Osgood–Schlatter disease
| Osgood–Schlatter disease | |
|---|---|
|
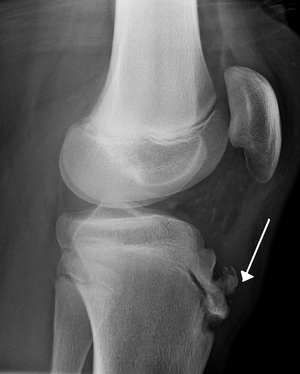
Lateral view X-ray of the knee demonstrating fragmentation of the tibial tubercle with overlying soft tissue swelling. | |
| Classification and external resources | |
| Specialty | Orthopedics |
| ICD-10 | M92.5 |
| ICD-9-CM | 732.4 |
| DiseasesDB | 9299 |
| MedlinePlus | 001258 |
| eMedicine | emerg/347 orthoped/426 radio/491 sports/89 |
| Patient UK | Osgood–Schlatter disease |
Osgood–Schlatter disease (OSD), also known as apophysitis of the tibial tubercle, or Lannelongue's disease,[1] is an inflammation of the patellar ligament at the tibial tuberosity.[2] It is characterized by a painful bump just below the knee and is most often seen in young adolescents. Risk factors include overuse (especially in sports involving running, jumping and quick changes of direction) and adolescent growth spurts.
The condition is named after Robert Bayley Osgood (1873–1956), an American orthopedic surgeon and Carl B. Schlatter, (1864–1934), a Swiss surgeon who described the condition independently in 1903.[1]
Signs and symptoms

Osgood–Schlatter disease causes pain in the front lower part of the knee.[3] This is usually at the ligament-bone junction of the patellar ligament and the tibial tuberosity.[4] The tibial tuberosity is a slight elevation of bone on the anterior and proximal portion of the tibia. The patellar tendon attaches the anterior quadriceps muscles to the tibia.[5]
Intense knee pain is usually the presenting symptom that occurs during activities such as running, jumping, squatting, and especially ascending or descending stairs and during kneeling. The pain is worse with acute knee impact. The pain can be reproduced by extending the knee against resistance, stressing the quadriceps, or striking the knee. Pain is initially mild and intermittent. In the acute phase, the pain is severe and continuous in nature. Impact of the affected area can be very painful. Bilateral symptoms are observed in 20–30% of patients.
Diagnosis
Diagnosis is made based on signs and symptoms.[6]
Ultrasonography
This test can see various warning signs that predict if OSD might occur. Ultrasonography can detect if there is any swelling within the tissue as well as cartilage swelling.[5] Ultrasonography's main goal is to identify OSD in the early stage rather than later on. It has unique features such as detection of an increase of swelling within the tibia or the cartilage surrounding the area and can also see if there is any new bone starting to build up around the tibial tuberosity.
Types
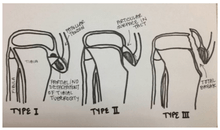
OSD may result in an avulsion fracture, with the tibial tuberosity separating from the tibia (usually remaining connected to a tendon or ligament). This injury is uncommon because there are mechanisms that prevent strong muscles from doing damage. The fracture on the tibial tuberosity can be a complete or incomplete break.
Type I: A small fragment is displaced proximally and does not require surgery.
Type II: The articular surface remains together and the fracture occurs at the junction where the secondary center of ossification and the proximal tibial epiphysis come together (may or may not require surgery).
Type III: Total break (through articular surface) including high chance of meniscal damage that usually requires surgery.
Differential diagnosis
Sinding-Larsen and Johansson syndrome,[7] is an analogous condition involving the patellar tendon and the lower margin of the patella bone, instead of the upper margin of the tibia. Sever's disease is a similar condition affecting the heel.
