Erlotinib
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tarceva |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605008 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral tablets |
| ATC code | L01XE03 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 59% |
| Protein binding | 95% |
| Metabolism | Hepatic (mainly CYP3A4, less CYP1A2) |
| Biological half-life | 36.2 hrs (median) |
| Excretion | >98% as metabolites, of which >90% via faeces, 9% via urine |
| Identifiers | |
| |
| CAS Number |
183321-74-6 |
| PubChem (CID) | 176870 |
| IUPHAR/BPS | 4920 |
| DrugBank |
DB00530 |
| ChemSpider |
154044 |
| UNII |
J4T82NDH7E |
| KEGG |
D07907 |
| ChEBI |
CHEBI:114785 |
| ChEMBL |
CHEMBL553 |
| ECHA InfoCard | 100.216.020 |
| Chemical and physical data | |
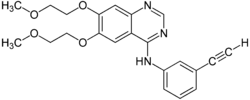
| Formula | C22H23N3O4 |
| Molar mass | 393.436 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| (verify) | |
Erlotinib hydrochloride (trade name Tarceva) is a drug used to treat non-small cell lung cancer (NSCLC), pancreatic cancer and several other types of cancer. It is a receptor tyrosine kinase inhibitor, which acts on the epidermal growth factor receptor (EGFR).
It is marketed in the United States by Genentech and OSI Pharmaceuticals and elsewhere by Roche. In the United States as of 2015 one 150 mg pill costs between 200 and 242 USD.[1]
Medical uses
Erlotinib has shown a survival benefit in the treatment of lung cancer in phase III trials. The SATURN (Sequential Tarceva in Unresectable NSCLC) study found that erlotinib added to chemotherapy improved overall survival by 19%, and improved progression-free survival (PFS) by 29%, when compared to chemotherapy alone.[2][3]
The U.S. Food and Drug Administration (FDA) has approved erlotinib for the treatment of locally advanced or metastatic non-small cell lung cancer that has failed at least one prior chemotherapy regimen.
In November 2005, the FDA approved erlotinib in combination with gemcitabine for treatment of locally advanced, unresectable, or metastatic pancreatic cancer.[4]
In lung cancer, erlotinib has been shown to be effective in patients with or without EGFR mutations, but appears to be more effective in patients with EGFR mutations.[5][6] Overall survival, progression-free survival and one-year survival are similar to standard second-line therapy (docetaxel or pemetrexed). Overall response rate is about 50% better than standard second-line chemotherapy.[6] Patients who are non-smokers, and light former smokers, with adenocarcinoma or subtypes like BAC are more likely to have EGFR mutations, but mutations can occur in all types of patients. A test for the EGFR mutation in cancer patients has been developed by Genzyme.
Erlotinib has recently been shown to be a potent inhibitor of JAK2V617F activity. JAK2V617F is a mutant of tyrosine kinase JAK2, is found in most patients with polycythemia vera (PV) and a substantial proportion of patients with idiopathic myelofibrosis or essential thrombocythemia. The study suggests that erlotinib may be used for treatment of JAK2V617F-positive PV and other myeloproliferative disorders.[7]
The drug's US patent will expire in 2020.[8] In May 2012, the US District Court of Delaware passed an order in favour of OSI Pharmaceutical LLC against Mylan Pharmaceuticals upholding the validity of the patent for Erlotinib. In India, generic pharmaceutical firm Cipla is battling with Roche against the Indian patent for this drug.
Side effects
Common
- Rash occurs in the majority of patients. This resembles acne and primarily involves the face and neck. It is self-limited and resolves in the majority of cases, even with continued use. Interestingly, some clinical studies have indicated a correlation between the severity of the skin reactions and increased survival though this has not been quantitatively assessed.[9] The Journal of Clinical Oncology reported in 2004 that "cutaneous [skin] rash seems to be a surrogate marker of clinical benefit, but this finding should be confirmed in ongoing and future studies."[10] The newsletter Lung Cancer Frontiers reported in its October 2003 issue, "Patients with moderate to severe cutaneous reactions [rashes] have a far better survival, than those with only mild reactions and much better than those with no cutaneous manifestations of drug effects."[11]
- Diarrhea
- Loss of appetite
- Fatigue
- Rarely, interstitial pneumonitis, which is characterized by cough and increased dyspnea. This may be severe and must be considered among those patients whose breathing acutely worsens.
- Rarely, ingrown hairs, such as eyelashes
- It has also been suggested that erlotinib can cause hearing loss.
