Bipolar disorder
| Bipolar disorder | |
|---|---|
| bipolar affective disorder, bipolar illness, manic depression, bipolar disease[1] | |
|
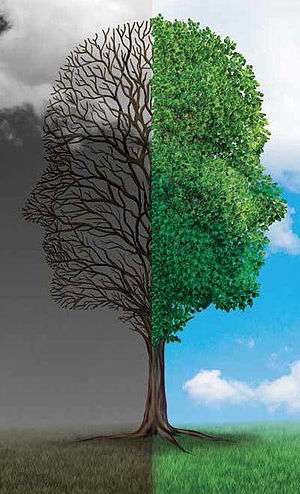
Bipolar disorder is characterized by episodes of depression and mania. | |
| Classification and external resources | |
| Specialty | Psychiatry |
| ICD-10 | F31 |
| ICD-9-CM | 296.0, 296.1, 296.4, 296.5, 296.6, 296.7, 296.8 |
| OMIM | 125480 309200 |
| DiseasesDB | 7812 |
| MedlinePlus | 000926 |
| eMedicine | med/229 |
| Patient UK | Bipolar disorder |
| MeSH | D001714 |
Bipolar disorder, also known as manic depression, is a mental disorder with periods of depression and periods of elevated mood.[2][3] The elevated mood is significant and is known as mania or hypomania, depending on its severity, or whether symptoms of psychosis are present. During mania an individual behaves or feels abnormally energetic, happy or irritable.[2] Individuals often make poorly thought out decisions with little regard to the consequences. The need for sleep is usually reduced during manic phases.[3] During periods of depression there may be crying, a negative outlook on life, and poor eye contact with others.[2] The risk of suicide among those with the illness is high at greater than 6 percent over 20 years, while self-harm occurs in 30–40 percent.[2] Other mental health issues such as anxiety disorders and substance use disorder are commonly associated.[2]
The causes are not clearly understood, but both environmental and genetic factors play a role.[2] Many genes of small effect, contribute to risk.[2][4] Environmental factors include a history of childhood abuse and long-term stress.[2] It is divided into bipolar I disorder if there is at least one manic episode and bipolar II disorder if there are at least one hypomanic episode and one major depressive episode. In those with less severe symptoms of a prolonged duration the condition cyclothymic disorder may be present. If due to drugs or medical problems it is classified separately.[3] Other conditions that may present in a similar manner include attention deficit hyperactivity disorder, personality disorders, schizophrenia and substance use disorder as well as a number of medical conditions.[2] Medical testing is not required for a diagnosis. However, blood tests or medical imaging can be done to rule out other problems.[5]
Treatment commonly includes psychotherapy, as well as medications such as mood stabilizers and antipsychotics. Examples of mood stabilizers that are commonly used include lithium and anticonvulsants. Treatment in hospital against a person's consent may be required at times as people may be a risk to themselves or others yet refuse treatment. Severe behavioral problems may be managed with short term antipsychotics or benzodiazepines. In periods of mania it is recommended that antidepressants be stopped. If antidepressants are used for periods of depression they should be used with a mood stabilizer. Electroconvulsive therapy (ECT) may be helpful for those who do not respond to other treatments. If treatments are stopped, it is recommended that this be done slowly. Many individuals have financial, social or work-related problems due to the illness. These difficulties occur a quarter to a third of the time on average. The risk of death from natural causes such as heart disease is twice that of the general population. This is due to poor lifestyle choices and the side effects from medications.[2]
About 3 percent of people in the US are estimated to have bipolar disorder at some point in their life.[6] Lower rates of around 1 percent are found in other countries. The most common age at which symptoms begin is 25.[2] Rates appear to be similar in females as males.[7] The economic costs of the disorder has been estimated at $45 billion for the United States in 1991.[8] A large proportion of this was related to a higher number of missed work days, estimated at 50 per year.[8] People with bipolar disorder often face problems with social stigma.[2]
Signs and symptoms
.jpg)
Mania is the defining feature of bipolar disorder,[9] and can occur with different levels of severity. With milder levels of mania, known as hypomania, individuals appear energetic, excitable, and may be highly productive.[10] As mania worsens, individuals begin to exhibit erratic and impulsive behavior, often making poor decisions due to unrealistic ideas about the future, and sleep very little.[10] At the most severe level, manic individuals can experience distorted or delusional beliefs about the universe known as psychosis.[10] A depressive episode commonly follows an episode of mania.[10] The biological mechanisms responsible for switching from a manic or hypomanic episode to a depressive episode or vice versa remain poorly understood.[11]
Manic episodes

Mania is a distinct period of at least one week of elevated or irritable mood, which can take the form of euphoria, and exhibit three or more of the following behaviors (four if irritable): speak in a rapid, uninterruptible manner, are easily distracted, have racing thoughts, display an increase in goal-oriented activities or feel agitated, or exhibit behaviors characterized as impulsive or high-risk such as hypersexuality or excessive money spending.[9] To meet the definition for a manic episode, these behaviors must impair the individual's ability to socialize or work.[9][10] If untreated, a manic episode usually lasts three to six months.[12]
People with mania may also experience a decreased need for sleep, speak excessively in addition to speaking rapidly, and may have impaired judgment.[10][13] Manic individuals often have issues with substance abuse due to a combination of thrill-seeking and poor judgment.[14] At more extreme levels, a person in a manic state can experience psychosis, or a break with reality, a state in which thinking is affected along with mood.[10] They may feel out of control or unstoppable, or as if they have been "chosen" and are on a special mission, or have other grandiose or delusional ideas.[15] Approximately 50 percent of those with bipolar disorder experience delusions or hallucinations.[16] This may lead to violent behaviors and hospitalization in an inpatient psychiatric hospital.[10][13] The severity of manic symptoms can be measured by rating scales such as the Young Mania Rating Scale.[13][17]
The onset of a manic (or depressive) episode is often foreshadowed by sleep disturbances.[18] Mood changes, psychomotor and appetite changes, and an increase in anxiety can also occur up to three weeks before a manic episode develops.[19]
Hypomanic episodes
Hypomania is a milder form of mania defined as at least four days of the same criteria as mania,[10] but does not cause a significant decrease in the individual's ability to socialize or work, lacks psychotic features—such as delusions or hallucinations—and does not require psychiatric hospitalization.[9] Overall functioning may actually increase during episodes of hypomania and is thought to serve as a defense mechanism against depression.[20] Hypomanic episodes rarely progress to true manic episodes.[20] Some hypomanic people show increased creativity[10] while others are irritable or demonstrate poor judgment. Hypomanic people generally have increased energy and increased activity levels.
Hypomania may feel good to the person who experiences it.[10] Thus, even when family and friends recognize mood swings, the individual will often deny that anything is wrong.[21] What might be called a "hypomanic event", if not accompanied by depressive episodes, is often not deemed as problematic, unless the mood changes are uncontrollable, volatile or mercurial.[20] Most commonly, symptoms continue for a few weeks to a few months.[22]
Depressive episodes

Signs and symptoms of the depressive phase of bipolar disorder include persistent feelings of sadness, irritability or anger, loss of interest in previously enjoyable activities, excessive or inappropriate guilt, hopelessness, sleeping too much or not enough, changes in appetite and/or weight, fatigue, problems concentrating, self-loathing or feelings of worthlessness, and thoughts of death or suicidal ideation.[23] In severe cases, the individual may develop symptoms of psychosis, a condition also known as severe bipolar disorder with psychotic features. These symptoms include delusions and hallucinations. A major depressive episode persists for at least two weeks, and may continue for over six months if left untreated.[24]
The earlier the age of onset, the more likely the first few episodes are to be depressive.[25] Because a bipolar diagnosis requires a manic or hypomanic episode, many patients are initially diagnosed and treated as having major depression.[26]
Mixed affective episodes
In the context of bipolar disorder, a mixed state is a condition during which symptoms of both mania and depression occur at the same time.[27] Individuals experiencing a mixed state may have manic symptoms such as grandiose thoughts while at the same time experiencing depressive symptoms such as excessive guilt or feeling suicidal.[27] Mixed states are considered to be high-risk for suicidal behavior since depressive emotions such as hopelessness are often paired with mood swings or difficulties with impulse control.[27] Anxiety disorder occurs more frequently as a comorbidity in mixed bipolar episodes than in non mixed bipolar depression or mania.[27] Substance abuse (including alcohol) also follows this trend.[27]
Associated features
Associated features are clinical phenomena that often accompany the disorder but are not part of the diagnostic criteria. In adults with the condition, bipolar disorder is often accompanied by changes in cognitive processes and abilities. These include reduced attentional and executive capabilities and impaired memory. How the individual processes the universe also depends on the phase of the disorder, with differential characteristics between the manic, hypomanic and depressive states.[19] Some studies have found a significant association between bipolar disorder and creativity.[28] Those with bipolar disorder may have difficulty in maintaining relationships.[29] There are several common childhood precursors seen in children who later receive a diagnosis of bipolar disorder; these disorders include mood abnormalities, full major depressive episodes, and attention deficit hyperactivity disorder (ADHD).[30]
Comorbid conditions
The diagnosis of bipolar disorder can be complicated by coexisting (comorbid) psychiatric conditions including the following: obsessive-compulsive disorder, substance abuse, eating disorders, attention deficit hyperactivity disorder, social phobia, premenstrual syndrome (including premenstrual dysphoric disorder), or panic disorder.[14][16][23][31] A careful longitudinal analysis of symptoms and episodes, enriched if possible by discussions with friends and family members, is crucial to establishing a treatment plan where these comorbidities exist.[32]
Causes
The causes of bipolar disorder likely vary between individuals and the exact mechanism underlying the disorder remains unclear.[33] Genetic influences are believed to account for 60–80 percent of the risk of developing the disorder indicating a strong hereditary component.[16] The overall heritability of the bipolar spectrum has been estimated at 0.71.[34] Twin studies have been limited by relatively small sample sizes but have indicated a substantial genetic contribution, as well as environmental influence. For bipolar disorder type I, the (probandwise) concordance rates in modern studies have been consistently estimated at around 40 percent in identical twins (same genes), compared to about 5 percent in fraternal twins.[9][35] A combination of bipolar I, II and cyclothymia produced concordance rates of 42 percent vs. 11 percent, with a relatively lower ratio for bipolar II that likely reflects heterogeneity. There is overlap with unipolar depression and if this is also counted in the co-twin the concordance with bipolar disorder rises to 67 percent in monozygotic twins and 19 percent in dizygotic.[36] The relatively low concordance between dizygotic twins brought up together suggests that shared family environmental effects are limited, although the ability to detect them has been limited by small sample sizes.[34]
Genetic
