Oral microbiology
Oral microbiology is the study of the microorganisms (microbiota) of the oral cavity and their interactions between oral microorganisms or with the host.[1] The environment present in the human mouth allows the growth of characteristic microorganisms found there. It provides a source of water and nutrients, as well as a moderate temperature.[2] Resident microbes of the mouth adhere to the teeth and gums to resist mechanical flushing from the mouth to stomach where acid-sensitive microbes are destroyed by hydrochloric acid.[2][3]
Anaerobic bacteria in the oral cavity include: Actinomyces, Arachnia, Bacteroides, Bifidobacterium, Eubacterium, Fusobacterium, Lactobacillus, Leptotrichia, Peptococcus, Peptostreptococcus, Propionibacterium, Selenomonas, Treponema, and Veillonella.[4] Genera of fungi that are frequently found in the mouth include Candida, Cladosporium, Aspergillus, Fusarium, Glomus, Alternaria, Penicillium, and Cryptococcus, among others.[5] Bacteria accumulate on both the hard and soft oral tissues in biofilms. Bacterial adhesion is particularly important for oral bacteria.
Oral bacteria have evolved mechanisms to sense their environment and evade or modify the host. Bacteria occupy the ecological niche provided by both the tooth surface and gingival epithelium. However, a highly efficient innate host defense system constantly monitors the bacterial colonization and prevents bacterial invasion of local tissues. A dynamic equilibrium exists between dental plaque bacteria and the innate host defense system.[6] Of particular interest is the role of oral microorganisms in the two major dental diseases: dental caries and periodontal disease.[6] Additionally, research has correlated poor oral heath and the resulting ability of the oral microbiota to invade the body to affect cardiac health as well as cognitive function.[7]
Oral bacteria

The environment present in the human mouth allows the growth of characteristic microorganisms found there. It provides a source of water and nutrients, as well as a moderate temperature.[2] Resident microbes of the mouth adhere to the teeth and gums to resist mechanical flushing from the mouth to stomach where acid-sensitive microbes are destroyed by hydrochloric acid.[2][3]
Anaerobic bacteria in the oral cavity include: Actinomyces, Arachnia, Bacteroides, Bifidobacterium, Eubacterium, Fusobacterium, Lactobacillus, Leptotrichia, Peptococcus, Peptostreptococcus, Propionibacterium, Selenomonas, Treponema, and Veillonella.[4]
The oral cavity of the new-born baby does not contain bacteria but rapidly becomes colonized with bacteria such as Streptococcus salivarius. With the appearance of the teeth during the first year colonization by Streptococcus mutans and Streptococcus sanguinis occurs as these organisms colonise the dental surface and gingiva. Other strains of streptococci adhere strongly to the gums and cheeks but not to the teeth. The gingival crevice area (supporting structures of the teeth) provides a habitat for a variety of anaerobic species. Bacteroides and spirochetes colonize the mouth around puberty.[6]
Of particular interest is the role of oral microorganisms in the two major dental diseases: dental caries and periodontal disease.[6]
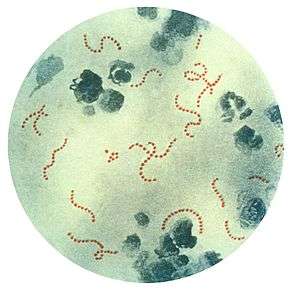
Fusospirochetes
Spirochetes and fusi-form bacilli live as normal flora in the mouth, but in the case of bleeding in the oral cavity, the bacteria can cause infection and diseases to oral cavity:
- Acute necrotizing ulcerative gingivitis (ANUG)
- Vincent angina with a membrane covering the throat area
Veillonella
Veillonella are gram-negative anaerobic cocci. It is thought that this species thrives in the acidic environment of caries and is thought to slow the development of dental caries. It converts the acidic products of other species to less acidic products.
Actinobacillus actinomycetemcomitans
Actinobacillus actinomycetemcomitans is considered an oral pathogen due to its virulence factors, its association with localized aggressive periodontitis in young adolescents, and studies indicating that it can cause bone loss.[9]
Lactobacillus
Some Lactobacillus species have been associated with dental cavities although these bacteria are normally symbiotic in humans and are found in the gut flora.[10]
Dental plaque
Dental plaque is the material that adheres to the teeth and consists of bacterial cells (mainly S. mutans and S. sanguis), salivary polymers and bacterial extracellular products. Plaque is a biofilm on the surfaces of the teeth. This accumulation of microorganisms subject the teeth and gingival tissues to high concentrations of bacterial metabolites which results in dental disease. If not taken care of, via brushing or flossing, the plaque can turn into tartar (its hardened form) and lead to gingivitis or periodontal disease.
