Posterior column–medial lemniscus pathway
| Posterior column-medial lemniscus pathway | |
|---|---|
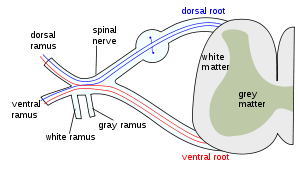 The formation of the spinal nerve from the dorsal and ventral roots. | |
 Originating in peripheral sensory receptors, the posterior column-medial lemniscus pathway transmits fine touch and conscious proprioceptive information to the brain. | |
| Details | |
| Precursor | Neural tube and crest |
| System | Somatosensory system |
| Latin | via columnae posterioris lemniscique medialis |
Posterior column–medial lemniscus pathway (PCML) (also known as the dorsal column-medial lemniscus pathway DCML) is a sensory pathway of the central nervous system that conveys localized sensations of fine touch, vibration, two-point discrimination, and proprioception (position sense) from the skin and joints. It transmits information from the body to the postcentral gyrus of the cerebral cortex.[1][2]
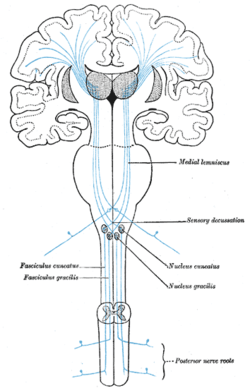
There are three neurons involved in the pathway: first-order neurons, second-order neurons, and third-order neurons. The first-order neurons reside in dorsal root ganglia and send their axons through the gracile fasciculus and cuneate fasciculus.[3] The first-order axons make contact with second order neurons at the gracile and cuneate nuclei in the lower medulla. The second-order neurons send their axons to the thalamus. The third order neurons arise from thalamus to the postcentral gyrus.
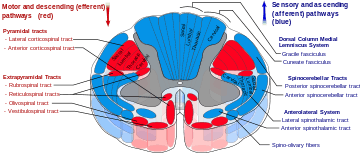
The posterior column is composed of gracile fasciculus and cuneate fasciculus. The gracile fasciculus carries input from the lower half of the body and the cuneate fasciculus carries input from the upper half of the body. The gracile fasciculus arise from the fibers more medial than the cuneate fasciculus.
When the axons of second-order neurons of the dorsal column system decussate in the medulla, they are called internal arcuate fibers. The crossings of the internal arcuate fibers form the medial lemniscus.
The name comes from the two structures that the sensation travels up: the posterior (or dorsal) column of the spinal cord, and the medial lemniscus in the brainstem.
The PCML pathway is composed of rapidly conducting, large, myelinated fibers.[2]
Structure
Discriminative sensation is well developed in the fingers of humans, and allows us to feel fine textures and determine what an unknown object in our hands is without looking at it (stereognosis).
First neuron
This fine sensation is detected by mechanoreceptors called tactile corpuscles that lie in the dermis of the skin close to the epidermis. When these structures are stimulated by slight pressure, an action potential is started. Alternatively, proprioceptive muscle spindles and other skin surface touch receptors such as Merkel cells, bulbous corpuscles, lamellar corpuscles, and hair follicle receptors (peritrichial endings) may involve the first neuron in this pathway.
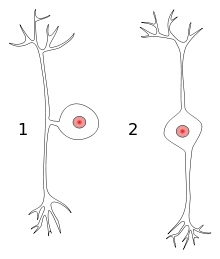
The sensory neurons in this pathway are pseudounipolar, meaning that they have a single process emanating from the soma (also known as the cell body, perikaryon, or cyton) with two distinct branches: one peripheral branch that functions somewhat like a dendrite of a typical neuron by receiving input (although it should not be confused with a true dendrite), and one central branch that functions like a typical axon by carrying information to other neurons (again, both branches are actually part of one axon).
The action potential that was initiated in the tactile corpuscles will travel up the peripheral branch of the pseudounipolar neuron's axon and reach the neuron's soma in the dorsal root ganglion.[Note 1] Then it will continue along the central branch of that same neuron's axon through the posterior root, into the posterior horn, and up the posterior column of the spinal cord.
PCML pathway axons from the lower body enter the posterior column inferior to T6 and travel in a medial section of the column called the fasciculus gracilis (also known as the tract of Goll, gracile fasciculus, or gracile tract).[4] Axons from the upper body enter at or superior to T6 and travel up a more lateral section called the fasciculus cuneatus (also known as the tract of Burdach, cuneate fasciculus, or cuneate tract). In effect, the shorter upper body axons enter "after" and travel outside the longer lower body axons.
At the level of the closed medulla oblongata, lower body axons synapse with neurons in the gracile nucleus (nucleus gracilis), and upper body axons synapse with neurons in the cuneate nucleus (nucleus cuneatus).
Second neuron
The secondary neurons (that start in the nuclei) cross over to the other side of the medulla (as internal arcuate fibres) to form the medial lemniscus. This crossing over is commonly referred to as the sensory decussation.
At the medulla, the medial lemniscus is orientated perpendicular to the way the fibres travelled in the posterior columns. For example, in the columns, lower limb is medial, upper limb is more lateral. At the medial lemniscus, axons from the leg are more ventral, and axons from the arm are more dorsal. Fibres from the trigeminal nerve (supplying the head) come in dorsal to the arm fibres, and travel up the lemniscus too.
The medial lemniscus rotates 90 degrees at the pons. The secondary axons from neurons giving sensation to the head, stay at around the same place, while the leg axons move outwards.
The axons travel up the rest of the brainstem, and synapse at the thalamus (at the ventral posterolateral nucleus for sensation from the neck, trunk, and extremities, and at the ventral posteromedial nucleus for sensation from the head).
Third neuron
Neurons starting in the thalamus travel up the posterior limb of the internal capsule, and again head and leg swap relative positions. The axons synapse in the primary sensory cortex, with lower body sensation most medial (e.g., the paracentral lobule) and upper body more lateral. Consider: Corona Radiata --> 312 Brodeman
Clinical significance
Examination
The pathway is tested with the Romberg's test. Lesions to the posterior column-medial lemniscus pathway below the decussation of its fibers produce loss of sensation on the same side of the body as the lesion. Above the decussation produces loss of sensation on the opposite side of the body than the lesion.
Notes
- ↑ Not generally called "posterior root ganglion".
References
- ↑ Physiology: 8/8ch5/s8ch5_22 - Essentials of Human Physiology
- 1 2 O'Sullivan, S. B., & Schmitz, T. J. (2007). Physical Rehabilitation (5th Edition ed.). Philadelphia: F.A. Davis Company.
- ↑ Giuffrida, R; Rustioni, A (1992). "Dorsal root ganglion neurons projecting to the dorsal column nuclei of rats". J. Comp. Neurol. 316: 206–20. doi:10.1002/cne.903160206. PMID 1374085.
- ↑ Luria, V; Laufer, E (Jul 2, 2007). "Lateral motor column axons execute a ternary trajectory choice between limb and body tissues.". Neural development. 2: 13. doi:10.1186/1749-8104-2-13. PMID 17605791.