Meningioma
| Meningioma | |
|---|---|
 | |
| A contrast-enhanced CT scan of the brain, demonstrating the appearance of a meningioma | |
| Classification and external resources | |
| Specialty | Neurosurgery |
| ICD-10 | C70, D32 |
| ICD-9-CM | 225.2 |
| ICD-O | M9530/0 |
| OMIM | 607174 |
| DiseasesDB | 8008 |
| eMedicine | neuro/209 radio/439 |
| Patient UK | Meningioma |
| MeSH | D008579 |
Meningiomas are a diverse set of tumors arising from the meninges, the membranous layers surrounding the central nervous system.[1] Many meningiomas produce no symptoms throughout a person's life, and if discovered, require no treatment other than periodic observation. Typically, symptomatic meningiomas are treated with either radiosurgery or conventional surgery.
They arise from the arachnoid "cap" cells of the arachnoid villi in the meninges.[2] These tumors usually are benign in nature; however, a small percentage are cancerous.[3] Historical evidence of meningiomas has been found going back hundreds of years, with some successful surgeries for their removal beginning in the 1800s.
Signs and symptoms

Small tumors (e.g., < 2.0 cm) usually are incidental findings at autopsy without having caused symptoms. Larger tumors may cause symptoms, depending on the size and location.
- Focal seizures may be caused by meningiomas that overlie the cerebrum.
- Progressive spastic weakness in legs and incontinence may be caused by tumors that overlie the parasagittal frontoparietal region.
- Tumors of the Sylvian aqueduct may cause myriad motor, sensory, aphasic, and seizure symptoms, depending on the location.
- Increased intracranial pressure eventually occurs, but is less frequent than in gliomas.
- Diplopia (Double vision) or uneven pupil size may be symptoms if related pressure causes a third and/or sixth nerve palsy.
Causes
The causes of meningiomas are not well understood.[4] Most cases are sporadic, appearing randomly, while some are familial. Persons who have undergone radiation, especially to the scalp, are more at risk for developing meningiomas, as are those who have had a brain injury.[5] Atomic bomb survivors from Hiroshima had a higher than typical frequency of developing meningiomas, with the incidence increasing the closer that they were to the site of the explosion. Dental x-rays are correlated with an increased risk of meningioma, in particular for people who had frequent dental x-rays in the past, when the x-ray dose of a dental x-ray was higher than in the present.[6]
Having excess body fat increases the risk.[7] A 2012 review found that mobile telephone use was unrelated to meningioma.[8]
People with neurofibromatosis type 2 (NF-2) have a 50% chance of developing one or more meningiomas.
Ninety-two percent of meningiomas are benign. Eight percent are either atypical or malignant.[9]
Genetics
The most frequent genetic mutations (~50%) involved in meningiomas are inactivation mutations in the neurofibromatosis 2 gene (merlin) on chromosome 22q.
TRAF7 mutations are present in about one-fourth of meningiomas. Mutations in the TRAF7, KLF4, AKT1, and SMO genes are commonly expressed in benign skull-base meningiomas. Mutations in NF2 are commonly expressed in meningiomas located in the cerebral and cerebellar hemispheres.[10]
Pathophysiology
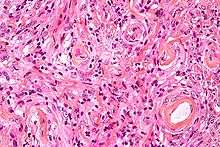
Meningiomas arise from arachnoidal cells,[11] most of which are near the vicinity of the venous sinuses, and this is the site of greatest prevalence for meningioma formation. They most frequently are attached to the dura over the superior parasagittal surface of frontal and parietal lobes, along the sphenoid ridge, in the olfactory grooves, the sylvian region, superior cerebellum along the falx cerebri, cerebellopontine angle, and the spinal cord. The tumor is usually gray, well-circumscribed, and takes on the form of the space it occupies. They usually are dome-shaped, with the base lying on the dura.
Locations
- Parasagittal/falcine (25%)
- Convexity (surface of the brain) (19%)
- Sphenoid ridge (17%)
- Suprasellar (9%)
- Posterior fossa (8%)
- Olfactory groove (8%)
- Middle fossa/Meckel's cave (4%)
- Tentorial (3%)
- Peri-torcular (3%)
Other uncommon locations are the lateral ventricle, foramen magnum, and the orbit/optic nerve sheath.[9] Meningiomas also may occur as a spinal tumor, more often in women than in men. This occurs more often in Western countries than Asian.