Prevention

One of the main ways to prevent OSD is to check the participant's flexibility in their quadriceps and hamstrings. Lack of flexibility in these muscles can be direct risk indicator for OSD. Muscles can shorten, which can cause pain but this is not permanent.[8] Stretches can help reduce shortening of the muscles. The main stretches for prevention of OSD focus on the hamstrings and quadriceps.[9]
Treatment
Treatment is generally conservative with rest, ice, and specific exercises being recommended.[10] Simple pain killers may be used if required such as acetaminophen (paracetamol) or ibuprofen. Typically symptoms resolve as the growth plate closes.[10] Physiotherapy is generally recommended once the initial symptoms have improved to prevent recurrence.[10] Surgery may rarely be used in those who have stopped growing yet still have symptoms.[10]
Physiotherapy
Recommended efforts include exercises to improve the strength of the quadriceps, hamstring and gastrocnemius muscles.[10]
Bracing or use of an orthopedic cast to enforce joint immobilization is rarely required and does not necessarily give quicker resolution. Sometimes, however, bracing may give comfort and help reduce pain as it reduces strain on the tibial tubercle.[11]
Surgery
Surgical excision may rarely be required in skeletally mature patients.[12] In chronic cases that are refractory to conservative treatment, surgical intervention yields good results, particularly for patients with bony or cartilaginous ossicles. Excision of these ossicles produces resolution of symptoms and return to activity in several weeks. After surgery, it is common for lack of blood flow to below the knees and to the feet. This may cause the loss of circulation to the area, but will be back to normal again shortly. A high pain may come and go every once in a while, due to the lack of blood flow. If this happens, sitting down will help the pain decrease. Removal of all loose intratendinous ossicles associated with prominent tibial tubercles is the procedure of choice, both from the functional and the cosmetic point of view.[13]
Rehabilitation

Rehabilitation focuses on muscle strengthening, gait training, and pain control to restore knee function.[14] Nonsurgical treatments for less severe symptoms include: exercises for strength, stretches to increase range of motion, ice packs, knee tape, knee braces, anti-inflammatory agents, and electrical stimulation to control inflammation and pain. Quadriceps and hamstring exercises prescribed by rehabilitation experts restore flexibility and muscle strength.
Education and knowledge on stretches and exercises is important. Exercises should lack pain and increase gradually with intensity. The patient is given strict guidelines on how to perform exercises at home to avoid more injury.[14] Exercises can include leg raises, squats, and wall stretches to increase quadriceps and hamstring strength. This helps to avoid pain, stress, and tight muscles that lead to further injury that oppose healing. Knee orthotics such as patella straps and knee sleeves help decrease force traction and prevent painful tibia contact by restricting unnecessary movement, providing support, and also adding compression to the area of pain.
Prognosis

The condition is usually self-limiting and is caused by stress on the patellar tendon that attaches the quadriceps muscle at the front of the thigh to the tibial tuberosity. Following an adolescent growth spurt, repeated stress from contraction of the quadriceps is transmitted through the patellar tendon to the immature tibial tuberosity. This can cause multiple subacute avulsion fractures along with inflammation of the tendon, leading to excess bone growth in the tuberosity and producing a visible lump which can be very painful, especially when hit. Activities such as kneeling may also irritate the tendon.
The syndrome may develop without trauma or other apparent cause; however, some studies report up to 50% of patients relate a history of precipitating trauma. Several authors have tried to identify the actual underlying etiology and risk factors that predispose Osgood–Schlatter disease and postulated various theories. However, currently it is widely accepted that Osgood–Schlatter disease is a traction apophysitis of the proximal tibial tubercle at the insertion of the patellar tendon caused by repetitive micro-trauma. In other words, Osgood–Schlatter disease is an overuse injury and closely related to the physical activity of the child. It was shown that children who actively participate in sports are affected more frequently as compared with non-participants. In a retrospective study of adolescents, old athletes actively participating in sports showed a frequency of 21% reporting the syndrome compared with only 4.5% of age-matched nonathletic controls.[15]
The symptoms usually resolve with treatment but may recur for 12–24 months before complete resolution at skeletal maturity, when the tibial epiphysis fuses. In some cases the symptoms do not resolve until the patient is fully grown. In approximately 10% of patients the symptoms continue unabated into adulthood, despite all conservative measures.[12]
Long-term implications
OSD occurs from the combined effects of tibial tuberosity immaturity and quadriceps tightness.[5] There is a possibility of migration of the ossicle or fragmentation in Osgood-Schlatter patients.[4] The implications of OSD and the ossification of the tubercle can lead to functional limitations and pain for patients into adulthood.[9]
Of people admitted with OSD, about half were children who were between the ages of 1 and 17. In addition, in 2014, a case study of 261 patients was observed over 12 to 24 months. 237 of these patients responded well to sport restriction and non-steroid anti-inflammatory agents, which resulted in recovery to normal athletic activity.[16]
Epidemiology
Osgood–Schlatter disease generally occurs in boys and girls aged 9–16[17] coinciding with periods of growth spurts. It occurs more frequently in boys than in girls, with reports of a male-to-female ratio ranging from 3:1 to as high as 7:1. It has been suggested that difference is related to a greater participation by boys in sports and risk activities than by girls.[18]
Society and culture
Paul Scholes is a sportsman who has recovered from this condition[19] whilst Mick Bennett took up cycling as a means of treatment.[20] The French tennis player, Gaël Monfils wears patella bands in an attempt to combat the condition.[21] Liverpool F.C. captain Jordan Henderson is also said to require regular treatment for his condition.[22]
References
- 1 2 Osgood-Schlatter disease at Who Named It?
