Nephron
| Nephron | |
|---|---|
|
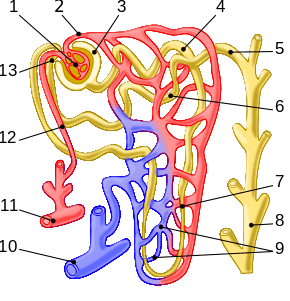
Nephron of the kidney. The labelled parts are 1. Glomerulus, 2. Efferent arteriole, 3. Bowman's capsule, 4. Proximal convoluted tubule, 5. Cortical collecting duct, 6. Distal convoluted tubule, 7. Loop of Henle, 8. Papillary duct, 9. Peritubular capillaries, 10. Arcuate vein, 11. Arcuate artery, 12. Afferent arteriole, 13. Juxtaglomerular apparatus. | |
| Details | |
| Precursor | Metanephric blastema (intermediate mesoderm) |
| System | Urinary system |
| Identifiers | |
| Latin | Nephroneum |
| MeSH | Nephrons |
| FMA | 17640 |
The nephron (from Greek νεφρός - nephros, meaning "kidney") is the basic structural and functional unit of the kidney.[1] Its chief function is to regulate the concentration of water and soluble substances like sodium salts by filtering the blood, reabsorbing what is needed and excreting the rest as urine. A nephron eliminates wastes from the body, regulates blood volume and blood pressure, controls levels of electrolytes and metabolites, and regulates blood pH. Its functions are vital to life and are regulated by the endocrine system by hormones such as antidiuretic hormone, aldosterone, and parathyroid hormone.[2] In humans, a normal kidney contains 800,000 to 1.5 million nephrons.[3]
Structure

Each nephron is composed of an initial filtering component (the "renal corpuscle") and a tubule specialized for reabsorption and secretion (the "renal tubule"). The renal corpuscle filters out solutes from the blood, delivering water and small solutes to the renal tubule for modification.
Renal corpuscle
Composed of a glomerulus and the Bowman's capsule, the renal corpuscle (or Malpighian corpuscle) is the beginning of the nephron. It is the nephron's initial filtering component.
The glomerulus is a capillary tuft that receives its blood supply from an afferent arteriole of the renal circulation. The glomerular blood pressure provides the driving force for water and solutes to be filtered out of the blood and into the space made by Bowman's capsule. The remainder of the blood (only approximately 1/5 of all plasma passing through the kidney is filtered through the glomerular wall into the Bowman's capsule) passes into the efferent arteriole. The diameter of efferent arterioles is smaller than that of afferent arterioles, increasing the hydrostatic pressure in the glomerulus.
The Bowman's capsule, also called the glomerular capsule, surrounds the glomerulus. It is composed of a visceral inner layer formed by specialized cells called podocytes, and a parietal outer layer composed of simple squamous epithelium. Fluids from blood in the glomerulus are filtered through the visceral layer of podocytes, resulting in the glomerular filtrate.
The glomerular filtrate next moves to the renal tubule, where it is further processed to form urine. The different stages of this fluid are collectively known as the tubular fluid.
Renal tubule
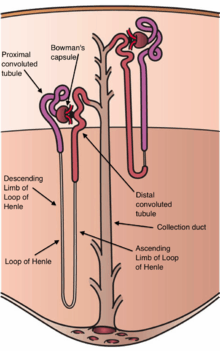
The renal tubule is the portion of the nephron containing the tubular fluid filtered through the glomerulus.[4] After passing through the renal tubule, the filtrate continues to the collecting duct system. [5]
The components of the renal tubule are:
- Proximal convoluted tubule (lies in cortex and lined by simple cuboidal epithelium with brush borders which help to increase the area of absorption greatly.)
- Loop of Henle (hair-pin like i.e. U-shaped and lies in medulla)
- Descending limb of loop of Henle
- Ascending limb of loop of Henle
- The ascending limb of loop of Henle is divided into 2 segments: Lower end of ascending limb is very thin and is lined by simple squamous epithelium. The distal portion of ascending limb is thick and is lined by simple cuboidal epithelium.
- Thin ascending limb of loop of Henle
- Thick ascending limb of loop of Henle (enters cortex and becomes DCT-distal convoluted tubule.)
- Distal convoluted tubule
Blood from the efferent arteriole, containing everything that was not filtered out in the glomerulus, moves into the peritubular capillaries, tiny blood vessels that surround the loop of Henle and the proximal and distal tubules, where the tubular fluid flows. Substances then reabsorb from the latter back to the blood stream.
The peritubular capillaries then recombine to form an efferent venule, which combines with efferent venules from other nephrons into the renal vein, and rejoins the main bloodstream.