- Partial hair loss (by strands, not typically in clumps)
Rare
- gastrointestinal tract toxicity
- serious or fatal gastrointestinal tract perforations
- skin toxicity
- bullous, blistering, and exfoliative skin conditions (some fatal)
- Stevens–Johnson syndrome/toxic epidermal necrolysis [12]
- ocular disorders
- corneal lesions
- Pulmonary toxicity
Interactions
As per published report, erlotinib is not a substrate for either of hepatic OATPs (OATP1B1 or OATP1B3).[14] Also, erlotinib is not an inhibitor of OATP-1B1 or OATP-1B3 transporter.[15]
Erlotinib is mainly metabolized by the liver enzyme CYP3A4. Compounds which induce this enzyme (i.e. stimulate its production), such as St John's wort, can lower erlotinib concentrations, while inhibitors can increase concentrations.[16]
Resistance to treatment

As with other ATP competitive small molecule tyrosine kinase inhibitors, such as imatinib (Gleevec) in CML, patients rapidly develop resistance. In the case of erlotinib this typically occurs 8–12 months from the start of treatment. Over 50% of resistance is caused by a mutation in the ATP binding pocket of the EGFR kinase domain involving substitution of a small polar threonine residue with a large nonpolar methionine residue (T790M).[17] While proponents of the 'gatekeeper' mutation hypothesis suggest this mutation prevents the binding of erlotinib through steric hindrance, research suggests that T790M confers an increase in ATP binding affinity, thereby reducing the inhibitory efficacy of erlotinib.[18]
Approximately 20% of drug resistance is caused by amplification of the hepatocyte growth factor receptor, which drives ERBB3 dependent activation of PI3K.[19][20]
Other cases of resistance can involve numerous mutations, including recruitment of a mutated IGF-1 receptor to dimerise with EGFR so forming a heterodimer.[21] This allows activation of the downstream effectors of EGFR even in the presence of an EGFR inhibitor. Some IGR-1R inhibitors are in various stages of development (based either around TKIs such as AG1024 or AG538[22] or pyrrolo[2,3-d]-pyrimidine derivatives such as NVP-AEW541[23]). The monoclonal antibody figitumumab which targets the IGF-1R is currently undergoing clinical trials.[24][25]
Another cause of resistance can be inactivating mutations of the PTEN tumour suppressor, which allow increased activation of Akt independent of stimulation by EGFR.[26]
The most promising approach to combating resistance is likely to be combination therapy. Commencing treatment with a number of different therapeutic agents with differing modes of action is thought to provide the best defence against development of T790M and other resistance conferring mutations.[27]
Mechanism
Erlotinib is an epidermal growth factor receptor inhibitor (EGFR inhibitor). The drug follows Iressa (gefitinib), which was the first drug of this type. Erlotinib specifically targets the epidermal growth factor receptor (EGFR) tyrosine kinase, which is highly expressed and occasionally mutated in various forms of cancer. It binds in a reversible fashion to the adenosine triphosphate (ATP) binding site of the receptor.[28] For the signal to be transmitted, two EGFR molecules need to come together to form a homodimer. These then use the molecule of ATP to trans-phosphorylate each other on tyrosine residues, which generates phosphotyrosine residues, recruiting the phosphotyrosine-binding proteins to EGFR to assemble protein complexes that transduce signal cascades to the nucleus or activate other cellular biochemical processes. When erlotinib binds to EGFR, formation of phosphotyrosine residues in EGFR is not possible and the signal cascades are not initiated.
References
- ↑ Langreth, Robert (June 29, 2016). "Decoding Big Pharma's Secret Drug Pricing Practices". Bloomberg. Retrieved 15 July 2016.
- ↑ 2009 - SATURN: A double-blind, randomized, phase III study of maintenance erlotinib versus placebo following nonprogression with first-line platinum-based chemotherapy in patients with advanced NSCLC.
- ↑ April 2010 - Tarceva Indication Announcement Letter
- ↑ Takimoto CH, Calvo E. "Principles of Oncologic Pharmacotherapy" in Pazdur R, Wagman LD, Camphausen KA, Hoskins WJ (Eds) Cancer Management: A Multidisciplinary Approach. 11 ed. 2008.
- ↑ Kobayashi, K.; Hagiwara, K. (2013). "Epidermal growth factor receptor (EGFR) mutation and personalized therapy in advanced nonsmall cell lung cancer (NSCLC)". Targeted Oncology. 8 (1): 27–33. doi:10.1007/s11523-013-0258-9. PMC 3591525
 . PMID 23361373.
