functioning of Factor VIII[12]), haemophilia C is also a possible, differential diagnosis.[2]
Treatment

In regards to the treatment of this genetic disorder, most individuals with severe haemophilia require regular supplementation with intravenous recombinant or plasma concentrate Factor VIII. The prophylactic treatment regime is highly variable and individually determined.[5] In children, an easily accessible intravenous port ( portacath) [13] may have to be inserted to minimise frequent traumatic intravenous cannulation. These devices have made prophylaxis in haemophilia much easier for families because the problems of finding a vein for infusion several times a week are eliminated. However, there are risks involved with their use, the most worrisome being that of infection,studies differ but some show an infection rate that is high[14] These infections can usually be treated with intravenous antibiotics but sometimes the device must be removed,[15] also, there are other studies that show a risk of clots forming at the tip of the catheter.Some individuals with severe haemophilia and most with moderate and mild haemophilia treat only as needed without a regular prophylactic schedule.[16] Mild haemophiliacs often manage their condition with desmopressin, which releases stored factor VIII from blood vessel walls.[17]
Complications
One therapeutic conundrum is the development of inhibitor antibodies against factor VIII due to frequent infusions. These develop as the body recognises the "normal form" factor VIII as foreign, as the body does not have its own copy. The problem is that in these individuals, factor VIII infusions are ineffective. Recently activated factor VII has become available as a treatment for haemorrhage in individuals with haemophilia and factor inhibitors[3][18]
Prognosis
Two Dutch studies have followed hemophilia patients for a number of years.[19][20] Both studies found that viral infections were common in hemophiliacs due to the frequent blood transfusions which put them at risk of getting blood borne infections such as HIV and hepatitis C. In the latest study which followed patients from 1992 to 2001, the male life expectancy was 59 years. If cases with known viral infections were excluded, the life expectancy was 72, close to that of the general population. 26% of the cases died from AIDS and 22% from hepatitis C.[20]
Epidemiology
Haemophilia A occurs in approximately 1 in 5,000 males,[8] while the incidence of haemophilia B is 1 in 30,000 in male population,[8] of these, 85% have haemophilia A and 15% have hemophilia B.[8]
See also
References
- ↑ "Hemophilia A: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 24 June 2016.
- 1 2 "Haemophilia A (Factor VIII Deficiency) information | Patient". Patient. Retrieved 24 June 2016.
- 1 2 3 4 5 6 Konkle, Barbara A.; Josephson, Neil C.; Nakaya Fletcher, Shelley (1993-01-01). Pagon, Roberta A.; Adam, Margaret P.; Ardinger, Holly H.; Wallace, Stephanie E.; Amemiya, Anne; Bean, Lora JH; Bird, Thomas D.; Fong, Chin-To; Mefford, Heather C., eds. Hemophilia A. Seattle (WA): University of Washington, Seattle. PMID 20301578.update 2014
- ↑ Lissauer, Tom; Fanaroff, Avroy A.; Miall, Lawrence; Fanaroff, Jonathan (2015-06-10). Neonatology at a Glance. John Wiley & Sons. p. 135. ISBN 9781118767429.
- 1 2 "How Is Hemophilia Treated? - NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 2016-07-08.
- ↑ "Management of Joint Bleeding in Hemophilia: Management of Acute Hemarthrosis". Medscape. Medscape.org. Retrieved 1 August 2016.
- ↑ Nair, Preethi S.; Shetty, S.; Ghosh, Kanjaksha (2012-01-01). "A homozygous female hemophilia A". Indian Journal of Human Genetics. 18 (1): 134–136. doi:10.4103/0971-6866.96685. ISSN 0971-6866. PMC 3385172
 . PMID 22754241.
. PMID 22754241. - 1 2 3 4 5 6 7 Kliegman, Robert (2011). Nelson textbook of pediatrics. (19th ed.). Philadelphia: Saunders. pp. 1700–1. ISBN 978-1-4377-0755-7.
- ↑ Bowen, D J (2002). "Haemophilia A and haemophilia B: molecular insights". Molecular Pathology. 55 (1): 1–18. doi:10.1136/mp.55.1.1. PMC 1187139
 . PMID 11836440.
. PMID 11836440. - ↑ "OMIM Entry - # 306700 - HEMOPHILIA A; HEMA". omim.org. Retrieved 2016-07-08.
