Vegan nutrition

Vegan nutrition refers to the nutritional aspects of vegan diets – diets which include no animal products.
While a well-planned, balanced vegan diet is suitable to meet all recommendations for nutrients in every stage of life, improperly-planned vegan diets may be deficient in vitamin B12, vitamin D, calcium, iodine, iron, zinc, riboflavin (vitamin B2), long-chain fatty acids EPA and DHA, and omega-3 fatty acids.[1]
Background
Doctors Dean Ornish, T. Colin Campbell, John A. McDougall, Michael Klaper, Caldwell Esselstyn, Michael Greger, Joel Fuhrman, and Neal D. Barnard claim that high animal fat and protein diets, such as the standard American diet, are detrimental to health.[2][3][4] They also state that a lifestyle change incorporating a vegan whole foods diet could not only prevent various degenerative diseases, such as coronary artery disease, but reverse them.[5][6][7][8][9] A number of documentary films, such as Fat, Sick and Nearly Dead, Planeat and Forks over Knives, focus on the purported health benefits of plant-based diets. Although there is general consensus amongst doctors advocating plant-based diets, Joel Fuhrman and Michael Greger have disagreed with Campbell and Esselstyn on the use of nuts and seeds.[10]
Some athletes, such as Brendan Brazier, follow a vegan diet, including raw veganism.[11] Vegan diets tend to be higher in dietary fibre, magnesium, folic acid, vitamin C, vitamin E, iron, and phytochemicals, and lower in calories, saturated fat, cholesterol, long-chain omega-3 fatty acids, vitamin D, calcium, zinc, and vitamin B12.[12] Because uncontaminated plant foods do not provide vitamin B12 (which is produced by microorganisms such as bacteria), researchers agree that vegans should eat foods fortified with B12 or take a daily supplement.[13]
Nutrition
The American Dietetic Association and Dietitians of Canada state that well-planned vegan diets can meet all nutrient requirements and are appropriate for all stages of the life cycle, including during pregnancy, lactation, infancy, childhood, and adolescence.[14] Poorly planned vegan diets may be low in vitamin B12, omega-3 fatty acids, vitamin D, calcium, iron, zinc, riboflavin (vitamin B2), and iodine.
Vitamin B12
Vitamin B12 deficiency is potentially extremely serious, leading to megaloblastic anemia, nerve degeneration and irreversible neurological damage.[15]
Evidence suggests that vegans who are not taking vitamin B12 supplements do not consume sufficient servings of B12 and often have abnormally low blood concentrations of vitamin B12.[16] This is because, unless fortified, plant foods do not contain reliable amounts of active vitamin B12. Vegans are recommended to do one of the following dietary options:[17]
- Consume fortified foods 2-3 times per day to get at least 3 micrograms of vitamin B12,
- or take 1 vitamin B12 supplement per day to get at least 10 micrograms
- or take 1 weekly B12 supplement to get a least 2000 micrograms.
Protein
Proteins are composed of amino acids and essential amino acids cannot be synthesised by the human body. A 1994 study found a varied intake of such sources can be adequate.[18]
Omega-3 fatty acids

Vegan diets can be low in omega-3 fatty acids (O3FA). Major vegan sources of O3FA include algae, hempseeds and hempseed oil, walnuts, flaxseeds and flaxseed oil, olive oil, canola (rapeseed) oil, avocado and chia seeds. However, diets lacking generous amounts of sea vegetables (seaweed) generally lack a direct source of long-chain O3FA such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Vegan diets, like the standard American diet, may also have a high ratio of O6FA to O3FA, which inhibits the conversion of short-chain fatty acids such as alpha-Linolenic acid (ALA), found in most vegan O3FA sources, to EPA and DHA.[1] Short-term supplemental ALA has been shown to increase EPA levels but not DHA levels, suggesting poor conversion of the intermediary EPA to DHA.[19] DHA supplements derived from DHA-rich microalgae are available,[1] and the human body can also convert DHA to EPA.[20]

There is only weak evidence that omega-3 benefits cardiovascular health,[21] and although omega-3 has previously been thought useful for helping alleviate dementia, as of 2016 there is no good evidence of effectiveness.[22]
While there is little evidence of adverse health or cognitive effects due to DHA deficiency in adult vegetarians or vegans, fetal and breast milk levels remain a concern.[19] EPA and DHA supplementation has been shown to reduce platelet aggregation in vegetarians, but a direct link to cardiovascular morbidity and mortality, which is already lower for vegetarians, has yet to be determined.[23]
