Laryngotracheal stenosis
| Laryngotracheal stenosis | |
|---|---|
 | |
| This condition can also be referred to as subglottic or tracheal stenosis. | |
| Classification and external resources | |
| Specialty | pulmonology |
| ICD-10 | Q31.1, Q32.1, J38.6, J39.8, J95.5 |
| ICD-9-CM | 519.19, 748.3 |
| MeSH | D014135 |
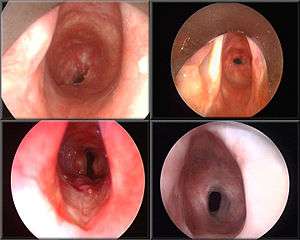
Laryngotracheal stenosis refers to abnormal narrowing of the central air passageways.[1] This can occur at the level of the larynx, trachea, carina or main bronchi.[2] In a small number of patients narrowing may be present in more than one anatomical location.
Nomenclature
Laryngotracheal stenosis (Laryngo-: Glottic Stenosis; Subglottic Stenosis; Tracheal: narrowings at different levels of the windpipe) is a more accurate description for this condition when compared, for example to subglottic stenosis which technically only refers to narrowing just below vocal folds or tracheal stenosis. In babies and young children however, the subglottis is the narrowest part of the airway and most stenoses do in fact occur at this level. Subglottic stenosis is often therefore used to describe central airway narrowing in children, and laryngotracheal stenosis is more often used in adults.
Causes
Laryngotracheal stenosis is an umbrella term for a wide and heterogeneous group of very rare conditions. The population incidence of adult post-intubation laryngotracheal stenosis which is the commonest benign sub-type of this condition is approximately 1 in 200,000 adults per year.[3] The main causes of adult laryngotracheal stenosis are:
| Benign causes | Malignant causes | |
|---|---|---|
| Extrinsic compression |
|
|
| Intrinsic narrowing |
|
|
Presentation
The most common symptom of laryngotracheal stenosis is gradually-worsening breathlessness (dyspnea) particularly when undertaking physical activities (exertional dyspnea). The patient may also experience added respiratory sounds which in the more severe cases can be identified as stridor but in many cases can be readily mistaken for wheeze. This creates a diagnostic pitfall in which many patients with laryngotracheal stenosis are incorrectly diagnosed as having asthma and are treated for presumed lower airway disease.[20][21] [22] [23] [24] .[25] This increases the likelihood of the patient eventually requiring major open surgery in benign disease [26] and can lead to tracheal cancer presenting too late for curative surgery to be performed.
Treatment
The optimal management of laryngotracheal stenosis is not well defined, depending mainly on the type of the stenosis.[27] General treatment options include
- Tracheal dilation using rigid bronchoscope
- Laser surgery and endoluminal stenting[28]
- Tracheal resection and reconstruction[17][29]
Tracheal dilation is used to temporarily enlarge the airway. The effect of dilation typically lasts from a few days to 6 months. Several studies have shown that as a result of mechanical dilation (used alone) may occur a high mortality rate and a rate of recurrence of stenosis higher than 90%.[27] Thus, many authors treat the stenosis by endoscopic excision with laser (commonly either the carbon dioxide or the neodymium: yttrium aluminum garnet laser) and then by using bronchoscopic dilatation and prolonged stenting with a T-tube (generally in silicone).[30][31][32]
There are differing opinions on treating with laser surgery.
In very experienced surgery centers, tracheal resection and reconstruction (anastomosis complete end-to-end with or without laryngotracheal temporary stent to prevent airway collapse) is currently the best alternative to completely cure the stenosis and allows to obtain good results. Therefore, it can be considered the gold standard treatment and is suitable for almost all patients.[33]
The narrowed part of the trachea will be cut off and the cut ends of the trachea sewn together with sutures. For stenosis of length greater than 5 cm a stent may be required to join the sections.
Late June or early July 2010, a new potential treatment was pioneered at Great Ormond Street Hospital in London, where Ciaran Finn-Lynch (aged 11) received a transplanted trachea which had been injected with stem cells harvested from his own bone marrow. The use of Ciaran's stem cells is hoped to prevent his immune system from rejecting the transplant.[34]
See also
- Hermes Grillo pioneer in tracheal resection surgery
References
- ↑ Gelbard, A (2014). "Causes and Consequences of Laryngotracheal Stenosis". The Laryngoscope. doi:10.1002/lary.24956.
- ↑ Armstrong WB, Netterville JL (August 1995). "Anatomy of the larynx, trachea, and bronchi". Otolaryngol. Clin. North Am. 28 (4): 685–99. PMID 7478631.