Cell-cell communication
Most of the bacterial species found in the mouth belong to microbial communities, called biofilms, a feature of which is inter-bacterial communication. Cell-cell contact is mediated by specific protein adhesins and often, as in the case of inter-species aggregation, by complementary polysaccharide receptors. Another method of communication involves cell-cell signalling molecules, which are of two classes: those used for intra-species and those used for inter-species signalling. An example of intra-species communication is quorum sensing. Oral bacteria have been shown to produce small peptides, such as competence stimulating peptides, which can help promote single-species biofilm formation. A common form of inter-species signalling is mediated by 4, 5-dihydroxy-2, 3-pentanedione (DPD), also known as autoinducer-2 (Al-2).[11]
Vaccination against oral infections
In the case of dental caries, proteins involved in colonization of teeth by Streptococcus mutans can produce antibodies that inhibit the cariogenic process.[12]
Other microbiota
Bacteria species typically associated with oral flora have been found to be present in women with bacterial vaginosis.[13]
Genera of fungi that are frequently found in the mouth include Candida, Cladosporium, Aspergillus, Fusarium, Glomus, Alternaria, Penicillium, and Cryptococcus, among others.[5]
Role in non-oral disease
Additionally, research has correlated poor oral heath and the resulting ability of the oral microbiota to invade the body to affect cardiac health as well as cognitive function.[7]
See also
- Biofilms
- Dental plaque
- Environmental microbiology
- Human microbiota
- Human microbiome project
- Microbiology
- Theodor Rosebury
- List of bacterial vaginosis microbiota
References
- ↑ Schwiertz, Andreas (2016). Microbiota of the human body : implications in health and disease. Switzerland: Springer. p. 45. ISBN 978-3-319-31248-4.
- 1 2 3 4 Sherwood, Linda; Willey, Joanne; Woolverton, Christopher (2013). Prescott's Microbiology (9th ed.). New York: McGraw Hill. pp. 713–721. ISBN 9780073402406. OCLC 886600661.
- 1 2 Wang ZK, Yang YS, Stefka AT, Sun G, Peng LH (April 2014). "Review article: fungal microbiota and digestive diseases". Aliment. Pharmacol. Ther. 39 (8): 751–766. doi:10.1111/apt.12665. PMID 24612332.
In addition, GI fungal infection is reported even among those patients with normal immune status. Digestive system-related fungal infections may be induced by both commensal opportunistic fungi and exogenous pathogenic fungi. ... Candida sp. is also the most frequently identified species among patients with gastric IFI. ... It was once believed that gastric acid could kill microbes entering the stomach and that the unique ecological environment of the stomach was not suitable for microbial colonisation or infection. However, several studies using culture-independent methods confirmed that large numbers of acid-resistant bacteria belonging to eight phyla and up to 120 species exist in the stomach, such as Streptococcus sp., Neisseria sp. and Lactobacillus sp. etc.26, 27 Furthermore, Candida albicans can grow well in highly acidic environments,28 and some genotypes may increase the severity of gastric mucosal lesions.29
- 1 2 Sutter, V. L. (1984). "Anaerobes as normal oral flora". Reviews of infectious diseases. 6 Suppl 1: S62–S66. doi:10.1093/clinids/6.Supplement_1.S62. PMID 6372039.
- 1 2 Cui L, Morris A, Ghedin E (July 2013). "The human mycobiome in health and disease". Genome Med. 5 (7): 63. doi:10.1186/gm467. PMC 3978422
 . PMID 23899327.
. PMID 23899327. Figure 2: Distribution of fungal genera in different body sites
- 1 2 3 4 Rogers A H (editor). (2008). Molecular Oral Microbiology. Caister Academic Press. ISBN 978-1-904455-24-0.
- 1 2 Noble JM, Scarmeas N, Papapanou PN (2013). "Poor oral health as a chronic, potentially modifiable dementia risk factor: review of the literature.". Curr Neurol Neurosci Rep. 13 (10): 384. doi:10.1007/s11910-013-0384-x. PMID 23963608.
- ↑ Dorfman J, The Center for Special Dentistry.
- ↑ Fine DH, et al. (2008). "Molecular Windows into the Pathogenic Properties of Actinobacillus actinomycetemcomitans". Molecular Oral Microbiology. Caister Academic Press. ISBN 978-1-904455-24-0.
- ↑ Ljungh A, Wadstrom T (editors) (2009). Lactobacillus Molecular Biology: From Genomics to Probiotics. Caister Academic Press. ISBN 978-1-904455-41-7.
- ↑ Rickard A H (2008). "Cell-cell Communication in Oral Microbial Communities". Molecular Oral Microbiology. Caister Academic Press. ISBN 978-1-904455-24-0.
- ↑ Hajishengallis G, Russell MW (2008). "Molecular Approaches to Vaccination against Oral Infections". Molecular Oral Microbiology. Caister Academic Press. ISBN 978-1-904455-24-0.
- ↑ Africa, Charlene; Nel, Janske; Stemmet, Megan (2014). "Anaerobes and Bacterial Vaginosis in Pregnancy: Virulence Factors Contributing to Vaginal Colonisation". International Journal of Environmental Research and Public Health. 11 (7): 6979–7000. doi:10.3390/ijerph110706979. ISSN 1660-4601. PMC 4113856
 . PMID 25014248.
. PMID 25014248.
External links
| Wikispecies has information related to: Microbiota |