Mosquito net


A mosquito net offers protection against mosquitos,[1] flies, and other insects, and thus against the diseases they may carry. Examples include malaria, dengue fever, yellow fever, and various forms of encephalitis, including the West Nile virus.[2] To be effective the mesh of a mosquito net must be fine enough to exclude such insects without reducing visibility or air flow to unacceptable levels. It is possible to increase the effectiveness of a mosquito net greatly by treating it with an appropriate insecticide or mosquito repellant.
History
The usage of mosquito netting is mainly used for the protection against the malaria transmitting vector, Anopheles gambiae. The first record of malaria-like symptoms occurred as early as 2700 BCE from China. The vector for this disease was not identified until 1880 when Charles Louis Alphonse Laveran identified mosquitos as a vector for malaria.[3]
Mosquito netting has a long history. Though use of the term dates from the mid-18th century,[1] Indian literature from the late medieval period has references to the usage of mosquito nets in ritual Hindu worship. Poetry composed by Annamayya, the earliest known Telugu musician and poet, references domatera, which means mosquito net in Telugu.[4] Use of mosquito nets has been dated to prehistoric times. It is said that Cleopatra, the last active pharaoh of Ancient Egypt, also slept under a mosquito net.[5] Mosquito nets were used during the malaria-plagued construction of the Suez Canal.[5]
Construction
Mosquito netting can be made from cotton, polyethylene, polyester, polypropylene, or nylon.[6] A mesh size of 1.2 mm stops mosquitoes, and smaller, such as 0.6 mm, stops other biting insects such as biting midges/no-see-ums.[7]
A mosquito bar is an alternate form of a mosquito net. It is constructed of a fine see-through mesh fabric mounted on and draped over a box-shaped frame. It is designed to fit over an area or item such as a sleeping bag to supply protection from insects. A mosquito bar could be used to protect oneself from mosquitos and other insects while sleeping in jungle areas.[8] The mesh is woven tightly enough to stop insects from entering but loosely enough to not interfere with ventilation. The frame is usually self-supporting or freestanding although it can be designed to be attached from the top to an alternative support such as tree limbs.[8]
Usage
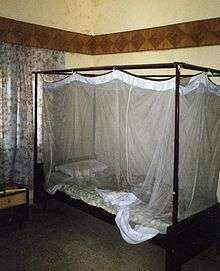
Mosquito nets are often used where malaria or other insect-borne diseases are common, especially as a tent-like covering over a bed. For effectiveness, it is important that the netting does not have holes or gaps large enough to allow insects to enter. It is also important to 'seal' the net properly because mosquitos are able to 'squeeze' through improperly secured nets. Because an insect can bite a person through the net, the net must not rest directly on the skin.[9]
Mosquito netting can be hung over beds from the ceiling or a frame, built into tents, or installed in windows and doors. When hung over beds, rectangular nets provide more room for sleeping without the danger of netting contacting skin, at which point mosquitos may bite through untreated netting.[10]
Where mosquito nets are freely or cheaply distributed, local residents sometimes opportunistically use them inappropriately, for example as fishing nets. When used for fishing, mosquito nets have harmful ecological consequences because the fine mesh of a mosquito net retains almost all fishes, including bycatch such as immature or small fish and fish species that are not suitable for consumption.[11][12][13] In addition, insecticides with which the mesh has been treated, such as permethrin, may be harmful to the fish and other aquatic fauna.[11]
Insecticide-treated nets
Mosquito nets treated with insecticides—known as insecticide-treated nets (ITNs) or bednets—were developed in the 1980s for malaria prevention. ITNs are estimated to be twice as effective as untreated nets,[14] and offer greater than 70% protection compared with no net.[15] These nets are dip-treated using a synthetic pyrethroid insecticide such as deltamethrin or permethrin which will double the protection over a non-treated net by killing and repelling mosquitoes. For maximum effectiveness, ITNs should be re-impregnated with insecticide every six months. This process poses a significant logistical problem in rural areas. Newer, long-lasting insecticidal nets (LLINs) have now replaced ITNs in most countries.[16]
Effectiveness
The distribution of mosquito nets or bednets impregnated with insecticides such as permethrin or deltamethrin has been shown to be an extremely effective method of malaria prevention. It is also one of the most cost-effective methods of prevention. These nets can often be obtained for around $2.50–$3.50 (2–3 euros) from the United Nations, the World Health Organization (WHO), and others. ITNs have been shown to be the most cost-effective prevention method against malaria and are part of WHO’s Millennium Development Goals (MDGs).[17] Generally LLINs are purchased by donor groups and delivered through in-country distribution networks.