. PMID 23361373. - 1 2 Qi, W. X.; Shen, Z.; Lin, F.; Sun, Y. J.; Min, D. L.; Tang, L. N.; He, A. N.; Yao, Y. (2012). "Comparison of the efficacy and safety of EFGR tyrosine kinase inhibitor monotherapy with standard second-line chemotherapy in previously treated advanced non-small-cell lung cancer: A systematic review and meta-analysis". Asian Pacific Journal of Cancer Prevention. 13 (10): 5177–5182. doi:10.7314/APJCP.2012.13.10.5177. PMID 23244131.
- ↑ Li Z, Xu M, Xing S, Ho W, Ishii T, Li Q, Fu X, Zhao Z (2007). "Erlotinib Effectively Inhibits JAK2V617F Activity and Polycythemia Vera Cell Growth". J Biol Chem. 282 (6): 3428–32. doi:10.1074/jbc.C600277200. PMC 2096634
 . PMID 17178722.
. PMID 17178722. - ↑ http://drugpatentwatch.com/p/ingredient/erlotinib, "Details for Generic Name: erlotinib", DrugPatentWatch.com
- ↑ Dudek A, Kmak K, Koopmeiners J, Keshtgarpour M (2006). "Skin rash and bronchoalveolar histology correlates with clinical benefit in patients treated with gefitinib as a therapy for previously treated advanced or metastatic non-small cell lung cancer". Lung Cancer. 51 (1): 89–96. doi:10.1016/j.lungcan.2005.09.002. PMID 16290256.
- ↑ Román Pérez-Soler, M.D.; et al. (2004). "Selected Highlights". Lung Cancer Frontiers. 22 (16): 3238–3247.
- ↑ Thomas L. Petty, M.D. (2003). "Determinants of Tumor Response and Survival With Erlotinib in Patients With Non—Small-Cell Lung Cancer". Journal of Clinical Oncology. 1 (17): 3–4.
- ↑ http://jama.ama-assn.org/cgi/content/extract/301/24/2542-b
- ↑ Ren, S; Li, Y; Li, W; Zhao, Z; Jin, C; Zhang, D (2012). "Fatal asymmetric interstitial lung disease after erlotinib for lung cancer". Respiration. 84 (5): 431–5. doi:10.1159/000339508. PMID 22889962.
- ↑ Khurana V, Minocha M, Pal D, Mitra AK (March 2014). "Role of OATP-1B1 and/or OATP-1B3 in hepatic disposition of tyrosine kinase inhibitors.". Drug Metabol Drug Interact. 0 (0): 1–11. doi:10.1515/dmdi-2013-0062. PMID 24643910.
- ↑ Khurana V, Minocha M, Pal D, Mitra AK (May 2014). "Inhibition of OATP-1B1 and OATP-1B3 by tyrosine kinase inhibitors.". Drug Metabol Drug Interact. 0 (0): 1–11. doi:10.1515/dmdi-2014-0014. PMID 24807167.
- ↑ Haberfeld, H, ed. (2010). Austria-Codex (in German) (2010/2011 ed.). Vienna: Österreichischer Apothekerverlag.
- ↑ Balak MN, Gong Y, Riely GJ, Somwar R, Li AR, Zakowski MF, Chiang A, Yang G, Ouerfelli O, Kris MG, Ladanyi M, Miller VA, Pao W (2006). "Novel D761Y and common secondary T790M mutations in epidermal growth factor receptor-mutant lung adenocarcinomas with acquired resistance to kinase inhibitors". Clin Cancer Res. 12 (1): 6494–501. doi:10.1158/1078-0432.CCR-06-1570. PMID 17085664.
- ↑ Yun CH, Mengwasser KE, Toms AV, Woo MS, Greulich H, Wong KK, Meyerson M, Eck MJ (2008). "The T790M mutation in EGFR kinase causes drug resistance by increasing the affinity for ATP". PNAS. 105 (6): 2070–5. doi:10.1073/pnas.0709662105. PMC 2538882
 . PMID 18227510.
. PMID 18227510. - ↑ Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, Lindeman N, Gale CM, Zhao X, Christensen J, Kosaka T, Holmes AJ, Rogers AM, Cappuzzo F, Mok T, Lee C, Johnson BE, Cantley LC, Jänne PA (2007). "MET Amplification Leads to Gefitinib Resistance in Lung Cancer by Activating ERBB3 Signaling". Science. 316 (5827): 1039–43. doi:10.1126/science.1141478. PMID 17463250.