Genetic studies have suggested that many chromosomal regions and candidate genes are related to bipolar disorder susceptibility with each gene exerting a mild to moderate effect.[16] The risk of bipolar disorder is nearly ten-fold higher in first degree-relatives of those affected with bipolar disorder when compared to the general population; similarly, the risk of major depressive disorder is three times higher in relatives of those with bipolar disorder when compared to the general population.[9]
Although the first genetic linkage finding for mania was in 1969,[37] the linkage studies have been inconsistent.[9] The largest and most recent genome-wide association study failed to find any particular locus that exerts a large effect reinforcing the idea that no single gene is responsible for bipolar disorder in most cases.[38]
Findings point strongly to heterogeneity, with different genes being implicated in different families.[39] Robust and replicable genome-wide significant associations showed several common single nucleotide polymorphisms, including variants within the genes CACNA1C, ODZ4, and NCAN.[16][38]
Advanced paternal age has been linked to a somewhat increased chance of bipolar disorder in offspring, consistent with a hypothesis of increased new genetic mutations.[40]
Physiological

Abnormalities in the structure and/or function of certain brain circuits could underlie bipolar. Meta-analyses of structural MRI studies in bipolar disorder report an increase in the volume of the lateral ventricles, globus pallidus and increase in the rates of deep white matter hyperintensities.[41][42][43] Functional MRI findings suggest that abnormal modulation between ventral prefrontal and limbic regions, especially the amygdala, are likely contribute to poor emotional regulation and mood symptoms.[44]
According to the "kindling" hypothesis, when people who are genetically predisposed toward bipolar disorder experience stressful events, the stress threshold at which mood changes occur becomes progressively lower, until the episodes eventually start (and recur) spontaneously. There is evidence supporting an association between early-life stress and dysfunction of the hypothalamic-pituitary-adrenal axis (HPA axis) leading to its over activation, which may play a role in the pathogenesis of bipolar disorder.[45][46]
Other brain components which have been proposed to play a role are the mitochondria[33] and a sodium ATPase pump.[47] Circadian rhythms and melatonin activity also seem to be altered.[48]
Environmental
Evidence suggests that environmental factors play a significant role in the development and course of bipolar disorder, and that individual psychosocial variables may interact with genetic dispositions.[49] There is fairly consistent evidence from prospective studies that recent life events and interpersonal relationships contribute to the likelihood of onsets and recurrences of bipolar mood episodes, as they do for onsets and recurrences of unipolar depression.[50] There have been repeated findings that 30–50 percent of adults diagnosed with bipolar disorder report traumatic/abusive experiences in childhood, which is associated on average with earlier onset, a higher rate of suicide attempts, and more co-occurring disorders such as PTSD.[51] The total number of reported stressful events in childhood is higher in those with an adult diagnosis of bipolar spectrum disorder compared to those without, particularly events stemming from a harsh environment rather than from the child's own behavior.[52]
Neurological
Less commonly bipolar disorder, or a bipolar-like disorder, may occur as a result of or in association with a neurological condition or injury. Such conditions and injuries include (but are not limited to) stroke, traumatic brain injury, HIV infection, multiple sclerosis, porphyria, and rarely temporal lobe epilepsy.[53]
Neurochemical
Dopamine, a known neurotransmitter responsible for mood cycling, has been shown to have increased transmission during the manic phase.[11][54] The dopamine hypothesis states that the increase in dopamine results in secondary homeostatic down regulation of key systems and receptors such as an increase in dopamine mediated G protein-coupled receptors. This results in decreased dopamine transmission characteristic of the depressive phase.[11] The depressive phase ends with homeostatic up regulation potentially restarting the cycle over again.[55]
Glutamate is significantly increased within the left dorsolateral prefrontal cortex during the manic phase of bipolar disorder, and returns to normal levels once the phase is over.[56] The increase in GABA is possibly caused by a disturbance in early development causing a disturbance of cell migration and the formation of normal lamination, the layering of brain structures commonly associated with the cerebral cortex.[57]
Prevention
Attempts at prevention of bipolar disorder have focused on stress (such as childhood adversity or highly conflictual families) which, although not a diagnostically specific causal agent for bipolar, does place genetically and biologically vulnerable individuals at risk for a more pernicious course of illness.[58] There has been debate regarding the causal relationship between usage of cannabis and bipolar disorder.[59]
Diagnosis
Bipolar disorder is commonly diagnosed during adolescence or early adulthood, but onset can occur throughout the life cycle.[3][60] The disorder can be difficult to distinguish from unipolar depression and the average delay in diagnosis is 5–10 years after symptoms begin.[61] Diagnosis of bipolar disorder takes several factors into account and considers the self-reported experiences of the symptomatic individual, abnormal behavior reported by family members, friends or co-workers, observable signs of illness as assessed by a clinician, and often a medical work-up to rule-out medical causes. Assessment is usually done on an outpatient basis; admission to an inpatient facility is considered if there is a risk to oneself or others. The most widely used criteria for diagnosing bipolar disorder are from the American Psychiatric Association's (APA) Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and the World Health Organization's (WHO) International Statistical Classification of Diseases and Related Health Problems, 10th Edition (ICD-10). The ICD-10 criteria are used more often in clinical settings outside of the U.S. while the DSM criteria are used clinically within the U.S. and are the prevailing criteria used internationally in research studies. The DSM-5, published in 2013, included further and more accurate specifiers compared to its predecessor, the DSM-IV-TR.[62]
Several rating scales for the screening and evaluation of bipolar disorder exist,[63] including the Bipolar spectrum diagnostic scale, Mood Disorder Questionnaire, and the HCL-32.[64] The use of evaluation scales can not substitute a full clinical interview but they serve to systematize the recollection of symptoms.[64] On the other hand, instruments for screening bipolar disorder tend to have lower sensitivity.[63]
Differential diagnosis
There are several other mental disorders with symptoms similar to those seen in bipolar disorder. These disorders include schizophrenia, major depressive disorder,[65] attention deficit hyperactivity disorder (ADHD), and certain personality disorders, such as borderline personality disorder.[66][67][68]
Although there are no biological tests that are diagnostic of bipolar disorder,[38] blood tests and/or imaging may be carried out to exclude medical illnesses with clinical presentations similar to that of bipolar disorder such as hypothyroidism or hyperthyroidism, metabolic disturbance, a chronic disease, or an infection such as HIV or syphilis.[60] A review of current and recent medications and drug use is considered to rule out these causes; common medications that can cause manic symptoms include antidepressants, prednisone, Parkinson's disease medications, thyroid hormone, stimulants (including cocaine and methamphetamine), and certain antibiotics.[69] An EEG may be used to exclude neurological disorders such as epilepsy, and a CT scan or MRI of the head may be used to exclude brain lesions.[60] Additional testing is especially indicated when age of first onset is mid to late life.[3] Investigations are not generally repeated for a relapse unless there is a specific medical indication.
Bipolar spectrum
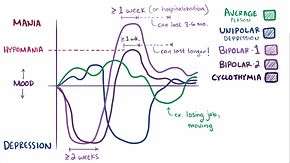
Bipolar spectrum disorders includes: bipolar I disorder, bipolar II disorder, cyclothymic disorder and cases where subthreshold symptoms are found to cause clinically significant impairment or distress.[3][60] These disorders involve major depressive episodes that alternate with manic or hypomanic episodes, or with mixed episodes that feature symptoms of both mood states.[3] The concept of the bipolar spectrum is similar to that of Emil Kraepelin's original concept of manic depressive illness.[70]
Unipolar hypomania without accompanying depression has been noted in the medical literature.[71] There is speculation as to whether this condition may occur with greater frequency in the general, untreated population; successful social function of these potentially high-achieving individuals may lead to being labeled as normal, rather than as individuals with substantial dysregulation.
Criteria and subtypes
The DSM and the ICD characterize bipolar disorder as a spectrum of disorders occurring on a continuum. The DSM-5 lists three specific subtypes:[3]
- Bipolar I disorder: At least one manic episode is necessary to make the diagnosis;[72] depressive episodes are common in the vast majority of cases with bipolar disorder I, but are unnecessary for the diagnosis.[9] Specifiers such as "mild, moderate, moderate-severe, severe" and "with psychotic features" should be added as applicable to indicate the presentation and course of the disorder.[3]
- Bipolar II disorder: No manic episodes and one or more hypomanic episodes and one or more major depressive episode.[72] Hypomanic episodes do not go to the full extremes of mania (i.e., do not usually cause severe social or occupational impairment, and are without psychosis), and this can make bipolar II more difficult to diagnose, since the hypomanic episodes may simply appear as periods of successful high productivity and are reported less frequently than a distressing, crippling depression.
- Cyclothymia: A history of hypomanic episodes with periods of depression that do not meet criteria for major depressive episodes.[73]
When relevant, specifiers for peripartum onset and with rapid cycling should be used with any subtype. Individuals who have subthreshold symptoms that cause clinically significant distress or impairment, but do not meet full criteria for one of the three subtypes may be diagnosed with other specified or unspecified bipolar disorder. Other specified bipolar disorder is used when a clinician chooses to provide an explanation for why the full criteria were not met (e.g., hypomania without a prior major depressive episode).[3]
Rapid cycling
Most people who meet criteria for bipolar disorder experience a number of episodes, on average 0.4 to 0.7 per year, lasting three to six months.[74] Rapid cycling, however, is a course specifier that may be applied to any of the above subtypes. It is defined as having four or more mood disturbance episodes within a one-year span and is found in a significant proportion of individuals with bipolar disorder.[23] These episodes are separated from each other by a remission (partial or full) for at least two months or a switch in mood polarity (i.e., from a depressive episode to a manic episode or vice versa).[9] The definition of rapid cycling most frequently cited in the literature (including the DSM) is that of Dunner and Fieve: at least four major depressive, manic, hypomanic or mixed episodes are required to have occurred during a 12-month period.[75] Ultra-rapid (days) and ultra-ultra rapid or ultradian (within a day) cycling have also been described.[76] The literature examining the pharmacological treatment of rapid cycling is sparse and there is no clear consensus with respect to its optimal pharmacological management.[77]
Management
There are a number of pharmacological and psychotherapeutic techniques used to treat bipolar disorder. Individuals may use self-help and pursue recovery.