Calcium
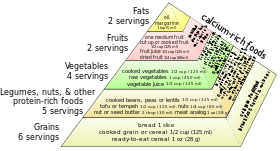
It is recommended that vegans eat three servings per day of a high-calcium food, such as fortified soy milk, almonds, hazelnuts, kale, collard greens, Chinese greens, and take a calcium supplement or other calcium-fortified foods as necessary.[1]
Many studies have examined possible correlation between veganism, calcium intake, and bone health. The EPIC-Oxford study suggested that vegans who consumed 525 mg or less of calcium per day have an increased risk of bone fractures over meat eaters and vegetarians, but that vegans consuming more than 525 mg/day had a risk of fractures similar to other groups. Overall, the entire group of vegans had a higher risk of fractures.[24] A 2009 study of bone density found the bone density of vegans was 94 percent that of omnivores, but deemed the difference clinically insignificant.[25] Another study in 2009 by the same researchers examined over 100 vegan post-menopausal women, and found that their diet had no adverse effect on bone mineral density (BMD) and no alteration in body composition.[26] Biochemist T. Colin Campbell suggested in The China Study (2005) that osteoporosis is linked to the consumption of animal protein because, unlike plant protein, animal protein increases the acidity of blood and tissues, which is then neutralized by calcium pulled from the bones resulting in hypercalciuria. Campbell wrote that his China-Oxford-Cornell study of nutrition in the 1970s and 1980s found that, in rural China, "where the animal to plant ratio [for protein] was about 10 percent, the fracture rate is only one-fifth that of the U.S."[27]
Calcium is one component of the most common type of human kidney stones, calcium oxalate. Some studies suggest that people who take supplemental calcium have a higher risk of developing kidney stones, and these findings have been used as the basis for setting the recommended daily intake (RDI) for calcium in adults.[28][29][30]
Iodine
One study reported a "potential danger of iodine deficiency disorders due to strict forms of vegetarian nutrition, especially when fruits and vegetables grown in soils with low [iodine] levels are ingested."[31]
Iron
It is recommended for vegans to eat iron-rich foods and vitamin C daily.[32] In several studies, vegans were not found to suffer from iron-deficiency any more than non-vegans.[33][34][35][36] However, due to the low absorption rate on non-heme iron it is recommended to eat dark leafy greens (and other sources of iron) together with sources of Vitamin C.[37]
Choline
It is recommended for vegans to eat food rich in choline, as plant based sources of choline are limited.[38] Soy lecithin, cauliflower, spinach, wheat germ, firm tofu, kidney beans, quinoa and amaranth are vegan sources of choline. The Adequate Intake (AI) of choline is 425 mg (milligrams) per day for adult women; higher for pregnant and breastfeeding women. The AI for adult men is 550 mg/day.[39] Choline deficiency can lead to health problems such as liver damage, a result of liver cells initiating programmed cell death (apoptosis), as well as an increase in neural tube defects in pregnant women.[40] In a study, 77% of men, 44% of premenopausal women, and 80% of postmenopausal women developed fatty liver or muscle damage due to choline deficiency, showing that subject characteristics regulate the dietary requirement.[41] Choline deficiency has also been associated with hypertension in rats.[42] There is also some evidence that choline is an anti-inflammatory as well, but further studies are needed to confirm/refute findings.[43] In order to avoid these problems, it's important to meet the adequate intake, especially since many multivitamins do not contain enough choline.[44] Although many animal products, like liver and egg, contain high amounts of choline (355 mg/3 oz and 126 mg/large egg, respectively), wheat germ (172 mg/cup), brussel sprouts (63 mg/cup), and broccoli (62 mg/cup) are good sources of choline as well.[40]
See also
References
- 1 2 3 4 For an overview, see:
- American Dietetic, Association; Dietitians Of, Canada (2003). "Position of the American Dietetic Association and Dietitians of Canada : Vegetarian Diets". Canadian Journal of Dietetic Practice and Research. 64 (2): 62–81. doi:10.3148/64.2.2003.62. PMID 12826028.