- ↑ Nouraei SA, Ma E, Patel A, Howard DJ, Sandhu GS (2007). "Estimating the population incidence of adult postintubation laryngotracheal stenosis". Clin Otolaryngol. 32: 411–412. doi:10.1111/j.1749-4486.2007.01484.x.
- 1 2 Lu MS, Liu YH, Ko PJ, Wu YC, Hsieh MJ, Liu HP, Lin PJ (April 2003). "Preliminary experience with bronchotherapeutic procedures in central airway obstruction". Chang Gung Med J. 26 (4): 240–9. PMID 12846523.
- ↑ Tsutsui H, Kubota M, Yamada M, Suzuki A, Usuda J, Shibuya H, Miyajima K, Sugino K, Ito K, Furukawa K, Kato H (September 2008). "Airway stenting for the treatment of laryngotracheal stenosis secondary to thyroid cancer". Respirology. 13 (5): 632–8. doi:10.1111/j.1440-1843.2008.01309.x. PMID 18513246.
- ↑ Peña J, Cicero R, Marín J, Ramírez M, Cruz S, Navarro F (October 2001). "Laryngotracheal reconstruction in subglottic stenosis: an ancient problem still present". Otolaryngol Head Neck Surg. 125 (4): 397–400. doi:10.1067/mhn.2001.117372. PMID 11593179.
- ↑ Bent J (July 2006). "Pediatric laryngotracheal obstruction: current perspectives on stridor". Laryngoscope. 116 (7): 1059–70. doi:10.1097/01.mlg.0000222204.88653.c6. PMID 16826038.
- ↑ Perkins JA, Inglis AF, Richardson MA (March 1998). "Iatrogenic airway stenosis with recurrent respiratory papillomatosis". Arch. Otolaryngol. Head Neck Surg. 124 (3): 281–7. doi:10.1001/archotol.124.3.281. PMID 9525512.
- ↑ Wood DE, Mathisen DJ (September 1991). "Late complications of tracheotomy". Clin. Chest Med. 12 (3): 597–609. PMID 1934960.
- ↑ Lorenz RR (December 2003). "Adult laryngotracheal stenosis: etiology and surgical management". Curr Opin Otolaryngol Head Neck Surg. 11 (6): 467–72. doi:10.1097/00020840-200312000-00011. PMID 14631181.
- ↑ Lebovics RS, Hoffman GS, Leavitt RY, Kerr GS, Travis WD, Kammerer W, Hallahan C, Rottem M, Fauci AS (December 1992). "The management of subglottic stenosis in patients with Wegener's granulomatosis". Laryngoscope. 102 (12 Pt 1): 1341–5. doi:10.1288/00005537-199212000-00005. PMID 1453838.
- ↑ Hoffman GS, Thomas-Golbanov CK, Chan J, Akst LM, Eliachar I (May 2003). "Treatment of subglottic stenosis, due to Wegener's granulomatosis, with intralesional corticosteroids and dilation". J. Rheumatol. 30 (5): 1017–21. PMID 12734898.
- ↑ Gluth MB, Shinners PA, Kasperbauer JL (August 2003). "Subglottic stenosis associated with Wegener's granulomatosis". Laryngoscope. 113 (8): 1304–7. doi:10.1097/00005537-200308000-00008. PMID 12897550.
- ↑ Wester JL, Clayburgh DR, Stott WJ, Schindler JS, Andersen PE, Gross ND (December 2011). "Airway reconstruction in Wegener's granulomatosis-associated laryngotracheal stenosis". Laryngoscope. 121 (12): 2566–71. doi:10.1002/lary.22367. PMID 22109754.
- ↑ Chang SJ, Lu CC, Chung YM, Lee SS, Chou CT, Huang DF (June 2005). "Laryngotracheal involvement as the initial manifestation of relapsing polychondritis". J Chin Med Assoc. 68 (6): 279–82. doi:10.1016/S1726-4901(09)70151-0. PMID 15984823.
- ↑ Kim CM, Kim BS, Cho KJ, Hong SJ (April 2003). "Laryngotracheal involvement of relapsing polychondritis in a Korean girl". Pediatr. Pulmonol. 35 (4): 314–7. doi:10.1002/ppul.10247. PMID 12629631.
- 1 2 Mostafa BE, El Fiky L, El Sharnoubi M (July 2006). "Non-intubation traumatic laryngotracheal stenosis: management policies and results". Eur Arch Otorhinolaryngol. 263 (7): 632–6. doi:10.1007/s00405-006-0036-8. PMID 16633824.
- ↑ Kokturk N, Demircan S, Kurul C, Turktas H (October 2004). "Tracheal adenoid cystic carcinoma masquerading asthma: a case report". BMC Pulm Med. 4: 10. doi:10.1186/1471-2466-4-10. PMC 526771
 . PMID 15494074.