Hospitalization may be required especially with the manic episodes present in bipolar I. This can be voluntary or (if mental health legislation allows and varying state-to-state regulations in the USA) involuntary (called civil or involuntary commitment). Long-term inpatient stays are now less common due to deinstitutionalization, although these can still occur.[78] Following (or in lieu of) a hospital admission, support services available can include drop-in centers, visits from members of a community mental health team or an Assertive Community Treatment team, supported employment and patient-led support groups, intensive outpatient programs. These are sometimes referred to as partial-inpatient programs.[79]
Psychosocial
Psychotherapy is aimed at alleviating core symptoms, recognizing episode triggers, reducing negative expressed emotion in relationships, recognizing prodromal symptoms before full-blown recurrence, and, practicing the factors that lead to maintenance of remission.[80][81][82] Cognitive behavioral therapy, family-focused therapy, and psychoeducation have the most evidence for efficacy in regard to relapse prevention, while interpersonal and social rhythm therapy and cognitive-behavioral therapy appear the most effective in regard to residual depressive symptoms. Most studies have been based only on bipolar I, however, and treatment during the acute phase can be a particular challenge.[83] Some clinicians emphasize the need to talk with individuals experiencing mania, to develop a therapeutic alliance in support of recovery.[84]
Medication

A number of medications are used to treat bipolar disorder.[50] The medication with the best evidence is lithium, which is effective in treating acute manic episodes and preventing relapses; lithium is also an effective treatment for bipolar depression.[85] Lithium reduces the risk of suicide, self-harm, and death in people with bipolar disorder.[86] It is unclear if ketamine is useful in bipolar as of 2015.[87]
Four anticonvulsants are used in the treatment of bipolar disorder. Carbamazepine effectively treats manic episodes, with some evidence it has greater benefit in rapid-cycling bipolar disorder, or those with more psychotic symptoms or a more schizoaffective clinical picture. It is less effective in preventing relapse than lithium or valproate.[88][89] Carbamazepine became a popular treatment option for bipolar in the late 1980s and early 1990s, but was displaced by sodium valproate in the 1990s. Since then, valproate has become a commonly prescribed treatment, and is effective in treating manic episodes.[90] Lamotrigine has some efficacy in treating bipolar depression, and this benefit is greatest in more severe depression.[91] It has also been shown to have some benefit in preventing further episodes, though there are concerns about the studies done, and is of no benefit in rapid cycling disorder.[92] The effectiveness of topiramate is unknown.[93] Depending on the severity of the case, anticonvulsants may be used in combination with lithium or on their own.
Antipsychotic medications are effective for short-term treatment of bipolar manic episodes and appear to be superior to lithium and anticonvulsants for this purpose.[50] However, other medications such as lithium are preferred for long-term use.[50] Olanzapine is effective in preventing relapses, although the evidence is not as solid as the evidence for lithium.[94] Antidepressants have not been found to be of any benefit over that found with mood stabilizers.[95]
Short courses of benzodiazepines may be used in addition to other medications until mood stabilizing become effective.[96]
Alternative medicine
Several studies have suggested that omega 3 fatty acids may have beneficial effects on depressive symptoms, but not manic symptoms. However, only a few small studies of variable quality have been published and there is not enough evidence to draw any firm conclusions.[97]
Prognosis
A lifelong condition with periods of partial or full recovery in between recurrent episodes of relapse,[23][97] bipolar disorder is considered to be a major health problem worldwide because of the increased rates of disability and premature mortality.[97] It is also associated with co-occurring psychiatric and medical problems and high rates of initial under- or misdiagnosis, causing a delay in appropriate treatment interventions and contributing to poorer prognoses.[25] After a diagnosis is made, it remains is difficult to achieve complete remission of all symptoms with the currently available psychiatric medications and symptoms often become progressively more severe over time.[63][98]
Compliance with medications is one of the most significant factors that can decrease the rate and severity of relapse and have a positive impact on overall prognosis.[99] However, the types of medications used in treating BD commonly cause side effects[100] and more than 75% of individuals with BD inconsistently take their medications for various reasons.[99]
Of the various types of the disorder, rapid cycling (four or more episodes in one year) is associated with the worst prognosis due to higher rates of self-harm and suicide.[23] Individuals diagnosed with bipolar who have a family history of bipolar disorder are at a greater risk for more frequent manic/hypomanic episodes.[101] Early onset and psychotic features are also associated with worse outcomes,[102][103] as well as subtypes that are nonresponsive to lithium.[98]
Early recognition and intervention also improve prognosis as the symptoms in earlier stages are less severe and more responsive to treatment.[98] Onset after adolescence is connected to better prognoses for both genders, and being male is a protective factor against higher levels of depression. For women, better social functioning prior to developing bipolar disorder and being a parent are protective towards suicide attempts.[101]
Functioning
People with bipolar disorder often experience a decline in cognitive functioning during (or possibly before) their first episode, after which a certain degree of cognitive dysfunction typically becomes permanent, with more severe impairment during acute phases and moderate impairment during periods of remission. As a result, two-thirds of people with BD continue to experience impaired psychosocial functioning in between episodes even when their mood symptoms are in full remission. A similar pattern in seen in both BD-I and BD-II, but people with BD-II experience a lesser degree of impairment.[100] Cognitive deficits typically increase over the course of the illness. Higher degrees of impairment correlate with the number of previous manic episodes and hospitalizations, and with the presence psychotic symptoms.[104] Early intervention can slow the progression of cognitive impairment, while treatment at later stages can help reduce distress and negative consequences related to cognitive dysfunction.[98]
Despite the overly ambitious goals that are frequently part of manic episodes, symptoms of mania undermine the ability to achieve these goals and often interfere an individual's social and occupational functioning. One third of people with BD remain unemployed for one year following a hospitalization for mania.[105] Depressive symptoms during and between episodes, which occur much more frequently for most people than hypomanic or manic symptoms over the course of illness, are associated with lower functional recovery in between episodes, including unemployment or underemployment for both BD-I and BD-II.[3][106] However, the course of illness (duration, age of onset, number of hospitalizations, and presence or not of rapid cycling) and cognitive performance are the best predictors of employment outcomes in individuals with bipolar disorder, followed by symptoms of depression and years of education.[106]
Recovery and recurrence
A naturalistic study from first admission for mania or mixed episode (representing the hospitalized and therefore most severe cases) found that 50 percent achieved syndromal recovery (no longer meeting criteria for the diagnosis) within six weeks and 98 percent within two years. Within two years, 72 percent achieved symptomatic recovery (no symptoms at all) and 43 percent achieved functional recovery (regaining of prior occupational and residential status). However, 40 percent went on to experience a new episode of mania or depression within 2 years of syndromal recovery, and 19 percent switched phases without recovery.[107]
Symptoms preceding a relapse (prodromal), specially those related to mania, can be reliably identified by people with bipolar disorder.[108] There have been intents to teach patients coping strategies when noticing such symptoms with encouraging results.[109]
Suicide
Bipolar disorder can cause suicidal ideation that leads to suicidal attempts. Individuals whose bipolar disorder begins with a depressive or mixed affective episode seem to have a poorer prognosis and an increased risk of suicide.[65] One out of two people with bipolar disorder attempt suicide at least once during their lifetime and many attempts are successfully completed.[16] The annual average suicide rate is 0.4 percent, which is 10–20 times that of the general population.[110] The standardized mortality ratio from suicide in bipolar disorder is between 18 and 25.[111] The lifetime risk of suicide has been estimated to be as high as 20 percent in those with bipolar disorder.[9]
Epidemiology
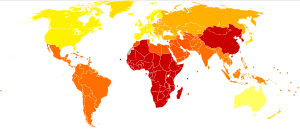
Bipolar disorder is the sixth leading cause of disability worldwide and has a lifetime prevalence of about 3 percent in the general population.[6][112] However, a reanalysis of data from the National Epidemiological Catchment Area survey in the United States suggested that 0.8 percent of the population experience a manic episode at least once (the diagnostic threshold for bipolar I) and a further 0.5 percent have a hypomanic episode (the diagnostic threshold for bipolar II or cyclothymia). Including sub-threshold diagnostic criteria, such as one or two symptoms over a short time-period, an additional 5.1 percent of the population, adding up to a total of 6.4 percent, were classified as having a bipolar spectrum disorder.[113] A more recent analysis of data from a second US National Comorbidity Survey found that 1 percent met lifetime prevalence criteria for bipolar I, 1.1 percent for bipolar II, and 2.4 percent for subthreshold symptoms.[114]
There are conceptual and methodological limitations and variations in the findings. Prevalence studies of bipolar disorder are typically carried out by lay interviewers who follow fully structured/fixed interview schemes; responses to single items from such interviews may suffer limited validity. In addition, diagnoses (and therefore estimates of prevalence) vary depending on whether a categorical or spectrum approach is used. This consideration has led to concerns about the potential for both underdiagnosis and overdiagnosis.[115]
The incidence of bipolar disorder is similar in men and women[116] as well as across different cultures and ethnic groups.[117] A 2000 study by the World Health Organization found that prevalence and incidence of bipolar disorder are very similar across the world. Age-standardized prevalence per 100,000 ranged from 421.0 in South Asia to 481.7 in Africa and Europe for men and from 450.3 in Africa and Europe to 491.6 in Oceania for women. However, severity may differ widely across the globe. Disability-adjusted life year rates, for example, appear to be higher in developing countries, where medical coverage may be poorer and medication less available.[118] Within the United States, Asian Americans have significantly lower rates than their African and European American counterparts.[119]