ITNs protect people sleeping under them and simultaneously kill mosquitoes that contact the nets. Some protection is provided to others by this method, including people sleeping in the same room but not under the net. However, mathematical modeling has suggested that disease transmission may be exacerbated after bed nets have lost their insecticidal properties under certain circumstances.[18] Although ITN users are still protected by the physical barrier of the netting, non-users could experience an increased bite rate as mosquitoes are deflected away from the non-lethal bed net users.[18] The modeling suggests that this could increase transmission when the human population density is high or at lower human densities when mosquitoes are more adept at locating their blood meals.[18]
Distribution
While some experts argue that international organizations should distribute ITNs and LLINs to people for free to maximize coverage (since such a policy would reduce price barriers), others insist that cost-sharing between the international organization and recipients would lead to greater use of the net (arguing that people will value a good more if they pay for it). Additionally, proponents of cost-sharing argue that such a policy ensures that nets are efficiently allocated to the people who most need them (or are most vulnerable to infection). Through a "selection effect", they argue, the people who most need the bed nets will choose to purchase them, while those less in need will opt out.
However, a randomized controlled trial study of ITNs uptake among pregnant women in Kenya, conducted by economists Pascaline Dupas and Jessica Cohen, found that cost-sharing does not necessarily increase the usage intensity of ITNs nor does it induce uptake by those most vulnerable to infection, as compared to a policy of free distribution.[19][20] In some cases, cost-sharing can decrease demand for mosquito nets by erecting a price barrier. Dupas and Cohen’s findings support the argument that free distribution of ITNs can be more effective than cost-sharing in increasing coverage and saving lives. In a cost-effectiveness analysis, Dupas and Cohen note that "cost-sharing is at best marginally more cost-effective than free distribution, but free distribution leads to many more lives saved."[19]
The researchers base their conclusions about the cost-effectiveness of free distribution on the proven spillover benefits of increased ITN usage.[21] ITNs protect the individuals or households that use them, and they protect people in the surrounding community in one of two ways.[22]
- First, ITNs kill adult mosquitos infected with the malaria parasite directly which increases their mortality rate and can therefore decrease the frequency in which a person in the community is bit by an infected mosquito.[23]
- Second, certain malaria parasites require days to develop in the salivary glands of the vector mosquito. This process can be accelerated or decelerated via weather; more specifically heat.[24] Plasmodium falciparum, for example, the parasite that is responsible for the majority of deaths in Sub-Saharan Africa, takes 8 days to mature. Therefore, malaria transmission to humans does not take place until approximately the 10th day, although it requires blood meals at intervals of 2 to 5 days.[25] By killing mosquitoes before maturation of the malaria parasite, ITNs can reduce the number of encounters of infected mosquitos with humans.[23]
When a large number of nets are distributed in one residential area, their chemical additives help reduce the number of mosquitoes in the environment. With fewer mosquitoes, the chances of malaria infection for recipients and non-recipients are significantly reduced. (In other words, the importance of the physical barrier effect of ITNs decreases relative to the positive externality effect of the nets in creating a mosquito-free environment when ITNs are highly concentrated in one residential cluster or community.)
Unfortunately, standard ITNs must be replaced or re-treated with insecticide after six washes and, therefore, are not seen as a convenient, effective long-term solution to the malaria problem.[26] As a result, the mosquito netting and pesticide industries developed so-called long-lasting insecticidal mosquito nets, which also use pyrethroid insecticides. There are three types of LLINs — polyester netting which has insecticide bound to the external surface of the netting fibre using a resin; polyethylene which has insecticide incorporated into the fibre and polypropylene which has insecticide incorporated into the fibre. All types can be washed at least 20 times, but physical durability will vary. A survey carried out in Tanzania concluded that effective life of polyester nets was 2 to 3 years;[27] with polyethylene LLINs there is data to support over 5 years of life with trials in showing nets which were still effective after 7 years.[28] When calculating the cost of LLINs for large-scale malaria prevention campaigns, the cost should be divided by the number of years of expected life: A more expensive net may be cheaper over time. In addition the logistical costs of replacing nets should be added to the calculation.
Scientific trials
A review of 22 randomized controlled trials of ITNs[29] found (for Plasmodium falciparum malaria) that ITNs can reduce deaths in children by one fifth and episodes of malaria by half.
More specifically, in areas of stable malaria "ITNs reduced the incidence of uncomplicated malarial episodes by 50% compared to no nets, and 39% compared to untreated nets" and in areas of unstable malaria "by 62% compared to no nets and 43% compared to untreated nets". As such the review calculated that for every 1000 children protected by ITNs, 5.5 lives would be saved each year.