. PMID 15494074. - ↑ Wassermann K, Mathen F, Edmund Eckel H (October 2000). "Malignant laryngotracheal obstruction: a way to treat serial stenoses of the upper airways". Ann. Thorac. Surg. 70 (4): 1197–201. doi:10.1016/s0003-4975(00)01614-3. PMID 11081870.
- ↑ Catenacci MH (July 2006). "A case of laryngotracheal stenosis masquerading as asthma". South. Med. J. 99 (7): 762–4. doi:10.1097/01.smj.0000217498.70967.77. PMID 16866062.
- ↑ Ricketti PA, Ricketti AJ, Cleri DJ, Seelagy M, Unkle DW, Vernaleo JR (2010). "A 41-year-old male with cough, wheeze, and dyspnea poorly responsive to asthma therapy". Allerg Asthma Proc. 31: 355–8. doi:10.2500/aap.2010.31.3344.
- ↑ Scott PM, Glover GW (1995). "All that wheezes is not asthma". Br J Clin Pract. 49: 43–4.
- ↑ Kokturk N, Demircan S, Kurul C, Turktas H (2004). "Tracheal adenoid cystic carcinoma masquerading asthma: a case report". BMC Pulm Med. 4: 10.
- ↑ Parrish RW, Banks J, Fennerty AG (1983). "Tracheal obstruction presenting as asthma". Postgrad Med J. 59: 775–6. doi:10.1136/pgmj.59.698.775.
- ↑ Galvin IF, Shepherd DR, Gibbons JR (1990). "Tracheal stenosis caused by congenital vascular ring anomaly misinterpreted as asthma for 45 years". Thorac Cardiovasc Surg. 38: 42–4. doi:10.1055/s-2007-1013990.
- ↑ Nouraei SA, Singh A, Patel A, Ferguson C, Howard DJ, Sandhu GS (2006). "Early endoscopic treatment of acute inflammatory airway lesions improves the outcome of postintubation airway stenosis". Laryngoscope. 116 (8): 1417–21. doi:10.1097/01.mlg.0000225377.33945.14.
- 1 2 Brichet A, Verkindre C, Dupont J, Carlier ML, Darras J, Wurtz A, Ramon P, Marquette CH (April 1999). "Multidisciplinary approach to management of postintubation tracheal stenoses". Eur. Respir. J. 13 (4): 888–93. doi:10.1034/j.1399-3003.1999.13d32.x. PMID 10362058.
- ↑ Ciccone AM, De Giacomo T, Venuta F, Ibrahim M, Diso D, Coloni GF, Rendina EA (October 2004). "Operative and non-operative treatment of benign subglottic laryngotracheal stenosis". Eur J Cardiothorac Surg. 26 (4): 818–22. doi:10.1016/j.ejcts.2004.06.020. PMID 15450579.
- ↑ Duncavage JA, Koriwchak MJ (August 1995). "Open surgical techniques for laryngotracheal stenosis". Otolaryngol. Clin. North Am. 28 (4): 785–95. PMID 7478638.
- ↑ Shapshay SM, Beamis JF, Hybels RL, Bohigian RK (1987). "Endoscopic treatment of subglottic and tracheal stenosis by radial laser incision and dilation". Ann. Otol. Rhinol. Laryngol. 96 (6): 661–4. doi:10.1177/000348948709600609. PMID 3688753.
- ↑ Shapshay SM, Beamis JF, Dumon JF (November 1989). "Total cervical tracheal stenosis: treatment by laser, dilation, and stenting". Ann. Otol. Rhinol. Laryngol. 98 (11): 890–5. doi:10.1177/000348948909801110. PMID 2817681.
- ↑ Mehta AC, Lee FY, Cordasco EM, Kirby T, Eliachar I, De Boer G (September 1993). "Concentric tracheal and subglottic stenosis. Management using the Nd-YAG laser for mucosal sparing followed by gentle dilatation". Chest. 104 (3): 673–7. doi:10.1378/chest.104.3.673. PMID 8365273.
- ↑ Gómez-Caro A, Morcillo A, Wins R, Molins L, Galan G, Tarrazona V (January 2011). "Surgical management of benign tracheal stenosis". Multimed Man Cardiothorac Surg. 2011 (1111): mmcts.2010.004945. doi:10.1510/mmcts.2010.004945. PMID 24413853.
- ↑ "New throat surgery 'a success'". BBC News. 2010-08-06.
- Bibliography
- Ongkasuwan, Julina (2006-02-09). "Tracheal Stenosis". Baylor College of Medicine. Archived from the original on 2007-02-20. Retrieved 2007-03-17.