Late adolescence and early adulthood are peak years for the onset of bipolar disorder.[120][121] One study also found that in 10 percent of bipolar cases, the onset of mania had happened after the patient had turned 50.[122]
History

Variations in moods and energy levels have been observed as part of the human experience since throughout history. The words "melancholia", an old word for depression, and "mania" originated in Ancient Greece. The word melancholia is derived from melas (μελας), meaning "black", and chole (χολη), meaning "bile" or "gall",[123] indicative of the term's origins in pre-Hippocratic humoral theory. Within the humoral theories, mania was viewed as arising from an excess of yellow bile, or a mixture of black and yellow bile. The linguistic origins of mania, however, are not so clear-cut. Several etymologies were proposed by the Ancient Roman physician Caelius Aurelianus, including the Greek word ania, meaning "to produce great mental anguish", and manos, meaning "relaxed" or "loose", which would contextually approximate to an excessive relaxing of the mind or soul.[124] There are at least five other candidates, and part of the confusion surrounding the exact etymology of the word mania is its varied usage in the pre-Hippocratic poetry and mythology.[124]
In the early 1800s, French psychiatrist Jean-Étienne Dominique Esquirol's lypemania, one of his affective monomanias, was the first elaboration on what was to become modern depression.[125] The basis of the current conceptualisation of bipolar illness can be traced back to the 1850s; on January 31, 1854, Jules Baillarger described to the French Imperial Académie Nationale de Médecine a biphasic mental illness causing recurrent oscillations between mania and depression, which he termed folie à double forme (dual-form insanity).[126] Two weeks later, on February 14, 1854, Jean-Pierre Falret presented a description to the Academy on what was essentially the same disorder, and which he called folie circulaire (circular insanity).[127]
These concepts were developed by the German psychiatrist Emil Kraepelin (1856–1926), who, using Kahlbaum's concept of cyclothymia,[128] categorized and studied the natural course of untreated bipolar patients. He coined the term manic depressive psychosis, after noting that periods of acute illness, manic or depressive, were generally punctuated by relatively symptom-free intervals where the patient was able to function normally.[129]
The term "manic–depressive reaction" appeared in the first version of the DSM in 1952, influenced by the legacy of Adolf Meyer.[130] Subtyping into "unipolar" depressive disorders and bipolar disorders was first proposed by German psychiatrists Karl Kleist and Karl Leonhard in the 1950s and they have regarded as a separate conditions since publication of the DSM-III. The subtypes bipolar II and rapid cycling have been included since the DSM-IV, based on work from the 1970s by David Dunner, Elliot Gershon, Frederick Goodwin, Ronald Fieve and Joseph Fleiss.[131][132][133]
Society and culture

There are widespread problems with social stigma, stereotypes, and prejudice against individuals with a diagnosis of bipolar disorder.[134]
Kay Redfield Jamison, a clinical psychologist and professor of psychiatry at the Johns Hopkins University School of Medicine, profiled her own bipolar disorder in her memoir An Unquiet Mind (1995).[135] In his autobiography Manicdotes: There's Madness in His Method (2008) Chris Joseph describes his struggle between the creative dynamism which allowed the creation of his multimillion-pound advertising agency Hook Advertising, and the money-squandering dark despair of his bipolar illness.[136]
Several dramatic works have portrayed characters with traits suggestive of the diagnosis that has been the subject of discussion by psychiatrists and film experts alike. A notable example is Mr. Jones (1993), in which Mr. Jones (Richard Gere) swings from a manic episode into a depressive phase and back again, spending time in a psychiatric hospital and displaying many of the features of the syndrome.[137] In The Mosquito Coast (1986), Allie Fox (Harrison Ford) displays some features including recklessness, grandiosity, increased goal-directed activity and mood lability, as well as some paranoia.[138] Psychiatrists have suggested that Willy Loman, the main character in Arthur Miller's classic play Death of a Salesman, suffers from bipolar disorder,[139] though that specific term for the condition did not exist when the play was written.
TV specials, for example the BBC's Stephen Fry: The Secret Life of the Manic Depressive,[140] MTV's True Life: I'm Bipolar, talk shows, and public radio shows, and the greater willingness of public figures to discuss their own bipolar disorder, have focused on psychiatric conditions, thereby, raising public awareness.
On April 7, 2009, the nighttime drama 90210 on the CW network, aired a special episode where the character Silver was diagnosed with bipolar disorder.[141] Stacey Slater, a character from the BBC soap EastEnders, has been diagnosed with the disorder. The storyline was developed as part of the BBC's Headroom campaign.[142] The Channel 4 soap Brookside had earlier featured a story about bipolar disorder when the character Jimmy Corkhill was diagnosed with the condition.[143] 2011 Showtime's political thriller drama Homeland protagonist Carrie Mathison is bipolar, which she has kept secret since her school days.[144] In April 2014, ABC premiered a medical drama, Black Box, in which the main character, a world-renowned neuroscientist, is bipolar.[145]
Specific populations
Children

In the 1920s, Emil Kraepelin noted that manic episodes are rare before puberty.[146] In general, bipolar disorder in children was not recognized in the first half of the twentieth century. This issue diminished with an increased following of the DSM criteria in the last part of the twentieth century.[146][147]
While in adults the course of bipolar disorder is characterized by discrete episodes of depression and mania with no clear symptomatology between them, in children and adolescents very fast mood changes or even chronic symptoms are the norm.[148] Pediatric bipolar disorder is commonly characterized by outbursts of anger, irritability and psychosis, rather than euphoric mania, which is more likely to be seen in adults.[146][148] Early onset bipolar disorder is more likely to manifest as depression rather than mania or hypomania.[149]
The diagnosis of childhood bipolar disorder is controversial,[148] although it is not under discussion that the typical symptoms of bipolar disorder have negative consequences for minors suffering them.[146] The debate is mainly centered on whether what is called bipolar disorder in children refers to the same disorder as when diagnosing adults,[146] and the related question of whether the criteria for diagnosis for adults are useful and accurate when applied to children.[148] Regarding diagnosis of children, some experts recommend following the DSM criteria.[148] Others believe that these criteria do not correctly separate children with bipolar disorder from other problems such as ADHD, and emphasize fast mood cycles.[148] Still others argue that what accurately differentiates children with bipolar disorder is irritability.[148] The practice parameters of the AACAP encourage the first strategy.[146][148] American children and adolescents diagnosed with bipolar disorder in community hospitals increased 4-fold reaching rates of up to 40 percent in 10 years around the beginning of the 21st century, while in outpatient clinics it doubled reaching 6 percent.[148] Studies using DSM criteria show that up to 1 percent of youth may have bipolar disorder.[146]
Treatment involves medication and psychotherapy.[148] Drug prescription usually consists in mood stabilizers and atypical antipsychotics.[148] Among the former, lithium is the only compound approved by the FDA for children.[146] Psychological treatment combines normally education on the disease, group therapy and cognitive behavioral therapy.[148] Chronic medication is often needed.[148]
Current research directions for bipolar disorder in children include optimizing treatments, increasing the knowledge of the genetic and neurobiological basis of the pediatric disorder and improving diagnostic criteria.[148] Some treatment research suggests that psychosocial interventions that involve the family, psychoeducation, and skills building (through therapies such as CBT, DBT, and IPSRT) can benefit in a pharmocotherapy.[150] Unfortunately, the literature and research on the effects of psychosocial therapy on BPSD is scarce, making it difficult to determine the efficacy of various therapies.[150] The DSM-5 has proposed a new diagnosis which is considered to cover some presentations currently thought of as childhood-onset bipolar.[151]
Elderly
There is a relative lack of knowledge about bipolar disorder in late life. There is evidence that it becomes less prevalent with age but nevertheless accounts for a similar percentage of psychiatric admissions; that older bipolar patients had first experienced symptoms at a later age; that later onset of mania is associated with more neurologic impairment; that substance abuse is considerably less common in older groups; and that there is probably a greater degree of variation in presentation and course, for instance individuals may develop new-onset mania associated with vascular changes, or become manic only after recurrent depressive episodes, or may have been diagnosed with bipolar disorder at an early age and still meet criteria. There is also some weak and not conclusive evidence that mania is less intense and there is a higher prevalence of mixed episodes, although there may be a reduced response to treatment. Overall, there are likely more similarities than differences from younger adults.[152][153] In the elderly, recognition and treatment of bipolar disorder may be complicated by the presence of dementia or the side effects of medications being taken for other conditions.[154]
See also
- Bipolar disorders research
- Bipolar Disorders (journal)
Notes
- ↑ Coyle, Nessa; Paice, Judith A. (2015). Oxford Textbook of Palliative Nursing. Oxford University Press, Incorporated. p. 623. ISBN 9780199332342.
- 1 2 3 4 5 6 7 8 9 10 11 12 Anderson IM, Haddad PM, Scott J (Dec 27, 2012). "Bipolar disorder". BMJ (Clinical research ed.). 345: e8508. doi:10.1136/bmj.e8508. PMID 23271744.
- 1 2 3 4 5 6 7 8 9 10 11 American Psychiatry Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington: American Psychiatric Publishing. pp. 123–154. ISBN 0-89042-555-8.
- ↑ Goodwin, Guy M. "Bipolar disorder". Medicine. 40 (11): 596–598. doi:10.1016/j.mpmed.2012.08.011.
- ↑ NIMH (April 2016). "Bipolar Disorder". National Institutes of Health. Retrieved August 13, 2016.
- 1 2 Schmitt A, Malchow B, Hasan A, Falkai P (February 2014). "The impact of environmental factors in severe psychiatric disorders". Front Neurosci. 8 (19). doi:10.3389/fnins.2014.00019. PMC 3920481
 . PMID 24574956.
. PMID 24574956. - ↑ Diflorio, A; Jones, I (2010). "Is sex important? Gender differences in bipolar disorder". International Review of Psychiatry (Abingdon, England). 22 (5): 437–52. doi:10.3109/09540261.2010.514601. PMID 21047158.
- 1 2 Hirschfeld, RM; Vornik, LA (Jun 2005). "Bipolar disorder—costs and comorbidity.". The American journal of managed care. 11 (3 Suppl): S85–90. PMID 16097719.