- ↑ EBean J, Brennan C, Shih JY, Riely G, Viale A, Wang L, Chitale D, Motoi N, Szoke J, Broderick S, Balak M, Chang WC, Yu CJ, Gazdar A, Pass H, Rusch V, Gerald W, Huang SF, Yang PC, Miller V, Ladanyi M, Yang CH, Pao W (2007). "MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib". PNAS. 104 (52): 20932–7. doi:10.1073/pnas.0710370104. PMC 2409244
 . PMID 18093943.
. PMID 18093943. - ↑ Jones H, Goddard L, Gee J, Hiscox S, Rubini M, Barrow D, Knowlden J, Williams S, Wakeling A, Nicholson R (2004). "Insulin-like growth factor-I receptor signalling and acquired resistance to gefitinib (ZD1839; Iressa) in human breast and prostate cancer cells". Endocr Relat Cancer. 11 (4): 793–814. doi:10.1677/erc.1.00799. PMID 15613453. Free full text
- ↑ Blum G, Gazit A, Levitzki A (2000). "Substrate competitive inhibitors of IGF-1 receptor kinase". Biochemistry. 39 (51): 15705–12. doi:10.1021/bi001516y. PMID 11123895.
- ↑ Warshamana-Greene G, Litz J, Buchdunger E, García-Echeverría C, Hofmann F, Krystal G (2005). "The insulin-like growth factor-I receptor kinase inhibitor, NVP-ADW742, sensitizes small cell lung cancer cell lines to the effects of chemotherapy". Clin Cancer Res. 11 (4): 1563–71. doi:10.1158/1078-0432.CCR-04-1544. PMID 15746061. Free full text
- ↑ Clinical trial number NCT00976508 for "Figitumumab Combined With Pegvisomant For Advanced Solid Tumors" at ClinicalTrials.gov
- ↑ Clinical trial number NCT00635245 for "CP-751871 in Treating Women With Early-Stage Breast Cancer That Can Be Removed by Surgery" at ClinicalTrials.gov
- ↑ Sos, M. L.; Koker, M.; Weir, B. A.; Heynck, S.; Rabinovsky, R.; Zander, T.; Seeger, J. M.; Weiss, J.; Fischer, F.; Frommolt, P.; Michel, K.; Peifer, M.; Mermel, C.; Girard, L.; Peyton, M.; Gazdar, A. F.; Minna, J. D.; Garraway, L. A.; Kashkar, H.; Pao, W.; Meyerson, M.; Thomas, R. K. (2009). "PTEN Loss Contributes to Erlotinib Resistance in EGFR-Mutant Lung Cancer by Activation of Akt and EGFR". Cancer Research. 69 (8): 3256–3261. doi:10.1158/0008-5472.CAN-08-4055. PMC 2849653
 . PMID 19351834.
. PMID 19351834. - ↑ J Clin Invest. 2009 October 1; 119(10). Tang, Dual MET EGFR combinatorial inhibition against T790M-EGFR-mediated erlotinib-resistant lung cancer, Br J Cancer. 2008 September 16; 99(6).
- ↑ Raymond E, Faivre S, Armand J (2000). "Epidermal growth factor receptor tyrosine kinase as a target for anticancer therapy". Drugs. 60 Suppl 1: 15–23; discussion 41–2. doi:10.2165/00003495-200060001-00002. PMID 11129168.
External links
- Official Tarceva website
- Tarceva Discussion Group for Cancer Patients
- Sordella R, Bell DW, Haber DA, Settleman J (August 2004). "Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways". Science. 305 (5687): 1163–7. doi:10.1126/science.1101637. PMID 15284455..
- Genzyme "Genzyme Launches Exclusive Lung Cancer Test" Press Release September 27, 2005
- "Determinants of Tumor Response and Survival With Erlotinib in Patients With Non-Small-Cell Lung Cancer, Journal of Clinical Oncology, August 15, 2004.
- October 2003 issue of Lung Cancer Frontiers on rash/effectiveness correlation
- FAQ: I started an EGFR inhibitor two weeks ago but haven’t developed a rash. Does this mean it’s not working?, Dr. Howard L. (Jack) West, M.D., GRACE, February 21, 2011 (directed toward the layperson).
- http://www.cancer.gov/clinicaltrials/results/lung-and-erlotinib0604l
- http://www.roche.com/med-cor-2007-10-22
- http://www.roche.com/med-cor-2009-05-30b
- http://www.cipla.com/whatsnew/news.htm#27apr09
- http://www.cipla.com/whatsnew/news.htm#20mar08