Classes
The two general classes of nephrons are cortical nephrons and juxtamedullary nephrons, both of which are classified according to the length of their associated Loop of Henle and location of their renal corpuscle. All nephrons have their renal corpuscles in the cortex. Cortical nephrons have their Loop of Henle in the renal medulla near its junction with the renal cortex, while the Loop of Henle of juxtamedullary nephrons is located deep in the renal medulla; they are called juxtamedullary because their renal corpuscle is located near the medulla (but still in the cortex). The nomenclature for cortical nephrons varies, with some sources distinguishing between superficial cortical nephrons and midcortical nephrons, depending on where their corpuscle is located within the cortex.[6]
The majority of nephrons are cortical. Cortical nephrons have a shorter loop of Henle compared to juxtamedullary nephrons. The longer loop of Henle in juxtamedullary nephrons create a hyperosmolar gradient that allows for the creation of concentrated urine.[7]
The peritubular capillaries surround the proximal and distal tubules in both classes of nephrons. However, they surround the loop of Henle, forming the vasa recta, only in juxtamedullary nephrons and not in cortical nephrons.
Function

The nephron carries out nearly all of the kidney's functions. Most of these functions concern the reabsorption and secretion of various solutes such as ions (e.g., sodium), carbohydrates (e.g., glucose), and amino acids (e.g., glutamate). Properties of the cells that line the nephron change dramatically along its length; consequently, each segment of the nephron has highly specialized functions.
The proximal tubule as a part of the nephron can be divided into an initial convoluted portion and a following straight (descending) portion.[8] Fluid in the filtrate entering the proximal convoluted tubule is reabsorbed into the peritubular capillaries, including approximately two-thirds of the filtered salt and water and all filtered organic solutes (primarily glucose and amino acids).
The loop of Henle is a U-shaped tube that extends from the proximal tubule. It consists of a descending limb and an ascending limb. It begins in the cortex, receiving filtrate from the proximal convoluted tubule, extends into the medulla as the descending limb, and then returns to the cortex as the ascending limb to empty into the distal convoluted tubule. The primary role of the loop of Henle is to concentrate the salt in the interstitium, the tissue surrounding the loop.
Considerable differences aid in distinguishing the descending and ascending limbs of the loop of Henle. The descending limb is permeable to water and noticeably less impermeable to salt, and thus only indirectly contributes to the concentration of the interstitium. As the filtrate descends deeper into the hypertonic interstitium of the renal medulla, water flows freely out of the descending limb by osmosis until the tonicity of the filtrate and interstitium equilibrate. The hypertonicity of the medulla (and therefore concentration of urine) is determined in part by the size of the loop of Henle.
Unlike the descending limb, the thin ascending limb is impermeable to water, a critical feature of the countercurrent exchange mechanism employed by the loop. The ascending limb actively pumps sodium out of the filtrate, generating the hypertonic interstitium that drives countercurrent exchange. In passing through the ascending limb, the filtrate grows hypotonic since it has lost much of its sodium content. This hypotonic filtrate is passed to the distal convoluted tubule in the renal cortex.
The distal convoluted tubule has a different structure and function to that of the proximal convoluted tubule. Cells lining the tubule have numerous mitochondria to produce enough energy (ATP) for active transport to take place. Much of the ion transport taking place in the distal convoluted tubule is regulated by the endocrine system. In the presence of parathyroid hormone, the distal convoluted tubule reabsorbs more calcium and secretes more phosphate. When aldosterone is present, more sodium is reabsorbed and more potassium secreted. Atrial natriuretic peptide causes the distal convoluted tubule to secrete more sodium. In addition, the tubule also secretes hydronium and ammonium cations to regulate pH.
Collecting duct system
Each distal convoluted tubule delivers its filtrate to a system of collecting ducts, the first segment of which is the connecting tubule. The collecting duct system begins in the renal cortex and extends deep into the medulla. As the urine travels down the collecting duct system, it passes by the medullary interstitium which has a high sodium concentration as a result of the loop of Henle's countercurrent multiplier system.
Though the collecting duct is normally impermeable to water, it becomes permeable in the presence of antidiuretic hormone (ADH). ADH affects the function of aquaporins, resulting in the reabsorption of water molecules as it passes through the collecting duct. Aquaporins are membrane proteins that selectively conduct water molecules while preventing the passage of ions and other solutes. As much as three-quarters of the water from urine can be reabsorbed as it leaves the collecting duct by osmosis. Thus the levels of ADH determine whether urine will be concentrated or diluted. An increase in ADH is an indication of dehydration, while water sufficiency results in a decrease in ADH allowing for diluted urine.
Lower portions of the collecting organ are also permeable to urea, allowing some of it to enter the medulla of the kidney, thus maintaining its high concentration (which is very important for the nephron).