- 1 2 3 4 5 6 7 8 9 10 Barnett JH, Smoller JW (2009). "The genetics of bipolar disorder". Neuroscience. 164 (1): 331–43. doi:10.1016/j.neuroscience.2009.03.080. PMC 3637882
 . PMID 19358880.
. PMID 19358880. - 1 2 3 4 5 6 7 8 9 10 11 Beentjes TA, Goossens PJ, Poslawsky IE (October 2012). "Caregiver burden in bipolar hypomania and mania: a systematic review". Perspect Psychiatr Care. 48 (4): 187–97. doi:10.1111/j.1744-6163.2012.00328.x. PMID 23005586.
- 1 2 3 Salvadore G, Quiroz JA, Machado-Vieira R, Henter ID, Manji HK, Zarate CA (November 2010). "The neurobiology of the switch process in bipolar disorder: a review". J Clin Psychiatry. 71 (11): 1488–1501. doi:10.4088/JCP.09r05259gre. PMC 3000635
 . PMID 20492846.
. PMID 20492846. - ↑ Titmarsh S (May–June 2013). "Characteristics and duration of mania: implications for continuation treatment". Progress in Neurology and Psychiatry. 17 (3): 26–7. doi:10.1002/pnp.283.
- 1 2 3 Tarr GP, Glue P, Herbison P (November 2011). "Comparative efficacy and acceptability of mood stabilizer and second generation antipsychotic monotherapy for acute mania—a systematic review and meta-analysis". J Affect Disord. 134 (1–3): 14–9. doi:10.1016/j.jad.2010.11.009. PMID 21145595.
- 1 2 Post RM, Kalivas P (March 2013). "Bipolar disorder and substance misuse: pathological and therapeutic implications of their comorbidity and cross-sensitisation". Br J Psychiatry. 202 (3): 172–6. doi:10.1192/bjp.bp.112.116855. PMID 23457180.
- ↑ Knowles R, McCarthy-Jones S, Rowse G (June 2011). "Grandiose delusions: a review and theoretical integration of cognitive and affective perspectives". Clin Psychol Rev. 31 (4): 684–96. doi:10.1016/j.cpr.2011.02.009. PMID 21482326.
- 1 2 3 4 5 6 Kerner B (February 2014). "Genetics of bipolar disorder". Appl Clin Genet. 7: 33–42. doi:10.2147/tacg.s39297. PMC 3966627
 . PMID 24683306.
. PMID 24683306. - ↑ Furukawa TA (2010). "Assessment of mood: Guides for clinicians". Journal of Psychosomatic Research. 68 (6): 581–589. doi:10.1016/j.jpsychores.2009.05.003. PMID 20488276.
- ↑ McKenna BS, Eyler LT (November 2012). "Overlapping prefrontal systems involved in cognitive and emotional processing in euthymic bipolar disorder and following sleep deprivation: a review of functional neuroimaging studies". Clin Psychol Rev. 32 (7): 650–63. doi:10.1016/j.cpr.2012.07.003. PMC 3922056
 . PMID 22926687.
. PMID 22926687. - 1 2 Mansell W, Pedley R (Mar 2008). "The ascent into mania: a review of psychological processes associated with the development of manic symptoms.". Clinical Psychology Review. 28 (3): 494–520. doi:10.1016/j.cpr.2007.07.010. PMID 17825463.
- 1 2 3 Bowins B (2007). "Cognitive regulatory control therapies". Am J Psychother. 67 (3): 215–36. PMID 24236353.
- ↑ "Bipolar Disorder: NIH Publication No. 95-3679". U.S. National Institutes of Health. September 1995. Archived from the original on April 29, 2008.
- ↑ "Bipolar II Disorder Symptoms and Signs". Web M.D. Retrieved December 6, 2010.
- 1 2 3 4 5 Muneer A (June 2013). "Treatment of the depressive phase of bipolar affective disorder: a review". J Pak Med Assoc. 63 (6): 763–9. PMID 23901682.
- ↑ "Practice Guideline for the Treatment of Patients With Bipolar Disorder Second Edition". APA Practice Guidelines for the Treatment of Psychiatric Disorders: Comprehensive Guidelines and Guideline Watches. 1. 2006. doi:10.1176/appi.books.9780890423363.50051. ISBN 978-0-89042-336-3.
- 1 2 Bowden CL (January 2001). "Strategies to reduce misdiagnosis of bipolar depression". Psychiatr Serv. 52 (1): 51–5. doi:10.1176/appi.ps.52.1.51. PMID 11141528.
- ↑ Muzina DJ, Kemp DE, McIntyre RS (October–December 2007). "Differentiating bipolar disorders from major depressive disorders: treatment implications". Ann Clin Psychiatry. 19 (4): 305–12. doi:10.1080/10401230701653591. PMID 18058287.
- 1 2 3 4 5 Swann AC, Lafer B, Perugi G, Frye MA, Bauer M, Bahk WM, Scott J, Ha K, Suppes T (January 2013). "Bipolar mixed states: an international society for bipolar disorders task force report of symptom structure, course of illness, and diagnosis". Am J Psychiatry. 170 (1): 31–42. doi:10.1176/appi.ajp.2012.12030301. PMID 23223893.
- ↑ Srivastava S, Ketter TA (December 2010). "The link between bipolar disorders and creativity: evidence from personality and temperament studies.". Current psychiatry reports. 12 (6): 522–30. doi:10.1007/s11920-010-0159-x. PMID 20936438.
- ↑ Goodwin & Jamison 2007, p. 338.
- ↑ Reinhardt MC, Reinhardt CA (March–April 2013). "Attention deficit-hyperactivity disorder, comorbidities, and risk situations". J Pediatr (Rio J). 89 (2): 124–30. doi:10.1016/j.jped.2013.03.015. PMID 23642421.
- ↑ Cirillo PC, Passos RB, Bevilaqua MC, López JR, Nardi AE (December 2012). "Bipolar disorder and Premenstrual Syndrome or Premenstrual Dysphoric Disorder comorbidity: a systematic review". Rev Bras Psiquiatr. 34 (4): 467–79. doi:10.1016/j.rbp.2012.04.010. PMID 23429819.
- ↑ Sagman D, Tohen M (2009). "Comorbidity in Bipolar Disorder: The Complexity of Diagnosis and Treatment". Psychiatric Times.
- 1 2 Nierenberg AA, Kansky C, Brennan BP, Shelton RC, Perlis R, Iosifescu DV (January 2013). "Mitochondrial modulators for bipolar disorder: a pathophysiologically informed paradigm for new drug development". Aust N Z J Psychiatry. 47 (1): 26–42. doi:10.1177/0004867412449303. PMID 22711881.
- 1 2 Edvardsen J, Torgersen S, Røysamb E, Lygren S, Skre I, Onstad S, Oien PA (2008). "Heritability of bipolar spectrum disorders. Unity or heterogeneity?". Journal of Affective Disorders. 106 (3): 229–240. doi:10.1016/j.jad.2007.07.001. PMID 17692389.
- ↑ Kieseppä T, Partonen T, Haukka J, Kaprio J, Lönnqvist J (2004). "High Concordance of Bipolar I Disorder in a Nationwide Sample of Twins". American Journal of Psychiatry. 161 (10): 1814–1821. doi:10.1176/appi.ajp.161.10.1814. PMID 15465978.
- ↑ McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A (2003). "The Heritability of Bipolar Affective Disorder and the Genetic Relationship to Unipolar Depression". Archives of General Psychiatry. 60 (5): 497–502. doi:10.1001/archpsyc.60.5.497. PMID 12742871.
- ↑ Reich T, Clayton PJ, Winokur G (1969). "Family history studies: V. The genetics of mania". The American Journal of Psychiatry. 125 (10): 1358–1369. doi:10.1176/ajp.125.10.1358. PMID 5304735.
- 1 2 3 Craddock N, Sklar P (May 2013). "Genetics of bipolar disorder". Lancet. 381 (9878): 1654–62. doi:10.1016/S0140-6736(13)60855-7. PMID 23663951.
- ↑ Segurado R, Detera-Wadleigh SD, Levinson DF, Lewis CM, Gill M, Nurnberger JI, Craddock N, DePaulo JR, Baron M, Gershon ES, Ekholm J, Cichon S, Turecki G, Claes S, Kelsoe JR, Schofield PR, Badenhop RF, Morissette J, Coon H, Blackwood D, McInnes LA, Foroud T, Edenberg HJ, Reich T, Rice JP, Goate A, McInnis MG, McMahon FJ, Badner JA, Goldin LR, Bennett P, Willour VL, Zandi PP, Liu J, Gilliam C, Juo SH, Berrettini WH, Yoshikawa T, Peltonen L, Lönnqvist J, Nöthen MM, Schumacher J, Windemuth C, Rietschel M, Propping P, Maier W, Alda M, Grof P, Rouleau GA, Del-Favero J, Van Broeckhoven C, Mendlewicz J, Adolfsson R, Spence MA, Luebbert H, Adams LJ, Donald JA, Mitchell PB, Barden N, Shink E, Byerley W, Muir W, Visscher PM, Macgregor S, Gurling H, Kalsi G, McQuillin A, Escamilla MA, Reus VI, Leon P, Freimer NB, Ewald H, Kruse TA, Mors O, Radhakrishna U, Blouin JL, Antonarakis SE, Akarsu N (2003). "Genome Scan Meta-Analysis of Schizophrenia and Bipolar Disorder, Part III: Bipolar Disorder". The American Journal of Human Genetics. 73 (1): 49–62. doi:10.1086/376547. PMC 1180589
 . PMID 12802785.
. PMID 12802785. - ↑ Frans EM, Sandin S, Reichenberg A, Lichtenstein P, Långström N, Hultman CM (2008). "Advancing Paternal Age and Bipolar Disorder". Archives of General Psychiatry. 65 (9): 1034–1040. doi:10.1001/archpsyc.65.9.1034. PMID 18762589.
- ↑ Kempton MJ, Geddes JR, Ettinger U, Williams SC, Grasby PM (2008). "Meta-analysis, Database, and Meta-regression of 98 Structural Imaging Studies in Bipolar Disorder". Archives of General Psychiatry. 65 (9): 1017–1032. doi:10.1001/archpsyc.65.9.1017. PMID 18762588.