- ↑ Hemophilia A at eMedicine
- ↑ "Von Willebrand's Disease. About Von Willebrand's Disease | Patient". Patient. Retrieved 2016-07-08.
- ↑ Ma, Alice D.; Roberts, Harold R.; Escobar, Miguel A. (2012-10-03). Hemophilia and Hemostasis: A Case-Based Approach to Management. John Wiley & Sons. ISBN 9781118439302.Google books no page
- ↑ Santagostino, Elena; Mancuso, Maria Elisa (2008-09-01). "Barriers to primary prophylaxis in haemophilic children: the issue of the venous access". Blood Transfusion. 6 (Suppl 2): s12–s16. doi:10.2450/2008.0031-08. ISSN 1723-2007. PMC 2652218
 . PMID 19105504.
. PMID 19105504. - ↑ "Guidelines for the Prevention of Intravascular Catheter-Related Infections". www.cdc.gov. Retrieved 8 July 2016.
- ↑ Ljung, Rolf (2007-09-01). "The risk associated with indwelling catheters in children with haemophilia". British Journal of Haematology. 138 (5): 580–586. doi:10.1111/j.1365-2141.2007.06703.x. ISSN 1365-2141.
- ↑ Franchini, Massimo; Lippi, Giuseppe (2011-10-01). "The use of desmopressin in acquired haemophilia A: a systematic review". Blood Transfusion. 9 (4): 377–382. doi:10.2450/2011.0113-10. ISSN 1723-2007. PMC 3200405
 . PMID 21839010.
. PMID 21839010. - ↑ Ma, Alice D.; Carrizosa, Daniel (2006-01-01). "Acquired Factor VIII Inhibitors: Pathophysiology and Treatment". ASH Education Program Book. 2006 (1): 432–437. doi:10.1182/asheducation-2006.1.432. ISSN 1520-4391. PMID 17124095.
- ↑ Triemstra, Mattanja (1995-12-01). "Mortality in Patients with Hemophilia: Changes in a Dutch Population from 1986 to 1992 and 1973 to 1986". Annals of Internal Medicine. 123 (11). doi:10.7326/0003-4819-123-11-199512010-00002. ISSN 0003-4819.
- 1 2 Plug, I.; Van Der Bom, J. G.; Peters, M.; Mauser-Bunschoten, E. P.; De Goede-Bolder, A.; Heijnen, L.; Smit, C.; Willemse, J.; Rosendaal, F. R. (2006-03-01). "Mortality and causes of death in patients with hemophilia, 1992–2001: a prospective cohort study1". Journal of Thrombosis and Haemostasis. 4 (3): 510–516. doi:10.1111/j.1538-7836.2006.01808.x. ISSN 1538-7836.
Further reading
- Casana, P.; Cabrera, N.; Cid, A. R.; Haya, S.; Beneyto, M.; Espinos, C.; Cortina, V.; Dasi, M. A.; Aznar, J. A. (2008-07-01). "Severe and moderate hemophilia A: identification of 38 new genetic alterations". Haematologica. 93 (7): 1091–1094. doi:10.3324/haematol.12344. ISSN 0390-6078.
- Roberts, Harold R. Haemophilia and Haemostasis: A Case-based Approach to Management. John Wiley & Sons. ISBN 9780470766439. Retrieved 8 July 2016.
- Collins, Peter; Baudo, Francesco; Huth-Kühne, Angela; Ingerslev, Jørgen; Kessler, Craig M; Castellano, Maria E Mingot; Shima, Midori; St-Louis, Jean; Lévesque, Hervé (7 June 2010). "Consensus recommendations for the diagnosis and treatment of acquired hemophilia A". BMC Research Notes. 3: 161. doi:10.1186/1756-0500-3-161. ISSN 1756-0500. PMC 2896368
 . PMID 20529258.
. PMID 20529258. - Coppola, Antonio; Windyga, Jerzy; Tufano, Antonella; Yeung, Cindy; Di Minno, Matteo Nicola Dario (9 February 2015). "Treatment for preventing bleeding in people with haemophilia or other congenital bleeding disorders undergoing surgery". Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd. doi:10.1002/14651858.cd009961.pub2. Retrieved 12 July 2016.