- Key, Timothy J.; Appleby, Paul N.; Rosell, Magdalena S. (2007). "Health effects of vegetarian and vegan diets". Proceedings of the Nutrition Society. 65 (1): 35–41. doi:10.1079/PNS2005481. PMID 16441942.
- For vitamin D and calcium: Appleby, P; Roddam, A; Allen, N; Key, T (2007). "Comparative fracture risk in vegetarians and nonvegetarians in EPIC-Oxford". European Journal of Clinical Nutrition. 61 (12): 1400–6. doi:10.1038/sj.ejcn.1602659. PMID 17299475.
- For iron: "Iron deficiency—adults". Better Health Channel. Government of Victoria, Australia. Retrieved February 4, 2011.
High-risk groups such as vegetarians, adolescent girls and women athletes need to eat iron-rich foods each day (combined with foods that are high in vitamin C). …Vegetarians who exclude all animal products from their diet may need almost twice as much dietary iron each day as non-vegetarians. Sources include dark green leafy vegetables—such as spinach—and raisins, nuts, seeds, beans, peas, and iron-fortified cereals, breads and pastas.
- ↑ Segelken, Roger (2001-06-28). "China Study II: Switch to Western diet may bring Western-type diseases". Cornell Chronicle. Retrieved 2006-09-15.
- ↑ "China-Cornell-Oxford Project On Nutrition, Environment and Health at Cornell University". Division of Nutritional Sciences. Cornell University. Retrieved 2006-09-15.
- ↑ Barnard, Neal D. (2007). Dr. Neal Barnard's Program for Reversing Diabetes. New York: Rodale. pp. 40–50.
Set aside animal products
- ↑ Ornish, D.; Brown, S.E.; Billings, J.H.; Scherwitz, L.W.; Armstrong, W.T.; Ports, T.A.; McLanahan, S.M.; Kirkeeide, R.L.; Gould, K.L.; et al. (1990). "Can lifestyle changes reverse coronary heart disease?". The Lancet. 336 (8708): 129–33. doi:10.1016/0140-6736(90)91656-U. PMID 1973470.
- ↑ Goldhamer, Alan C.; Lisle, Douglas J.; Sultana, Peter; Anderson, Scott V.; Parpia, Banoo; Hughes, Barry; Campbell, T. Colin (2002). "Medically Supervised Water-Only Fasting in the Treatment of Borderline Hypertension". The Journal of Alternative and Complementary Medicine. 8 (5): 643–50. doi:10.1089/107555302320825165. PMID 12470446.
- ↑ McDougall, John; Bruce, Bonnie; Spiller, Gene; Westerdahl, John; McDougall, Mary (2002). "Effects of a Very Low-Fat, Vegan Diet in Subjects with Rheumatoid Arthritis". The Journal of Alternative and Complementary Medicine. 8 (1): 71–5. doi:10.1089/107555302753507195. PMID 11890437.
- ↑ Esselstyn, Caldwell B (1999). "Updating a 12-year experience with arrest and reversal therapy for coronary heart disease (an overdue requiem for palliative cardiology)". The American Journal of Cardiology. 84 (3): 339–41, A8. doi:10.1016/S0002-9149(99)00290-8. PMID 10496449.
- ↑ Barnard, N. D.; Cohen, J; Jenkins, DJ; Turner-Mcgrievy, G; Gloede, L; Jaster, B; Seidl, K; Green, AA; Talpers, S (2006). "A Low-Fat Vegan Diet Improves Glycemic Control and Cardiovascular Risk Factors in a Randomized Clinical Trial in Individuals with Type 2 Diabetes". Diabetes Care. 29 (8): 1777–83. doi:10.2337/dc06-0606. PMID 16873779.
- ↑ "The Diet Wars: The Time for Unification Is Now" (PDF). The McDougall Newsletter (Volume 11, Issue 8). August 2012.