- ↑ Arnone D, Cavanagh J, Gerber D, Lawrie SM, Ebmeier KP, McIntosh AM (2009). "Magnetic resonance imaging studies in bipolar disorder and schizophrenia: Meta-analysis". The British Journal of Psychiatry. 195 (3): 194–201. doi:10.1192/bjp.bp.108.059717. PMID 19721106.
- ↑ "Bipolar MRI Database". Bipolar Disorder Neuroimaging Database (BiND).
- ↑ Strakowski SM, Adler CM, Almeida J, Altshuler LL, Blumberg HP, Chang KD, DelBello MP, Frangou S, McIntosh A, Phillips ML, Sussman JE, Townsend JD (2012). "The functional neuroanatomy of bipolar disorder: A consensus model". Bipolar Disorders. 14 (4): 313–325. doi:10.1111/j.1399-5618.2012.01022.x. PMID 22631617.
- ↑ Bender RE, Alloy LB (April 2011). "Life stress and kindling in bipolar disorder: review of the evidence and integration with emerging biopsychosocial theories". Clin Psychol Rev. 31 (3): 383–98. doi:10.1016/j.cpr.2011.01.004. PMC 3072804
 . PMID 21334286.
. PMID 21334286. - ↑ Lee HJ, Son GH, Geum D (September 2013). "Circadian Rhythm Hypotheses of Mixed Features, Antidepressant Treatment Resistance, and Manic Switching in Bipolar Disorder". Psychiatry Investig. 10 (3): 225–32. doi:10.4306/pi.2013.10.3.225. PMC 3843013
 . PMID 24302944.
. PMID 24302944. - ↑ Brown & Basso 2004, p. 16.
- ↑ Dallaspezia S, Benedetti F (December 2009). "Melatonin, circadian rhythms, and the clock genes in bipolar disorder". Curr Psychiatry Rep. 11 (6): 488–93. doi:10.1007/s11920-009-0074-1. PMID 19909672.
- ↑ Serretti A, Mandelli L (2008). "The genetics of bipolar disorder: Genome 'hot regions,' genes, new potential candidates and future directions". Molecular Psychiatry. 13 (8): 742–771. doi:10.1038/mp.2008.29. PMID 18332878.
- 1 2 3 4 Geddes JR, Miklowitz DJ (May 11, 2013). "Treatment of bipolar disorder". Lancet. 381 (9878): 1672–82. doi:10.1016/S0140-6736(13)60857-0. PMID 23663953.
- ↑ Brietzke E, Kauer Sant'anna M, Jackowski A, Grassi-Oliveira R, Bucker J, Zugman A, Mansur RB, Bressan RA (December 2012). "Impact of childhood stress on psychopathology" (PDF). Rev Bras Psiquiatr. 34 (4): 480–8. doi:10.1016/j.rbp.2012.04.009. PMID 23429820.
- ↑ Miklowitz DJ, Chang KD (2008). "Prevention of bipolar disorder in at-risk children: Theoretical assumptions and empirical foundations". Development and Psychopathology. 20 (3): 881–897. doi:10.1017/S0954579408000424. PMC 2504732
 . PMID 18606036.
. PMID 18606036. - ↑ Murray ED, Buttner N, Price BH. (2012) Depression and Psychosis in Neurological Practice. In: Neurology in Clinical Practice, 6th Edition. Bradley WG, Daroff RB, Fenichel GM, Jankovic J (eds.) Butterworth Heinemann. April 12, 2012. ISBN 1-4377-0434-4 | ISBN 978-1-4377-0434-1
- ↑ Lahera G, Freund N, Sáiz-Ruiz J (January–March 2013). "Salience and dysregulation of the dopaminergic system" (PDF). Rev Psquiatr Salud Ment. 6 (1): 45–51. doi:10.1016/j.rpsm.2012.05.003. PMID 23084802.
- ↑ Berk M, Dodd S, Kauer-Sant'anna M, Malhi GS, Bourin M, Kapczinski F, Norman T (2007). "Dopamine dysregulation syndrome: implications for a dopamine hypothesis of bipolar disorder". Acta Psychiatr Scanda Suppl. 116 (Supplement s434): 41–49. doi:10.1111/j.1600-0447.2007.01058.x. PMID 17688462.
- ↑ Michael N, Erfurth A, Ohrmann P, Gössling M, Arolt V, Heindel W, Pfleiderer B (2003). "Acute mania is accompanied by elevated glutamate/glutamine levels within the left dorsolateral prefrontal cortex". Psychopharmacology. 168 (3): 344–346. doi:10.1007/s00213-003-1440-z. PMID 12684737.
- ↑ Benes FM, Berretta S (2001). "GABAergic interneurons: implications for understanding schizophrenia and bipolar disorder". Neuropsychopharmacology. 25 (1): 1–27. doi:10.1016/S0893-133X(01)00225-1. PMID 11377916.
- ↑ Miklowitz DJ, Chang KD (Summer 2008). "Prevention of bipolar disorder in at-risk children: theoretical assumptions and empirical foundations.". Development and Psychopathology. 20 (3): 881–97. doi:10.1017/s0954579408000424. PMC 2504732
 . PMID 18606036.
. PMID 18606036. - ↑ Khan MA, Akella S (December 2009). "Cannabis-Induced Bipolar Disorder with Psychotic Features: A Case Report". Psychiatry (Edgmont). 6 (12): 44–8. PMC 2811144
 . PMID 20104292.
. PMID 20104292. - 1 2 3 4 Price AL, Marzani-Nissen GR (March 2012). "Bipolar disorders: a review". Am Fam Physician. 85 (5): 483–93. PMID 22534227.
- ↑ Phillips ML, Kupfer DJ (May 2013). "Bipolar disorder diagnosis: challenges and future directions". Lancet. 381 (9878): 1663–71. doi:10.1016/S0140-6736(13)60989-7. PMID 23663952.
- ↑ Perugi, G.; Ghaemi, S. N.; Akiskal, H. (2006). "Diagnostic and Clinical Management Approaches to Bipolar Depression, Bipolar II and Their Comorbidities". Bipolar Psychopharmacotherapy. Caring for the Patient. pp. 193–234. doi:10.1002/0470017953.ch11. ISBN 978-0-470-01795-1.
- 1 2 3 Carvalho, AF; et al. (Feb 2015). "Screening for bipolar spectrum disorders: A comprehensive meta-analysis of accuracy studies". J Affective Disorders. 172: 337. doi:10.1016/j.jad.2014.10.024. PMID 25451435.
- 1 2 Picardi A (2009). "Rating scales in bipolar disorder". Current Opinion in Psychiatry. 22 (1): 42–49. doi:10.1097/YCO.0b013e328315a4d2. PMID 19122534.
- 1 2 Baldessarini RJ, Faedda GL, Offidani E, Vázquez GH, Marangoni C, Serra G, Tondo L (May 2013). "Antidepressant-associated mood-switching and transition from unipolar major depression to bipolar disorder: a review". J Affect Disord. 148 (1): 129–35. doi:10.1016/j.jad.2012.10.033. PMID 23219059.
- ↑ Sood AB, Razdan A, Weller EB, Weller RA (2005). "How to differentiate bipolar disorder from attention deficit hyperactivity disorder and other common psychiatric disorders: A guide for clinicians". Current psychiatry reports. 7 (2): 98–103. doi:10.1007/s11920-005-0005-8. PMID 15802085.
- ↑ Magill CA (2004). "The boundary between borderline personality disorder and bipolar disorder: Current concepts and challenges". Canadian Journal of Psychiatry. 49 (8): 551–556. PMID 15453104.
- ↑ Bassett D (2012). "Borderline personality disorder and bipolar affective disorder. Spectra or spectre? A review". Australian and New Zealand Journal of Psychiatry. 46 (4): 327–339. doi:10.1177/0004867411435289. PMID 22508593.
- ↑ Peet, M; Peters, S (1995). "Drug-induced mania". Drug Safety. 12 (2): 146. PMID 7766338.
- ↑ Korn ML. "Across the Bipolar Spectrum: From Practice to Research". Medscape.
- ↑ Beesdo K, Höfler M, Leibenluft E, Lieb R, Bauer M, Pfennig A (September 2009). "Mood episodes and mood disorders: patterns of incidence and conversion in the first three decades of life". Bipolar Disord. 11 (6): 637–49. doi:10.1111/j.1399-5618.2009.00738.x. PMC 2796427
 . PMID 19689506.
. PMID 19689506. - 1 2 Renk K, White R, Lauer BA, McSwiggan M, Puff J, Lowell A (February 2014). "Bipolar Disorder in Children". Psychiatry J. 2014 (928685): 1–19. doi:10.1155/2014/928685. PMC 3994906
 . PMID 24800202.
. PMID 24800202. - ↑ Van Meter AR, Youngstrom EA, Findling RL (June 2012). "Cyclothymic disorder: a critical review". Clin Psychol Rev. 32 (4): 229–43. doi:10.1016/j.cpr.2012.02.001. PMID 22459786.
- ↑ Angst J, Sellaro R (2000). "Historical perspectives and natural history of bipolar disorder". Biological Psychiatry. 48 (6): 445–457. doi:10.1016/s0006-3223(00)00909-4. PMID 11018218.
- ↑ Bauer M, Beaulieu S, Dunner DL, Lafer B, Kupka R (February 2008). "Rapid cycling bipolar disorder – diagnostic concepts". Bipolar Disorders. 10 (1 Pt 2): 153–62. doi:10.1111/j.1399-5618.2007.00560.x. PMID 18199234.
- ↑ Tillman R, Geller B (2003). "Definitions of Rapid, Ultrarapid, and Ultradian Cycling and of Episode Duration in Pediatric and Adult Bipolar Disorders: A Proposal to Distinguish Episodes from Cycles". Journal of Child and Adolescent Psychopharmacology. 13 (3): 267–271. doi:10.1089/104454603322572598. PMID 14642014.
- ↑ Fountoulakis KN, Kontis D, Gonda X, Yatham LN (March 2013). "A systematic review of the evidence on the treatment of rapid cycling bipolar disorder". Bipolar Disord. 15 (2): 115–37. doi:10.1111/bdi.12045. PMID 23437958.