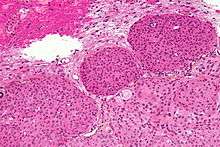
Histologically, meningioma cells are relatively uniform, with a tendency to encircle one another, forming whorls and psammoma bodies (laminated calcific concretions).[12] As such, they also have a tendency to calcify and are highly vascularized.
Meningiomas often are considered benign tumors that can be removed by surgery, but most recurrent meningiomas correspond to histologic benign tumors. The metabolic phenotype of these benign recurrent meningiomas indicated an aggressive metabolism resembling that observed for atypical meningioma.[13]
Diagnosis

Meningiomas are visualized readily with contrast CT, MRI with gadolinium,[14] and arteriography, all attributed to the fact that meningiomas are extra-axial and vascularized. CSF protein usually is elevated if lumbar puncture is attempted.
Although the majority of meningiomas are benign, they may have malignant presentations. Classification of meningiomas are based upon the WHO classification system.[15]
- Benign (Grade I) – (90%) – meningothelial, fibrous, transitional, psammomatous, angioblastic
- Atypical (Grade II) – (7%) – chordoid, clear cell, atypical (includes brain invasion)
- Anaplastic/malignant (Grade III) – (2%) – papillary, rhabdoid, anaplastic (most aggressive)
In a 2008 review of the latter two categories, atypical and anaplastic-meningioma cases, the mean overall survival for atypical meningiomas was found to be 11.9 years vs. 3.3 years for anaplastic meningiomas. Mean relapse-free survival for atypical meningiomas was 11.5 years vs. 2.7 years for anaplastic meningiomas.[16]
Malignant anaplastic meningioma is an especially malignant tumor with aggressive behavior. Even if, by general rule, neoplasms of the nervous system (brain tumors) cannot metastasize into the body because of the blood–brain barrier, anaplastic meningioma can. Although they are inside the cerebral cavity, they are located on the bloodside of the BBB, because meningiomas tend to be connected to blood vessels. Thus, cancerized cells can escape into the bloodstream, which is why meningiomas, when they metastasize, often turn up around the lungs.
Anaplastic meningioma and hemangiopericytoma are difficult to distinguish, even by pathological means, as they look similar, especially, if the first occurrence is a meningeal tumor, and both tumors occur in the same types of tissue.
Prevention
The risk of meningioma can be reduced by maintaining a normal body weight,[17] and by avoiding unnecessary dental x-rays.[18]
Treatment
Observation
Observation with close imaging follow-up may be used in select cases if a meningioma is small and asymptomatic. In a retrospective study on 43 patients, 63% of patients were found to have no growth on follow-up, and the 37% found to have growth at an average of 4 mm / year.[19] In this study, younger patients were found to have tumors that were more likely to have grown on repeat imaging; thus are poorer candidates for observation. In another study, clinical outcomes were compared for 213 patients undergoing surgery vs. 351 patients under watchful observation.[20] Only 6% of the conservatively treated patients developed symptoms later, while among the surgically treated patients, 5.6% developed persistent morbid condition, and 9.4% developed surgery-related morbid condition.
Observation is not recommended in tumors already causing symptoms. Furthermore, close follow-up with imaging is required with an observation strategy to rule out an enlarging tumor.[21]
Surgery
Meningiomas usually can be surgically resected (partially removed) and result in a permanent cure if the tumor is superficial on the dural surface and easily accessible. Transarterial embolization has become a standard preoperative procedure in the preoperative management.[22] If invasion of the adjacent bone occurs, total removal is nearly impossible. It is rare for benign meningiomas to become malignant.