- ↑ Berry 2007, pp. 604–605:
- "Despite the seeming hardships a vegan diet imposes on its practitioners, veganism is a burgeoning movement, especially among younger Americans. In the endurance sports, such as the Ironman triathlon and the Utramarathon, the top competitors are vegans who consume much of their vegan food in its uncooked state. Even young weight lifters and body builders are gravitating to a vegan diet, giving the lie to the notion that eating animal flesh is essential for strength and stamina. Brendan Brazier, a young athlete who regularly places in the top three in international triathlon events and who formulated Vega, a line of plant-based performance products, said of his fellow vegan athletes: 'We're beginning to build a strong presence in every sport.'"
- Also see Nijjar, Raman. "From pro athletes to CEOs and doughnut cravers, the rise of the vegan diet", CBC News, June 4, 2011.
- For other examples of Ironman triathlon athletes who are vegan, see Scott, David and Heidrich, Ruth. "Vegetarian/Vegan Ironman and Ironlady", European Vegetarian Union News, issue 4, 1997.
- ↑ Craig, Winston J. "Health effects of vegan diets", The American Journal of Clinical Nutrition, 89(5), May 2009, pp. 1627S–1633S (review article).
- ↑ Mangels, Reed; Messina, Virginia; and Messina, Mark. "Vitamin B12 (Cobalamin)," The Dietitian's Guide to Vegetarian Diets. Jones & Bartlett Learning, 2011, pp. 181–192.
- Mangels, Reed. "Vitamin B12 in the Vegan Diet", Vegetarian Resource Group, accessed December 17, 2012: "Vitamin B12 is needed for cell division and blood formation. Neither plants nor animals make vitamin B12. Bacteria are responsible for producing vitamin B12. Animals get their vitamin B12 from eating foods contaminated with vitamin B12 and then the animal becomes a source of vitamin B12. Plant foods do not contain vitamin B12 except when they are contaminated by microorganisms or have vitamin B12 added to them. Thus, vegans need to look to fortified foods or supplements to get vitamin B12 in their diet."
- Herbert, Victor. "Vitamin B12: plant sources, requirements and assay", American Journal of Clinical Nutrition, 48(3), September 1988, pp. 852–858.
- "Vitamin B12", Office of Dietary Supplements, National Institutes of Health, accessed December 17, 2012.
- Norris, Jack. "Vitamin B12: Are you getting it?", Vegan Outreach, July 26, 2006: "Contrary to the many rumors, there are no reliable, unfortified plant sources of vitamin B12 ... [There is an] overwhelming consensus in the mainstream nutrition community, as well as among vegan health professionals, that vitamin B12 fortified foods or supplements are necessary for the optimal health of vegans, and even vegetarians in many cases. Luckily, vitamin B12 is made by bacteria such that it does not need to be obtained from animal products."
- ↑ "Position of the American Dietetic Association and Dietitians of Canada: vegetarian diets", Canadian Journal of Dietetic Practice and Research, Summer 2003, 64(2), pp. 62–81 (also available here).
- ↑ C., Robert; Brown, David (2003-03-01). "Vitamin B12 Deficiency". 67 (5): 979–986.
- ↑ Krajčovičová-Kudláčková, M.; Blažíček, P.; Kopčová, J.; Béderová, A.; Babinská, K. (2000). "Homocysteine Levels in Vegetarians versus Omnivores". Annals of Nutrition and Metabolism. 44 (3): 135–8. doi:10.1159/000012827. PMID 11053901.
- ↑ "What Every Vegan Should Know About Vitamin B12". Retrieved 2015-08-05.
- ↑ VR Young and PL Pellett (1994). "Plant proteins in relation to human protein and amino acid nutrition". Am. J. Clinical Nutrition. 59 (5 Suppl): 1203S–1212S. PMID 8172124.
- 1 2 Sanders, Thomas A.B. (2009). "DHA status of vegetarians". Prostaglandins, Leukotrienes and Essential Fatty Acids. 81 (2–3): 137–41. doi:10.1016/j.plefa.2009.05.013. PMID 19500961.
- ↑ Bouchez, Colette. "Good Fat, Bad Fat: The Facts About Omega-3". WebMD.