- ↑ Becker T, Kilian R (2006). "Psychiatric services for people with severe mental illness across western Europe: What can be generalized from current knowledge about differences in provision, costs and outcomes of mental health care?". Acta Psychiatrica Scandinavica. 113 (429): 9–16. doi:10.1111/j.1600-0447.2005.00711.x. PMID 16445476.
- ↑ McGurk SR, Mueser KT, Feldman K, Wolfe R, Pascaris A (2007). "Cognitive Training for Supported Employment: 2–3 Year Outcomes of a Randomized Controlled Trial". American Journal of Psychiatry. 164 (3): 437–441. doi:10.1176/appi.ajp.164.3.437. PMID 17329468.
- ↑ Lam et al., 1999; Miklowitz & Goldstein, 1997; Frank, 2005.
- ↑ Leahy & Johnson 2003.
- ↑ Basco & Rush 2005.
- ↑ Zaretsky AE, Rizvi S, Parikh SV (2007). "How well do psychosocial interventions work in bipolar disorder?". Canadian Journal of Psychiatry. 52 (1): 14–21. PMID 17444074.
- ↑ Havens LL, Ghaemi SN (2005). "Existential despair and bipolar disorder: The therapeutic alliance as a mood stabilizer". American journal of psychotherapy. 59 (2): 137–147. PMID 16170918.
- ↑ Brown KM, Tracy DK (June 2013). "Lithium: the pharmacodynamic actions of the amazing ion". Ther Adv Psychopharmacol. 3 (3): 163–76. doi:10.1177/2045125312471963. PMC 3805456
 . PMID 24167688.
. PMID 24167688. - ↑ Cipriani A, Hawton K, Stockton S, Geddes JR (2013). "Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis". BMJ. 346: f3646. doi:10.1136/bmj.f3646. PMID 23814104.
- ↑ McCloud, TL; Caddy, C; Joachim, J; Rendell, JM; Diamond, PR; Shuttleworth, C; Brett, D; Amit, BH; McShane, R; Hamadi, L; Hawton, K; Cipriani, A (September 29, 2015). "Ketamine and other glutamate receptor modulators for depression in bipolar disorder in adults.". The Cochrane database of systematic reviews. 9: CD011611. doi:10.1002/14651858.CD011611.pub2. PMID 26415966.
- ↑ Post RM, Ketter TA, Uhde T, Ballenger JC (2007). "Thirty years of clinical experience with carbamazepine in the treatment of bipolar illness: Principles and practice". CNS Drugs. 21 (1): 47–71. doi:10.2165/00023210-200721010-00005. PMID 17190529.
- ↑ Rapoport SI, Basselin M, Kim HW, Rao JS (October 2009). "Bipolar disorder and mechanisms of action of mood stabilizers". Brain Res Rev. 61 (2): 185–209. doi:10.1016/j.brainresrev.2009.06.003. PMC 2757443
 . PMID 19555719.
. PMID 19555719. - ↑ Macritchie K, Geddes JR, Scott J, Haslam D, de Lima M, Goodwin G (2003). "Valproate for acute mood episodes in bipolar disorder". In Reid K. Cochrane Database of Systematic Reviews. Cochrane database of systematic reviews (Online). pp. CD004052. doi:10.1002/14651858.CD004052. PMID 12535506.
- ↑ Geddes JR, Calabrese JR, Goodwin GM (2008). "Lamotrigine for treatment of bipolar depression: Independent meta-analysis and meta-regression of individual patient data from five randomised trials". The British Journal of Psychiatry. 194 (1): 4–9. doi:10.1192/bjp.bp.107.048504. PMID 19118318.
- ↑ van der Loos ML, Kölling P, Knoppert-van der Klein EA, Nolen WA (2007). "Lamotrigine in the treatment of bipolar disorder, a review". Tijdschrift voor psychiatrie. 49 (2): 95–103. PMID 17290338.
- ↑ Vasudev K, Macritchie K, Geddes J, Watson S, Young A (2006). "Topiramate for acute affective episodes in bipolar disorder". In Young AH. Cochrane Database of Systematic Reviews. Cochrane database of systematic reviews (Online). pp. CD003384. doi:10.1002/14651858.CD003384.pub2. PMID 16437453.
- ↑ Cipriani A, Rendell JM, Geddes J (2009). Cipriani A, ed. "Olanzapine in long-term treatment for bipolar disorder". Cochrane database of systematic reviews (Online) (1): CD004367. doi:10.1002/14651858.CD004367.pub2. PMID 19160237.
- ↑ El-Mallakh RS, Elmaadawi AZ, Loganathan M, Lohano K, Gao Y (July 2010). "Bipolar disorder: an update". Postgraduate Medicine. 122 (4): 24–31. doi:10.3810/pgm.2010.07.2172. PMID 20675968.
- ↑ "Benzodiazepines for Bipolar Disorder". WebMD.com. Retrieved February 13, 2013.
- 1 2 3 Montgomery P, Richardson AJ (April 16, 2008). Montgomery P, ed. "Omega-3 fatty acids for bipolar disorder". The Cochrane database of systematic reviews (2): CD005169. doi:10.1002/14651858.CD005169.pub2. PMID 18425912.
Currently, there is simply not enough existing evidence, and what evidence is currently available is of such a varied and often-times questionable nature that no reliable conclusions may be drawn.
- 1 2 3 4 Muneer, Ather (2016), "Staging Models in Bipolar Disorder: A Systematic Review of the Literature", Clinical Psychopharmacology & Neuroscience, 14 (2): 117, doi:10.9758/cpn.2016.14.2.117, PMC 4857867

- 1 2 Jann, Michael W. (2014), "Diagnosis and Treatment of Bipolar Disorders in Adults: A Review of the Evidence on Pharmacologic Treatments", American Health & Drug Benefits, 7 (9): 489–499, PMC 4296286

- 1 2 Tsitsipa, Eirini; Fountoulakis, Konstantinos N. (1 December 2015), "The Neurocognitive Functioning in Bipolar Disorder: A Systematic Review of Data", Annals of General Psychiatry, 14: 42, doi:10.1186/s12991-015-0081-z, PMC 4666163

- 1 2 Maciukiewicz M, Pawlak J, Kapelski P, Łabędzka M, Skibinska M, Zaremba D, Leszczynska-Rodziewicz A, Dmitrzak-Weglarz M, Hauser J (2016). "Can Psychological, Social and Demographical Factors Predict Clinical Characteristics Symptomatology of Bipolar Affective Disorder and Schizophrenia?". Psychiatr Q. 87 (3): 501–13. doi:10.1007/s11126-015-9405-z. PMC 4945684
 . PMID 26646576.
. PMID 26646576. - ↑ Kennedy KP, Cullen KR, DeYoung CG, Klimes-Dougan B (2015). "The genetics of early-onset bipolar disorder: A systematic review". J Affect Disord. 184: 1–12. doi:10.1016/j.jad.2015.05.017. PMID 26057335.
- ↑ Serafini G, Pompili M, Borgwardt S, Houenou J, Geoffroy PA, Jardri R, Girardi P, Amore M (2014). "Brain changes in early-onset bipolar and unipolar depressive disorders: a systematic review in children and adolescents". Eur Child Adolesc Psychiatry. 23 (11): 1023–41. doi:10.1007/s00787-014-0614-z. PMID 25212880.
- ↑ Bortolato B, Miskowiak KW, Köhler CA, Vieta E, Carvalho AF (2015). "Cognitive dysfunction in bipolar disorder and schizophrenia: a systematic review of meta-analyses". Neuropsychiatr Dis Treat. 11: 3111–25. doi:10.2147/NDT.S76700. PMC 4689290
 . PMID 26719696.
. PMID 26719696. - ↑ Johnson, Sheri L. (2005), "Mania and Dysregulation in Goal Pursuit: A Review", Clinical Psychology Review, 25 (2): 241, doi:10.1016/j.cpr.2004.11.002, PMC 2847498

- 1 2 Tse S, Chan S, Ng KL, Yatham LN (2014). "Meta-analysis of predictors of favorable employment outcomes among individuals with bipolar disorder". Bipolar Disord. 16 (3): 217–29. doi:10.1111/bdi.12148. PMID 24219657.
- ↑ Tohen M, Zarate CA, Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, Salvatore P, Baldessarini RJ (2003). "The McLean-Harvard First-Episode Mania Study: Prediction of recovery and first recurrence". The American Journal of Psychiatry. 160 (12): 2099–2107. doi:10.1176/appi.ajp.160.12.2099. PMID 14638578.
- ↑ Jackson A, Cavanagh J, Scott J (2003). "A systematic review of manic and depressive prodromes". Journal of Affective Disorders. 74 (3): 209–217. doi:10.1016/s0165-0327(02)00266-5. PMID 12738039.
- ↑ Lam D, Wong G (2005). "Prodromes, coping strategies and psychological interventions in bipolar disorders". Clinical Psychology Review. 25 (8): 1028–1042. doi:10.1016/j.cpr.2005.06.005. PMID 16125292.
- ↑ Sadock, Kaplan & Sadock 2007, p. 388.
- ↑ Roger S. McIntyre, MD; Joanna K. Soczynska & Jakub Konarski. "Bipolar Disorder: Defining Remission and Selecting Treatment". Psychiatric Times, October 2006, Vol. XXIII, No. 11.
- ↑ Boland EM, Alloy LB (February 2013). "Sleep disturbance and cognitive deficits in bipolar disorder: toward an integrated examination of disorder maintenance and functional impairment". Clin Psychol Rev. 33 (1): 33–44. doi:10.1016/j.cpr.2012.10.001. PMC 3534911
 . PMID 23123569.
. PMID 23123569. - ↑ Judd LL, Akiskal HS (2003). "The prevalence and disability of bipolar spectrum disorders in the US population: Re-analysis of the ECA database taking into account subthreshold cases". Journal of Affective Disorders. 73 (1–2): 123–131. doi:10.1016/s0165-0327(02)00332-4. PMID 12507745.
- ↑ Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC (2007). "Lifetime and 12-Month Prevalence of Bipolar Spectrum Disorder in the National Comorbidity Survey Replication". Archives of General Psychiatry. 64 (5): 543–552. doi:10.1001/archpsyc.64.5.543. PMC 1931566
 . PMID 17485606.