The probability of a tumor recurring or growing after surgery may be estimated by comparing the tumor's WHO (World Health Organization) grade and by the extent of surgery by the Simpson Criteria.[23]
| Simpson Grade | Completeness of Resection | 10-year Recurrence |
|---|---|---|
| Grade I | complete removal including resection of underlying bone and associated dura | 9% |
| Grade II | complete removal and coagulation of dural attachment | 19% |
| Grade III | complete removal without resection of dura or coagulation | 29% |
| Grade IV | subtotal resection | 40% |
Radiation therapy
Radiation therapy may include photon-beam or proton-beam treatment, or fractionated external beam radiation. Radiosurgery may be used in lieu of surgery in small tumors located away from critical structures.[24] Fractionated external-beam radiation also can be used as primary treatment for tumors that are surgically unresectable or, for patients who are inoperable for medical reasons.
Radiation therapy often is considered for WHO grade I meningiomas after subtotal (incomplete) tumor resections. The clinical decision to irradiate after a subtotal resection is somewhat controversial, as no class I randomized, controlled trials exist on the subject.[25] Numerous retrospective studies, however, have suggested strongly that the addition of postoperative radiation to incomplete resections improves both progression-free survival (i.e. prevents tumor recurrence) and improves overall survival.[26]
In the case of a grade III meningioma, the current standard of care involves postoperative radiation treatment regardless of the degree of surgical resection.[27] This is due to the proportionally higher rate of local recurrence for these higher-grade tumors. Grade II tumors may behave variably and there is no standard of whether to give radiotherapy following a gross total resection. Subtotally resected grade II tumors should be radiated.
Chemotherapy
Likely, current chemotherapies are not effective. Antiprogestin agents have been used, but with variable results.[28] A 2007 study of whether hydroxyurea has the capacity to shrink unresectable or recurrent meningiomas is being further evaluated.[29]
Epidemiology
Many individuals have meningiomas, but remain asymptomatic, so the meningiomas are discovered during an autopsy. One to two percent of all autopsies reveal meningiomas that were unknown to the individuals during their lifetime, since there were never any symptoms. In the 1970s, tumors causing symptoms were discovered in 2 out of 100,000 people, while tumors discovered without causing symptoms occurred in 5.7 out of 100,000, for a total incidence of 7.7/100,000. With the advent of modern sophisticated imaging systems such as CT scans, the discovery of asymptomatic meningiomas has tripled.
Meningiomas are more likely to appear in women than men, though when they appear in men, they are more likely to be malignant. Meningiomas may appear at any age, but most commonly are noticed in men and women age 50 or older, with meningiomas becoming more likely with age. They have been observed in all cultures, Western and Eastern, in roughly the same statistical frequency as other possible brain tumors.[9]
History
The neoplasms currently referred to as meningiomas were referred to with a wide range of names in older medical literature, depending on the source. Various descriptors included "fungoid tumors", "fungus of the dura mater", "epithelioma", "psammoma", "dural sarcoma", "dural endothelioma", "fibrosarcoma", "angioendothelioma", "arachnoidal fibroboastoma", "endotheliosis of the meninges", "meningeal fibroblastoma", "meningoblastoma", "mestothelioma of the meninges", "sarcoma of the dura", and others.
The modern term of "meningioma" was used first by Harvey Cushing (1869–1939) in 1922, to describe a set of tumors that occur throughout the neuraxis (brain and spinal cord), but have various commonalities.[30][31] Charles Oberling then separated these into subtypes based on cell structure and, over the years, several other researchers have defined dozens of different subtypes as well. In 1979, the World Health Organization (WHO) classified seven subtypes, upgraded in 2000 to a classification system with nine low-grade variants (grade I tumors) and three variants each of grade II and grade III meningiomas.[31] The most common subtypes are Meningotheliomatous (63%), transitional or mixed-type (19%), fibrous (13%), and psammomatous (2%).[9]
The earliest evidence of a probable meningioma is from a skull approximately 365,000 years old, which was found in Germany. Other probable examples have been discovered in other continents around the world, including North and South America, and Africa.