Through the years 1999 and 2010 the abundance of female anopheles gambiae densities in houses throughout western Kenya were recorded. This data set was paired with the spatial data of bed net usage in order to determine correlation. Results showed that from 2008 to 2010 the relative population density of the female anopheles gambiae decreased from 90.6% to 60.7%.[30] The conclusion of this study showed than as the number of houses which used insecticide treated bed nets increased the population density of female anopheles gambiae decreased. This result did however vary from region to region based on the local environment.
Associated problems
Malaria and other arboviruses are known to contribute to economic disparity within that country and vice versa. This opens the stage for corruption associated to the distribution of self-protection aides.[31] The least wealthy members of society are both more likely to be in closer proximity to the vectors' prime habitat, but are also less likely to be protected from the vectors.[32] This increase in probability of being infected increases the demand for self-protection which therefore allows for unfair pricing and distribution of self-protection means. A decrease in per capita income exaggerates a high demand for resources such as water and food resulting in civil unrest among communities. Protecting resources as well as attempting to obtain resources are both a cause for conflict.
Alternatives
Mosquito nets do reduce air flow to an extent and sleeping under a net is hotter than sleeping without one, which can be uncomfortable in tropical areas without air-conditioning.
Some alternatives are:
- The use of a fan to increase air flow.[33]
- The application of an insect repellent to the skin; this also may be less effective (reducing rather than eliminating bites), more expensive, and may pose health risks with long-term use.
- Wearing clothing treated with insect repellency. Insect repellent clothing offers the advantage of long lasting protection, requiring no re-application. This protection is usually odorless and invisible, and, unlike traditional insect repellents, the repellency is near your skin, instead of on it, which can help alleviate concerns about overuse or misuse of insect repellent.
- The use of Indoor residual spraying of insecticides. This was a common practice back in late 20th Century. However, due to the publication of the book "Silent Spring" which identified some environmental hazards associated with the insecticide DDT usage for these programs. The effects of this book on government aide was disastrous; American funding for African programs were cut off and the number of malaria infected subjects skyrocketed. In order to see results from the usage of indoor residual spraying programs 80% of the towns homes need to be sprayed and the continual application of insecticide needs to be constant in order to suppress certain species densities which are immune to the insecticide.[34] Large scale application results in a dependence on continual spraying. If the aggressive style of application is not maintained one would risk the possibility of a bloom in genetically resistant mosquitos. This would ultimately result in an unrealistic mediation process.[35]
See also
- Nothing But Nets
- Against Malaria Foundation
- Screened porch
- Mosquito Trapping Net MTN
References
- 1 2 Oxford English Dictionary (draft ed.). Oxford University Press. 2009.
- ↑ "All Mosquito Netting Info". Retrieved 2009-10-27.
- ↑ 28. ^Murray, John. "Mosquitoes, malaria and man: a history of the hostilities since 1880.." Cab Direct 1 (1978): 1-314. Print.
- 1 2 "History of Malaria Control". Archived from the original on November 11, 2009. Retrieved 2009-10-27.
- ↑ "World Health Organization: Annex VII : Procedure for Treating Mosquito Nets and curtains" (PDF). Retrieved 2009-10-27.
- ↑ "Mosquito Netting Criteria". Retrieved 2009-10-27.
- 1 2 Tawrell, Paul (2006). Camping & wilderness survival : the ultimate outdoors book (2nd ed.). Lebanon, NH: Paul Tawrell. p. 92. ISBN 0-9740820-2-3.
- ↑ "Insecticide-Treated Bed Nets." Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, 9 Nov. 2012. Web. 23 Feb. 2014. <http://www.cdc.gov/malaria/malaria_worldwide
- ↑ "Travel Health Help: Mosquito Nets". Archived from the original on April 12, 2010. Retrieved 2009-10-27.
- 1 2 Gettlemanjan, Jeffrey (2015-01-24), "Meant to Keep Mosquitos Out, Nets Are Used to Haul Fish In", The New York Times
- ↑ "Malaria Journal - Full text - Unforeseen misuses of bed nets in fishing villages along Lake Victoria". malariajournal.com.
- ↑ "IRIN Africa - ZAMBIA: Mosquito-net fishing threatens Lake Tanganyika - Zambia - Economy - Environment - Food Security - Water & Sanitation". IRINnews.
- ↑ Hull, Kevin. (2006). "Malaria: Fever Wars". PBS.