- ↑ Nowinski RJ, Mehlman CT (1998). "Hyphenated history: Osgood-Schlatter disease". Am J. Orthopaedic. 27 (8): 584–5. PMID 9732084.
- ↑ Atanda A, Jr; Shah, SA; O'Brien, K (1 February 2011). "Osteochondrosis: common causes of pain in growing bones.". American family physician. 83 (3): 285–91. PMID 21302869.
- 1 2 Çakmak, S., Tekin, L., & Akarsu, S. (2014). Long-term outcome of Osgood-Schlatter disease: not always favorable. Rheumatology International, 34(1), 135–136.
- 1 2 3 Nakase, J., Aiba, T., Goshima, K., Takahashi, R., Toratani, T., Kosaka, M., Ohashi, Y. & Tsuchiya, H. (2014). "Relationship between the skeletal maturation of the distal attachment of the patellar tendon and physical features in preadolescent male football players". Knee Surgery, Sports Traumatology, Arthroscopy. 22 (1): 195–199. doi:10.1007/s00167-012-2353-3. PMID 23263228.
- ↑ Cassas KJ, Cassettari-Wayhs A (2006). "Childhood and adolescent sports-related overuse injuries". Am Fam Physician. 73 (6): 1014–22. PMID 16570735.
- ↑ Sinding-Larsen and Johansson syndrome at Who Named It?
- ↑ Lucena, G. L., Gomes, C. A., & Guerro R. O. (2010). Prevalence and Associated Factors of Osgood-Schlatter Syndrome in a Population-Based Sample of Brazilian Adolescents. The American Journal of Sports Medicine, 39, 415–420. doi:10.1177/0363546510383835
- 1 2 Kabiri, L., Tapley, H., & Tapley, S. (2014). "Evaluation and conservative treatment for Osgood–Schlatter disease: A critical review of the literature". International Journal of therapy & Rehabilitation. 21 (2): 91–96. doi:10.12968/ijtr.2014.21.2.91.
- 1 2 3 4 5 Gholve, PA; Scher, DM; Khakharia, S; Widmann, RF; Green, DW (February 2007). "Osgood Schlatter syndrome.". Current Opinion in Pediatrics. 19 (1): 44–50. doi:10.1097/mop.0b013e328013dbea. PMID 17224661.
- ↑ Engel A, Windhager R (1987). "[Importance of the ossicle and therapy of Osgood-Schlatter disease]". Sportverletz Sportschaden (in German). 1 (2): 100–8. doi:10.1055/s-2007-993701. PMID 3508010.
- 1 2 Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW (2007). "Osgood Schlatter syndrome". Curr. Opin. Pediatr. 19 (1): 44–50. doi:10.1097/MOP.0b013e328013dbea. PMID 17224661.
- ↑ O. Josh Bloom; Leslie Mackler (February 2004). "What is the best treatment for Osgood-Schlatter disease?" (pdf). Journal of Family Practice. 53 (2).
- 1 2 Baltaci, H., Ozer, V., and Tunay, B. (2004). Rehabilitation of avulsion fracture of the tibial tuberosity. Knee Surgery, Sports Traumatology, Arthroscopy. 12, 115–118.
- ↑ Kujala UM, Kvist M, Heinonen O (1985). "Osgood-Schlatter's disease in adolescent athletes. Retrospective study of incidence and duration". Am J Sports Med. 13 (4): 236–41. doi:10.1177/036354658501300404. PMID 4025675.
- ↑ Bloom J (2004). "What is the best treatment for Osgood-Schlatter disease?". Journal of Family Practice. 53 (2): 153–156.
- ↑ Yashar A, Loder RT, Hensinger RN (1995). "Determination of skeletal age in children with Osgood-Schlatter disease by using radiographs of the knee". J Pediatr Orthop. 15 (3): 298–301. doi:10.1097/01241398-199505000-00006. PMID 7790482.
- ↑ Vreju F, Ciurea P, Rosu A (December 2010). "Osgood-Schlatter disease—ultrasonographic diagnostic". Med Ultrason. 12 (4): 336–9. PMID 21210020.
- ↑ Simply the best. The Guardian (London). 18 May 2008
- ↑ "Famous Last Words: Mick Bennett". Cycling Weekly. 7 March 2014. Retrieved 30 May 2014.
- ↑ Gael could miss French Open. Sky Sports. 21 April 2009
- ↑ Jordan Henderson: From Sunderland's bright light to Liverpool's brilliant leader. Goal.com. 26 November 2016
| Wikimedia Commons has media related to Osgood–Schlatter disease. |