The earliest written record of what was probably a meningioma is from the 1600s, when Felix Plater (1536–1614) of the University of Basel performed an autopsy on Sir Caspar Bonecurtius.[32] Surgery for removal of meningiomas was first attempted in the sixteenth century, but the first known successful surgery for removal of a meningioma of the convexity (parasagittal) was performed in 1770 by Anoine Luis.[33] The first documented successful removal of a skull base meningioma was performed in 1835 by Zanobi Pecchioli, Professor of Surgery at the University of Siena.[34] Other notable meningioma researchers have been William Macewen (1848–1924), and William W. Keen (1837–1932).[32]
Improvements in meningioma research and treatment over the last century have occurred in terms of the surgical techniques for removal of the tumor, and related improvements in anesthesia, antiseptic methods, techniques to control blood loss, better ability to determine which tumors are and are not operable,[35] and to effectively differentiate between the different meningioma subtypes.[36]
Notable cases
- Leonard Wood (1860–1927), underwent successful surgery by Dr. Harvey Cushing for a meningioma circa 1910, a major advance in neurosurgery at the time [37]
- Crystal Lee Sutton (1940–2009), American union organizer and inspiration for the film Norma Rae, died of a malignant meningioma [38][39]
- Kathi Goertzen (1958–2012), television news anchor in Seattle who underwent a very public battle with recurring tumors. She died on August 13, 2012 of complications related to her treatment.[40]
- Eileen Ford (1922-2014), American model agency executive and co-founder of Ford Models. Died on July 9, 2014 from complications of meningioma and osteoporosis.[41]
- Hillary Howard, American television news reporter, had a successful surgery to remove her meningioma in 2011[42][43]
- Mary Tyler Moore (b. 1936), American actress, underwent surgery in May 2011 to remove a benign meningioma[44][45]
- Sheryl Crow (b. 1962), American singer-songwriter, revealed to an audience in 2012 that she was diagnosed with meningioma, but her representative has stated that it is quite common. Crow is "happy and healthy."[46]
- Kyle Kuric (b. 1989), American basketball player currently with Spanish club CB Gran Canaria, had headaches early in the 2015–16 season, and tests revealed a meningioma.[47] He underwent surgery in Barcelona to remove the tumors, but encountered post-operative swelling of the brain, prompting a second surgery to relieve the pressure.[48]
References
- ↑ Cushing H. (1922). "The meningiomas (dural endotheliomas): their source, and favoured seats of origin". Brain. 45 (2): 282–316. doi:10.1093/brain/45.2.282.
- ↑ Buetow MP, Buetow PC, Smirniotopoulos JG (November 1991). "Typical, atypical, and misleading features in meningioma". Radiographics. 11 (6): 1087–106. doi:10.1148/radiographics.11.6.1749851. PMID 1749851. Retrieved 2008-12-01.
- ↑ Goldsmith BJ, Wara WM, Wilson CB, Larson DA (February 1994). "Postoperative irradiation for subtotally resected meningiomas. A retrospective analysis of 140 patients treated from 1967 to 1990". J. Neurosurg. 80 (2): 195–201. doi:10.3171/jns.1994.80.2.0195. PMID 8283256.
- ↑ "Meningioma". Mayo Clinic. Retrieved February 27, 2012.
- ↑ Longstreth, W.T. Jr.; et al. (June 28, 2006). "Epidemiology of intracranial Meningioma". Cancer. 72 (3): 639–648. doi:10.1002/1097-0142(19930801)72:3<639::AID-CNCR2820720304>3.0.CO;2-P. Retrieved April 5, 2012.
- ↑ "Dental x-rays and risk of meningioma". doi:10.1002/cncr.26625/abstract (inactive 2015-12-04). Retrieved 10 April 2012.
- ↑ Niedermaier, T; Behrens, G; Schmid, D; Schlecht, I; Fischer, B; Leitzmann, MF (16 September 2015). "Body mass index, physical activity, and risk of adult meningioma and glioma: A meta-analysis". Neurology. 85 (15): 1342–50. doi:10.1212/WNL.0000000000002020. PMID 26377253.
- ↑ Repacholi, MH; Lerchl, A; Röösli, M; Sienkiewicz, Z; Auvinen, A; Breckenkamp, J; d'Inzeo, G; Elliott, P; Frei, P; Heinrich, S; Lagroye, I; Lahkola, A; McCormick, DL; Thomas, S; Vecchia, P (April 2012). "Systematic review of wireless phone use and brain cancer and other head tumors.". Bioelectromagnetics. 33 (3): 187–206. doi:10.1002/bem.20716. PMID 22021071.