- ↑ Bachou H, Tylleskär T, Kaddu-Mulindwa DH, Tumwine JK (2006). "Bacteraemia among severely malnourished children infected and uninfected with the human immunodeficiency virus-1 in Kampala, Uganda". BMC Infect. Dis. 6: 160. doi:10.1186/1471-2334-6-160. PMC 1660577
 . PMID 17090299.
. PMID 17090299. - ↑ "BMC International Health and Human Rights - Full text - Africa's largest long-lasting insecticide-treated net producer: lessons from A to Z Textiles". biomedcentral.com.
- ↑ "World Health Organization: MDG 6: combat HIV/AIDS, malaria and other diseases". Retrieved 2011-10-28.
- 1 2 3 Yakob, Laith; Guiyun Yan (2009). "Modeling the Effects of Integrating Larval Habitat Source Reduction and Insecticide Treated Nets for Malaria Control". PLoS ONE. Public Library of Science. 4 (9). doi:10.1371/journal.pone.0006921.
- 1 2 Jessica Cohen; Pascaline Dupas (February 2010). "Free Distribution or Cost-Sharing? Evidence from a Randomized Malaria Prevention Experiment" (PDF). Quarterly Journal of Economics. 125 (1): 24. doi:10.1162/qjec.2010.125.1.1. Archived from the original (PDF) on April 10, 2011.
- ↑ "Free Distribution or Cost-Sharing: Evidence from a Malaria Prevention Experiment in Kenya". Innovations for Poverty Action (IPA). Retrieved 2010-02-18.
- ↑ Hawley, William A.; et al. (2003). "Community-Wide Effects of Permethrin-Treated Bed Nets on Child Mortality and Malaria Morbidity in Western Kenya" (PDF). American Journal of Tropical Medicine and Hygiene 68 (Suppl. 4). Retrieved 2010-02-18.
- ↑ Maxwell CA, Msuya E, Sudi M, Njunwa KJ, Carneiro IA, et al. (2002) Effect of community-wide use of insecticide-treated nets for 3–4 years on malarial morbidity in Tanzania. Tropical Medicine and International Health, 7: 1003–1008.
- 1 2 Killeen GF, Smith TA (2007) Exploring the contributions of bednets, cattle, insecticides and excito-repellency to malaria control: A deterministic model of mosquito host-seeking behaviour and mortality. American Journal of Tropical Medicine and Hygiene.
- ↑ "Plasmodium falciparum: in vitro growth inhibition by febrile temperatures." Parasitology Research 87.7 (2001): 553-555. Print.
- ↑ Smith DL, McKenzie FE (2004) Statics and dynamics of malaria infection in Anopheles mosquitoes. Malaria Journal 3: 13.
- ↑ "Insecticide-Treated Mosquito Nets" (PDF). WHO. p. 5. Archived from the original (PDF) on October 7, 2009.
- ↑ Erlanger et al., 2004, Med Vet Entomol 18: 153-160
- ↑ Tami, A et al. Malaria Journal 2004, 3:19
- ↑ Lengeler C. (2004) Insecticide-treated bed nets and curtains for preventing malaria. The Cochrane Database of Systematic Reviews. Issue 2.
- ↑ Minakawa, Noboru . "Impacts of insecticide treated bed nets on Anopheles gambiae s.l. populations in Mbita district and Suba district, Western Kenya." Annals of Surgical and Innovation and Research 7 (2014): 2-13. Print.
- ↑ Teklehaimanot, Awash. "Malaria and Poverty." Annals of New York Academy of Sciences 1136 (2008): 32-37. Print.
- ↑ 31. ^Rivero-Rodriguez, L . "Exposure assessment for workers applying DDT to control malaria in Veracruz, Mexico.." Environemtal Health Perspectives 1 (1997): 98-101. Print.
- ↑ "House Fans and Mosquitoes." New York Times. N.p., n.d. Web. 24 Feb. 2014. <http://well.blogs.nytimes.com/2010/07/12/house-fans-and-mosquitoes/?_php=true&_type=blogs&_r=0>.
- ↑ Pluess, Bianca. "Indoor residual spraying for preventing malaria." The Cochrane Library 1 (2010): n. pag. Wiley online library. Web. 21 Feb. 2014.
- ↑ Chareonviriyaphap , Theeraphap . "Review of insecticide resistance and behavioral avoidance of vectors of human diseases in Thailand." BioMed Central 6 (2013): Web. 21 Feb. 2014.
External links
- World Health Organization
- Organization Malaria NIMBY Not In My Back Yard
- "Malaria and Poverty" article from Wiley