. PMID 17485606. - ↑ Phelps J (2006). "Bipolar Disorder: Particle or Wave? DSM Categories or Spectrum Dimensions?". Psychiatric Times.
- ↑ Farren CK, Hill KP, Weiss RD (December 2012). "Bipolar disorder and alcohol use disorder: a review". Curr Psychiatry Rep. 14 (6): 659–66. doi:10.1007/s11920-012-0320-9. PMC 3730445
 . PMID 22983943.
. PMID 22983943. - ↑ Ferrari, AJ; Baxter, AJ; Whiteford, HA (2011). "A systematic review of the global distribution and availability of prevalence data for bipolar disorder". J Affective Disorders. Elsevier. 134: 1–13. doi:10.1016/j.jad.2010.11.007. PMID 21131055.
- ↑ Ayuso-Mateos, Jose Luis. "Global burden of bipolar disorder in the year 2000" (PDF). World Health Organization. Retrieved December 9, 2012.
- ↑ Kurasaki, Karen S. (2002). Asian American Mental Health: Assessment Theories and Methods. pp. 14–15.
- ↑ Christie KA, Burke JD, Regier DA, Rae DS, Boyd JH, Locke BZ (1988). "Epidemiologic evidence for early onset of mental disorders and higher risk of drug abuse in young adults". The American Journal of Psychiatry. 145 (8): 971–975. doi:10.1176/ajp.145.8.971. PMID 3394882.
- ↑ Goodwin & Jamison 2007, p. 1945.
- ↑ Monczor M (2010). "Bipolar disorder in the elderly". Vertex (Buenos Aires, Argentina). 21 (92): 275–283. PMID 21188315.
- ↑ Liddell & Scott 1980.
- 1 2 Angst J, Marneros A (December 2001). "Bipolarity from ancient to modern times: conception, birth and rebirth". J Affect Disord. 67 (1–3): 3–19. doi:10.1016/S0165-0327(01)00429-3. PMID 11869749.
- ↑ Borch-Jacobsen M (October 2010). "Which came first, the condition or the drug?". London Review of Books. 32 (19): 31–33.
at the beginning of the 19th century with Esquirol’s ‘affective monomanias’ (notably ‘lypemania’, the first elaboration of what was to become our modern depression)
- ↑ Pichot P (2004). "Circular insanity, 150 years on". Bulletin de l'Academie nationale de medecine (in French). 188 (2): 275–284. PMID 15506718.
- ↑ Sedler MJ (1983). "Falret's discovery: The origin of the concept of bipolar affective illness. Translated by M. J. Sedler and Eric C. Dessain". The American Journal of Psychiatry. 140 (9): 1127–1133. doi:10.1176/ajp.140.9.1127. PMID 6351641.
- ↑ Millon 1996, p. 290.
- ↑ Kraepelin, Emil (1921), Manic–depressive Insanity and Paranoia, ISBN 0-405-07441-7
- ↑ Goodwin & Jamison 2007, Chapter 1.
- ↑ Bipolar Depression: Molecular Neurobiology, Clinical Diagnosis and Pharmacotherapy Carlos A. Zarate Jr., Husseini K. Manji, Springer Science & Business Media, April 16, 2009
- ↑ The course of bipolar disorder Kate E. A. Saunders and Guy M. Goodwin, Advances in Psychiatric Treatment (2010) 16: 318-328 doi:10.1192/apt.bp.107.004903
- ↑ DAVID L.DUNNER Interviewed by Thomas A. Ban for the ANCP, Waikoloa, Hawaii, December 13, 2001
- ↑ Elgie R. Morselli PL (Feb–Mar 2007). "Social functioning in bipolar patients: the perception and perspective of patients, relatives and advocacy organizations – a review". Bipolar disorders. 9 (1–2): 144–57. doi:10.1111/j.1399-5618.2007.00339.x. PMID 17391357.
- ↑ Jamison 1995.
- ↑ Joseph 2008.
- ↑ Robinson 2003, pp. 78–81.
- ↑ Robinson 2003, pp. 84–85.
- ↑ McKinley, Jesse (February 28, 1999). "Get That Man Some Prozac; If the Dramatic Tension Is All in His Head". The New York Times. Retrieved March 3, 2012.
- ↑ "The Secret Life of the Manic Depressive". BBC. 2006. Archived from the original on January 18, 2010. Retrieved February 20, 2007.
- ↑ "Child and Adolescent Bipolar Foundation special 90210 website". CABF. 2009. Retrieved April 7, 2009.
- ↑ "EastEnders' Stacey faces bipolar disorder". BBC Press Office. May 14, 2009. Retrieved May 28, 2009.
- ↑ Tinniswood, Rachael (May 14, 2003). "The Brookie boys who shone at soap awards show". Liverpool Echo. Mirror Group Newspapers. Retrieved April 26, 2014.
- ↑ "Pilot". Homeland. Season 1. Episode 1. October 2, 2011. Showtime.
- ↑ "Catherine Black by Kelly Reilly". abc.go.com. ABC. Archived from the original on May 23, 2014. Retrieved May 22, 2014.
- 1 2 3 4 5 6 7 8 McClellan J, Kowatch R, Findling RL (2007). Work Group on Quality Issues. "Practice Parameter for the Assessment and Treatment of Children and Adolescents with Bipolar Disorder". Journal of the American Academy of Child & Adolescent Psychiatry. 46 (1): 107–125. doi:10.1097/01.chi.0000242240.69678.c4. PMID 17195735.
- ↑ Anthony, J.; Scott, P. (1960). "Manic–depressive Psychosis in Childhood". Journal of Child Psychology and Psychiatry. 1: 53–72. doi:10.1111/j.1469-7610.1960.tb01979.x.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Leibenluft E, Rich BA (2008). "Pediatric Bipolar Disorder". Annual Review of Clinical Psychology. 4: 163–187. doi:10.1146/annurev.clinpsy.4.022007.141216. PMID 17716034.
- ↑ Cosgrove VE, Roybal D, Chang KD (April 2013). "Bipolar depression in pediatric populations: epidemiology and management". Paediatr Drugs. 15 (2): 83–91. doi:10.1007/s40272-013-0022-8. PMID 23529869.
- 1 2 Fristad, MA; MacPherson, HA (2014). "Evidence-based psychosocial treatments for child and adolescent bipolar spectrum disorders.". Journal of Clinical Child and Adolescent Psychology. 43 (3): 339–55. doi:10.1080/15374416.2013.822309. PMID 23927375.
- ↑ Roy, AK; et al. (Sep 2014). "Disruptive mood dysregulation disorder: a new diagnostic approach to chronic irritability in youth". Am J Psychiatry. 171 (9): 918. doi:10.1176/appi.ajp.2014.13101301. PMC 4390118
 . PMID 25178749.
. PMID 25178749. - ↑ Vasudev A, Thomas A (July 2010). "'Bipolar disorder' in the elderly: what's in a name?". Maturitas. 66 (3): 231–5. doi:10.1016/j.maturitas.2010.02.013. PMID 20307944.
- ↑ Depp CA, Jeste DV (2004). "Bipolar disorder in older adults: A critical review". Bipolar Disorders. 6 (5): 343–367. doi:10.1111/j.1399-5618.2004.00139.x. PMID 15383127.
- ↑ Trinh NH, Forester B (2007). "Bipolar Disorder in the Elderly: Differential Diagnosis and Treatment". Psychiatric Times. 24 (14).
References
- Basco, Monica Ramirez; Rush, A. John (2005). Cognitive-Behavioral Therapy for Bipolar Disorder (Second ed.). New York: The Guilford Press. ISBN 978-1-59385-168-2. OCLC 300306925.
- Brown, Malcomb R.; Basso, Michael R. (2004). Focus on Bipolar Disorder Research. Nova Science Publishers. ISBN 978-1-59454-059-2.
- Joseph, Chris (2008). Manicdotes: There's Madness in His Method. London: Austin & Macauley. ISBN 978-1-905609-07-9. Amazon review.
- Goodwin, F. K.; Jamison, K. R. (2007). Manic–depressive illness: bipolar disorders and recurrent depression (2nd. ed.). Oxford University Press. ISBN 978-0-19-513579-4. OCLC 70929267. Retrieved April 2, 2016.
- Jamison, Kay Redfield (1995). An Unquiet Mind: A Memoir of Moods and Madness. New York: Knopf. ISBN 978-0-330-34651-1.
- Leahy, Robert L.; Johnson, Sheri L. (2003). Psychological Treatment of Bipolar Disorder. New York: The Guilford Press. ISBN 978-1-57230-924-1. OCLC 52714775.
- Liddell, Henry George; Scott, Robert (1980). A Greek-English Lexicon (Abridged ed.). Oxford University Press. ISBN 978-0-19-910207-5.
- Millon, Theordore (1996). Disorders of Personality: DSM-IV-TM and Beyond. New York: John Wiley and Sons. ISBN 978-0-471-01186-6.
- Robinson, D. J. (2003). Reel Psychiatry: Movie Portrayals of Psychiatric Conditions. Port Huron, Michigan: Rapid Psychler Press. ISBN 978-1-894328-07-4.
- Sadock, Benjamin J.; Kaplan, Harold I.; Sadock, Virginia A. (2007). Kaplan & Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (Tenth ed.). ISBN 978-0-7817-7327-0. Retrieved April 2, 2016.
Further reading
- Healy, David (2011). Mania: A Short History of Bipolar Disorder. Baltimore: Johns Hopkins University Press. ISBN 978-1-4214-0397-7.
- Mondimore, Francis Mark (2014). Bipolar Disorder: A Guide for Patients and Families (3rd ed.). Baltimore: Johns Hopkins University Press. ISBN 978-1-4214-1206-1.
- Yatham, Lakshmi (2010). Bipolar Disorder. New York: Wiley. ISBN 978-0-470-72198-8.
External links
| Library resources about Bipolar disorder |
- Bipolar Disorder at DMOZ
- Bipolar Disorder overview from the U.S. National Institute of Mental Health website
- NICE Bipolar Disorder clinical guidelines from the U.K. National Institute for Health and Clinical Excellence website