- 1 2 3 4 Park, Bong Jin; Kim, Han Kyu; Sade, Burak; Lee, Joung H. "Epidemiology", Meningiomas, pp. 11–13.
- ↑ Victoria E Clark; E. Zyenep Erson-Omay; Akdes Serin; et al. (March 2013). "Genomic analysis of non-NF2 meningiomas reveals mutations in TRAF7, KLF4, AKT1, and SMO.". Science. 339 (6123): 1077–80. doi:10.1126/science.1233009. PMC 4808587
 . PMID 23348505. Retrieved 30 January 2016.
. PMID 23348505. Retrieved 30 January 2016. - ↑ "moon.ouhsc.edu". Retrieved 2008-11-30.
- ↑ "Neuropathology For Medical Students". Retrieved 2008-11-30.
- ↑ Monleón D, Morales JM, Gonzalez-Segura A, Gonzalez-Darder JM, Gil-Benso R, Cerdá-Nicolás M, López-Ginés C (November 2010). "Metabolic aggressiveness in benign meningiomas with chromosomal instabilities". Cancer Research. 70 (21): 8426–8434. doi:10.1158/0008-5472.CAN-10-1498. PMID 20861191.
- ↑ "Meningioma]". Radiopaedia.
- ↑ Wrobel G, Roerig P, Kokocinski F, et al. (March 2005). "Microarray-based gene expression profiling of benign, atypical and anaplastic meningiomas identifies novel genes associated with meningioma progression". Int. J. Cancer. 114 (2): 249–56. doi:10.1002/ijc.20733. PMID 15540215.
- ↑ Yang SY, et al. (May 2008). "Atypical and anaplastic meningiomas: prognostic implications of clinicopathological features". J Neurol Neurosurg Psychiatry. 79 (5): 574–80. doi:10.1136/jnnp.2007.121582. PMID 17766430.
- ↑ Lauby-Secretan, B; Scoccianti, C; Loomis, D; Grosse, Y; Bianchini, F; Straif, K; International Agency for Research on Cancer Handbook Working, Group (25 August 2016). "Body Fatness and Cancer - Viewpoint of the IARC Working Group.". The New England journal of medicine. 375 (8): 794–798. PMID 27557308.
- ↑ http://www.webmd.com/brain/news/20120410/dental-x-rays-linked-brain-tumors
- ↑ Herscovici Z, et al. (Sep 2004). ": Natural history of conservatively treated meningiomas". Neurology. 63 (6): 1133–4. doi:10.1212/01.wnl.0000138569.45818.50. PMID 15452322.
- ↑ Yano S, Kuratsu J (2006). "Indications for surgery in patients with asymptomatic meningiomas based on an extensive experience". J Neurosurgery. 105 (4): 538–43. doi:10.3171/jns.2006.105.4.538.
- ↑ Olivero WC, et al. (Aug 1995). "The natural history and growth rate of asymptomatic meningiomas: a review of 60 patients". J Neurosurg. 83 (2): 222–4. doi:10.3171/jns.1995.83.2.0222. PMID 7616265.
- ↑ http://www.aans.org/education/journal/neurosurgical/july03/15-1-10.pdf
- ↑ Simpson D (Feb 1957). "The recurrence of intracranial meningiomas after surgical treatment". J Neurol Neurosurg Psychiatry. 20 (1): 22–39. doi:10.1136/jnnp.20.1.22. PMC 497230
 . PMID 13406590.
. PMID 13406590. - ↑ Kullova A, et al. (Aug 2007). ": Radiosurgery for benign meningioma". J Neurosurg. 107 (2): 325–36. doi:10.3171/JNS-07/08/0325. PMID 17695387.
- ↑ Taylor BW, et al. (Aug 1988). ": The meningioma controversy: postoperative radiation therapy". Int J Radiat Oncol Biol Phys. 15 (2): 299–304. PMID 3403313.