- ↑ Colussi G, Catena C, Novello M, Bertin N, Sechi LA (2016). "Impact of omega-3 polyunsaturated fatty acids on vascular function and blood pressure: Relevance for cardiovascular outcomes". Nutr Metab Cardiovasc Dis (Review). doi:10.1016/j.numecd.2016.07.011. PMID 27692558.
- ↑ Burckhardt M, Herke M, Wustmann T, Watzke S, Langer G, Fink A (2016). "Omega-3 fatty acids for the treatment of dementia". Cochrane Database Syst Rev (Systematic review). 4: CD009002. doi:10.1002/14651858.CD009002.pub3. PMID 27063583.
- ↑ Mezzano, Diego; Kosiel, Karin; Martínez, Carlos; Cuevas, Ada; Panes, Olga; Aranda, Eduardo; Strobel, Pablo; Pérez, Druso D; Pereira, Jaime; et al. (2000). "Cardiovascular Risk Factors in Vegetarians: Normalization of Hyperhomocysteinemia with Vitamin B12 and Reduction of Platelet Aggregation with n-3 Fatty Acids". Thrombosis Research. 100 (3): 153–60. doi:10.1016/S0049-3848(00)00313-3. PMID 11108902.
- ↑ Appleby, P; Roddam, A; Allen, N; Key, T (2007). "Comparative fracture risk in vegetarians and nonvegetarians in EPIC-Oxford". European Journal of Clinical Nutrition. 61 (12): 1400–6. doi:10.1038/sj.ejcn.1602659. PMID 17299475.
- ↑ Ho-Pham, L. T; Nguyen, N. D; Nguyen, T. V (2009). "Effect of vegetarian diets on bone mineral density: A Bayesian meta-analysis". American Journal of Clinical Nutrition. 90 (4): 943–50. doi:10.3945/ajcn.2009.27521. PMID 19571226.
- ↑ Ho-Pham, L. T.; Nguyen, P. L. T.; Le, T. T. T.; Doan, T. A. T.; Tran, N. T.; Le, T. A.; Nguyen, T. V. (2009). "Veganism, bone mineral density, and body composition: A study in Buddhist nuns". Osteoporosis International. 20 (12): 2087–93. doi:10.1007/s00198-009-0916-z. PMID 19350341.
- ↑ Campbell, T. Colin. The China Study. Benbella Books, 2006, pp. 205–208.
- ↑ Brody, Jane E. (May 8, 1990). "Huge Study Of Diet Indicts Fat And Meat". The New York Times.
- ↑ Junshi, Chen; Campbell, T. Colin; Li; et al., eds. (1990). Diet, lifestyle, and mortality in China: a study of the characteristics of 65 Chinese counties. Oxford University Press. ISBN 978-0-19-261843-6.
- ↑ Byers, Tim (1992-05-15). "Book Reviews: Diet, lifestyle, and mortality in China: a study of the characteristics of 65 Chinese counties". American Journal of Epidemiology. 135 (10): 1180–1.
- ↑ Remer, Thomas; Neubert, Annette; Manz, Friedrich (1999). "Increased risk of iodine deficiency with vegetarian nutrition". British Journal of Nutrition. 81 (1): 45–9. doi:10.1017/s0007114599000136. PMID 10341675.
- ↑ "Iron deficiency—adults".
High-risk groups such as vegetarians, adolescent girls and women athletes need to eat iron-rich foods each day (combined with foods that are high in vitamin C). ... Vegetarians who exclude all animal products from their diet may need almost twice as much dietary iron each day as non-vegetarians. Sources include dark green leafy vegetables—such as spinach—and raisins, nuts, seeds, beans, peas, and iron-fortified cereals, breads and pastas
- ↑ Larsson, CL; Johansson, GK (2002). "Dietary intake and nutritional status of young vegans and omnivores in Sweden". The American Journal of Clinical Nutrition. 76 (1): 100–6. PMID 12081822.
- ↑ Messina, MJ; Messina, VL (1996). The Dietitian's Guide to Vegetarian Diets: Issues and Applications. Gaithersburg, MD: Aspen Publishers.
- ↑ Craig, WJ (1994). "Iron status of vegetarians". The American Journal of Clinical Nutrition. 59 (5 Suppl): 1233S–1237S. PMID 8172127.