Urine leaves the medullary collecting ducts through the renal papillae, emptying into the renal calyces, the renal pelvis, and finally into the urinary bladder via the ureter.
Because it has a different origin during the development of the urinary and reproductive organs than the rest of the nephron, the collecting duct is sometimes not considered a part of the nephron. Instead of originating from the metanephrogenic blastema, the collecting duct originates from the ureteric bud.
Juxtaglomerular apparatus
The juxtaglomerular apparatus is a specialized region of the nephron responsible for production and secretion of the enzyme renin, involved in the renin-angiotensin system. This occurs near the site of contact between the thick ascending limb and the afferent arteriole. It contains three components: the macula densa, juxtaglomerular cells, and extraglomerular mesangial cells.
Clinical significance
Because of its importance in body fluid regulation, the nephron is a common target of drugs that treat high blood pressure and edema. These drugs, called diuretics, inhibit the ability of the nephron to retain electrolytes (and consequently water), thereby increasing the amount of urine produced. However, this clinical significance raises many concerns about treatments to such medical conditions. Because diuretics are drugs that stimulate the body's metabolism to higher intensities, primarily stimulating the heart, the clinical significance creates minor controversy considering how individuals with high blood pressure would avoid introducing medications that raise their already high blood pressure.
Other animals
The size and functioning of nephrons are said to vary from species to species[9] .
Additional images

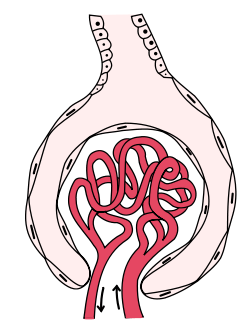 Glomerulus is red; Bowman's capsule is white.
Glomerulus is red; Bowman's capsule is white. Kidney tissue
Kidney tissue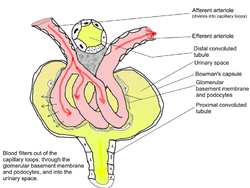 Glomerulus
Glomerulus This images shows the cells that make up a nephron in the kidneys. The following parts are seen: Lumen of a distal convoluted tubule (DCT), Macula densa, juxtaglomerular cells, lacis cells, mesangial cells, podocytes—visceral layer of Bowman’s capsule, parietal layer of Bowman’s capsule, lumen of a glomerular capillary, and the urinary space.
This images shows the cells that make up a nephron in the kidneys. The following parts are seen: Lumen of a distal convoluted tubule (DCT), Macula densa, juxtaglomerular cells, lacis cells, mesangial cells, podocytes—visceral layer of Bowman’s capsule, parietal layer of Bowman’s capsule, lumen of a glomerular capillary, and the urinary space.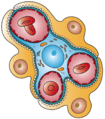 This image shows the types of cells present in the glomerulus part of a kidney nephron. Podocytes, Endothelial cells, and Glomerular mesangial cell are present.
This image shows the types of cells present in the glomerulus part of a kidney nephron. Podocytes, Endothelial cells, and Glomerular mesangial cell are present.
See also
References
- ↑ Pocock, G. Human Physiology.Oxford University Press.Third edition.2006. Page 349.
- ↑ Maton, Anthea; Jean Hopkins; Charles William McLaughlin; Susan Johnson; Maryanna Quon Warner; David LaHart; Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 0-13-981176-1.
- ↑ Guyton, Arthur C.; Hall, John E. (2006). Textbook of Medical Physiology. Philadelphia: Elsevier Saunders. p. 310. ISBN 0-7216-0240-1.
- ↑ Ecology & Evolutionary Biology - University of Colorado at Boulder. "The Kidney Tubule I: Urine Production." URL: http://www.colorado.edu/eeb/web_resources/cartoons/nephrex1.html. Accessed on: March 6, 2007. Archived October 2, 2007, at the Wayback Machine.
- ↑ Hook, Jerry B. & Goldstein, Robin S. (1993). Toxicology of the Kidney. Raven Press. p. 8. ISBN 0-88167-885-6.
- ↑ Physiology: 7/7ch03/7ch03p16 - Essentials of Human Physiology
- ↑ Jameson, J. Larry & Loscalzo, Joseph (2010). Harrison's Nephrology and Acid-Base Disorders. McGraw-Hill Professional. p. 3. ISBN 978-0-07-166339-7.
- ↑ Walter F. Boron. Medical Physiology: A Cellular And Molecular Approaoch. Elsevier/Saunders. p. 743. ISBN 1-4160-2328-3.
- ↑ Ganong. Ganong's Review of Medical Physioloy (24 ed.). TATA McGRAW HILL. p. 678. ISBN 978-1-25-902753-6.