- ↑ Goldsmith BJ, et al. (1994). "Postoperative irradiation for subtotally resected meningiomas. A retrospective analysis of 140 patients treated from 1967 to 1990". J Neurosurg. 80 (2): 195–201. doi:10.3171/jns.1994.80.2.0195. PMID 8283256.
- ↑ Goyal LK, et al. (2000). "Local control and overall survival in atypical meningioma: a retrospective study". Int J Radiat Oncol Biol Phys. 46 (1): 57–61. PMID 10656373.
- ↑ Wahab M, et al. (Dec 2003). ": Meningioma and hormonal influences". Climacteric. 6 (4): 285–92. doi:10.1080/cmt.6.4.285.292. PMID 15006250.
- ↑ Newton HB (2007). "Hydroxyurea chemotherapy in the treatment of meningiomas". Neurosurg Focus. 23 (4): E11. doi:10.3171/foc-07/10/e11.
- ↑ Okonkwo et al. p. 5.
- 1 2 Prayson, Richard A. "Pathology of Meningiomas". Meningiomas. pp. 31–41.
- 1 2 Okonkwo et al. pp. 7–8.
- ↑ Louis A (1774). "Mêmoire sur les Tumeurs Fungueuses de la Dure-mère". Mem Acad Roy Chir. 5: 1–59.
- ↑ Mirimanoff. p. 18.
- ↑ DeMonte. Al-Mefty's Memas
- ↑ Al-Kadi, OS (April 2015). "A multiresolution clinical decision support system based on fractal model design for classification of histological brain tumours". Computerized Medical Imaging and Graphics. 41: 67–79. doi:10.1016/j.compmedimag.2014.05.013. PMID 24962336.
- ↑ Okonkwo, David O.; Laws, Edward R. Jr. "Meningiomas: Historical perspective". Meningiomas. p. 8.
- ↑ Handgraaf, Brie (2008-06-28). "Real 'Norma Rae' has new battle involving cancer". The Times-News. Archived from the original on 2009-06-29.
- ↑ Sturgis, Sue (2009-09-14). "Real 'Norma Rae' dies of cancer after insurer delayed treatment". Facing South. Institute for Southern Studies.
- ↑ Staff (February 6, 2013). "News anchor Kathi Goertzen dies after long illness". CBS-Channel 5 KING. Retrieved March 5, 2015.
- ↑ Notice of death of Eileen Ford, with causes provided, CNN.com, July 10, 2014; accessed July 13, 2014.
- ↑ "Hillary Howard of WTOP is upbeat about brain surgery". The Washington Post. 2011-04-04. Retrieved February 25, 2012.
- ↑ "Update: Hillary Howard recovering from brain surgery". The Washington Post. 2011-04-18. Retrieved February 25, 2012.
- ↑ Goldman, Russell (May 12, 2011). "Mary Tyler Moore has brain surgery for meningioma tumor". ABC News. Retrieved 2012-02-25.
- ↑ Genzlinger, Neil (January 26, 2012). "Boy, did she make it". The New York Times. Retrieved February 25, 2012.
- ↑ Ann Oldenburg (June 5, 2012). "Sheryl Crow has a benign brain tumor". Los Angeles Daily News. Retrieved 2012-06-05.
- ↑ Crawford, Eric (November 3, 2015). "Former Louisville star Kuric to undergo brain surgery in Spain". Louisville, KY: WDRB. Retrieved November 4, 2015.
- ↑ Crawford, Eric (November 10, 2015). "Kuric off ventilator as condition improves following brain surgery". Louisville, KY: WDRB. Retrieved November 10, 2015.
- Sources
- Lee, Joung H. (2009). Meningiomas: Diagnosis, Treatment, and Outcome. Cleveland, Ohio, USA: Springer-Verlag. ISBN 978-1-84882-910-7.
- DeMonte, Franco; Ossama Al-Mefty; Michael McDermott (2011). Al-Mefty's Meningiomas (2nd ed.). Thieme. ISBN 978-1-60406-053-9.
External links
- MR/CT scans of meningioma from MedPix
- MR/CT scans of pneumosinus dilatans from MedPix
- Cancer.Net: Meningioma