- ↑ Ball, MJ; Bartlett, MA (1999). "Dietary intake and iron status of Australian vegetarian women". The American Journal of Clinical Nutrition. 70 (3): 353–8. PMID 10479197.
- ↑ Hallberg, L; Brune, M; Rossander, L (1989). "The role of vitamin C in iron absorption". International journal for vitamin and nutrition research. Supplement = Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Supplement. 30: 103–8. PMID 2507689.
The key role of ascorbic acid for the absorption of dietary nonheme iron is generally accepted. The reasons for its action are twofold: (1) the prevention of the formation of insoluble and unabsorbable iron compounds and (2) the reduction of ferric to ferrous iron, which seems to be a requirement for the uptake of iron into the mucosal cells.
- ↑ Entry for "Beans, kidney, all types, mature seeds, cooked, boiled, without salt" in the USDA Nutrients database
- ↑ http://www.iom.edu/Activities/Nutrition/SummaryDRIs/~/media/Files/Activity%20Files/Nutrition/DRIs/DRI_Vitamins.ashx[]
- 1 2 Higdon, Jane (Nov 2003). "Choline". Linus Pauling Institute at Oregon State University. Retrieved 3 March 2014.
- ↑ Fischer, Leslie M.; DaCosta, Kerry A.; Kwock, Lester; Stewart, Paul W.; Lu, Tsui-Shan; Stabler, Sally P.; Allen, Robert H.; Zeisel, Steven H. (May 2007). "Sex and Menopausal Status Influence Human Dietary Requirements for the Nutrient Choline". American Journal of Clinical Nutrition. Retrieved 3 March 2014.
- ↑ Kratzing, C.C.; Perry, J.J. (1 Dec 1971). "Hypertension in Young Rats Following Choline Deficiency in Maternal Diets" (PDF). The Journal of Nutrition.
- ↑ Paraskevi, Detopoulou; Panagiotakos, Demosthenes B.; Antonopoulou, Smaragdi; Pitsavos, Christos; Stefanadis, Christodoulos (5 Sep 2007). "Dietary Choline and Betaine Intakes in Relation to Concentrations of Inflammatory Markers in Healthy Adults: The ATTICA Study". American Society for Nutrition. Retrieved 3 March 2014.
- ↑ McCord, BreAnn. "Multivitamins Lack Choline". Beloit College.
Further reading
1980s
- John Robbins (1987) Diet for a New America
- Michael Klaper (1987) Vegan Nutrition
1990s
- Dean Ornish (1996) Dr. Dean Ornish's Programme for Reversing Heart Disease
- John A. McDougall (1996) The McDougall Program for a Healthy Heart
2000s
- Physicians Committee for Responsible Medicine (2002) Healthy Eating for Life to Prevent and Treat Cancer
- Joel Fuhrman (2003) Eat to Live
- T. Colin Campbell (2005) The China Study
- Michael Greger (2005) Carbophobia!
- Will Tuttle (2005) World Peace Diet
- Neal D. Barnard (2007) Dr. Neal Barnard's Program for Reversing Diabetes
- Caldwell Esselstyn (2008) Prevent and Reverse Heart Disease
- Barnard, Neal D; Cohen, Joshua; Jenkins, David JA; Turner-Mcgrievy, Gabrielle; Gloede, Lise; Green, Amber; Ferdowsian, Hope (2009). "A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: A randomized, controlled, 74-wk clinical trial". American Journal of Clinical Nutrition. 89 (5): 1588S–1596S. doi:10.3945/ajcn.2009.26736H. PMC 2677007
 . PMID 19339401.
. PMID 19339401. - Jacobs, David R; Gross, Myron D; Tapsell, Linda C (2009). "Food synergy: An operational concept for understanding nutrition". American Journal of Clinical Nutrition. 89 (5): 1543S–1548S. doi:10.3945/ajcn.2009.26736B. PMC 2731586
 . PMID 19279083.
. PMID 19279083. - Fraser, Gary E (2009). "Vegetarian diets: What do we know of their effects on common chronic diseases?". American Journal of Clinical Nutrition. 89 (5): 1607S–1612S. doi:10.3945/ajcn.2009.26736K. PMC 2677008
 . PMID 19321569.
. PMID 19321569.