Steatosis
| Steatosis | |
|---|---|
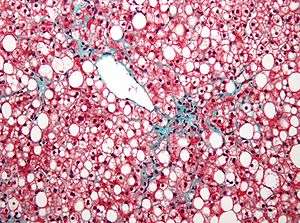 | |
| Micrograph demonstrating marked (macrovesicular) steatosis in non-alcoholic fatty liver disease. Masson's trichrome stain. | |
| Classification and external resources | |
| ICD-10 | Xxx.x |
| ICD-9-CM | xxx |
Steatosis (also called fatty change, fatty degeneration, or adipose degeneration) is the process describing the abnormal retention of lipids within a cell. It reflects an impairment of the normal processes of synthesis and elimination of triglyceride fat. Excess lipid accumulates in vesicles that displace the cytoplasm. When the vesicles are large enough to distort the nucleus, the condition is known as macrovesicular steatosis; otherwise, the condition is known as microvesicular steatosis. While not particularly detrimental to the cell in mild cases, large accumulations can disrupt cell constituents, and in severe cases the cell may even burst.
The risk factors associated with steatosis are varied, and include diabetes mellitus,[1][2] protein malnutrition,[3] hypertension[4] cell toxins, obesity,[5] anoxia[6] and sleep apnea.[7][8][9] As the liver is the primary organ of lipid metabolism it is most often associated with steatosis; however, it may occur in any organ, commonly the kidneys, heart, and muscle.[6]
Pathogenesis
No single mechanism leading to steatosis exists; rather, a varied multitude of pathologies disrupt normal lipid movement through the cell and cause accumulation.[10] These mechanisms can be separated on whether they ultimately cause an oversupply of lipid which can not be removed quickly enough (i.e., too much in), or whether they cause a failure in lipid breakdown (i.e., not enough used).
Failure of lipid metabolism can also lead to the mechanisms which would normally utilise or remove lipids becoming impaired, resulting in the accumulation of unused lipids in the cell. Certain toxins, such as alcohols, carbon tetrachloride, aspirin, and diphtheria toxin, interfere with cellular machinery involved in lipid metabolism. In those with Gaucher's disease, the lysosomes fail to degrade lipids and steatosis arises from the accumulation of glycolipids. Protein malnutrition, such as that seen in kwashiorkor, results in a lack of precursor apoproteins within the cell, therefore unused lipids which would normally participate in lipoprotein synthesis begin to accumulate.
Macrovesicular steatosis
Macrovesicular steatosis is the more common form of fatty degeneration and may be caused by oversupply of lipids due to obesity, obstructive sleep apnea (OSA),[11] insulin resistance, or alcoholism. Nutrient malnutrition may also cause the mobilisation of fat from adipocytes and create a local oversupply in the liver where lipid metabolism occurs. Excess alcohol over a long period of time can induce steatosis. The breakdown of large amounts of ethanol in alcoholic drinks produces large amounts of chemical energy, in the form of NADH, signalling to the cell to inhibit the breakdown of fatty acids (which also produces energy) and simultaneously increase the synthesis of fatty acids. This "false sense of energy" results in more lipid being created than is needed.
Microvesicular steatosis
Microvesicular steatosis is characterized by small intracytoplasmic fat vacuoles (liposomes) which accumulate in the cell. Common causes are tetracyclines, acute fatty liver of pregnancy, Reye's syndrome, and hepatitis C.
Histology
Histologically, steatosis is physically apparent as lipid within membrane bound liposomes of parenchymal cells.[6] When this tissue is fixed and stained to be better viewed under a microscope, the lipid is usually dissolved by the solvents used to prepare the sample. As such, samples prepared this way will appear to have empty holes (or vacuoles) within the cells where the lipid has been cleared. Special lipid stains, such as Sudan stains and osmium tetroxide are able to retain and show up lipid droplets, hence more conclusively indicating the presence of lipids. Other intracellular accumulations, such as water or glycogen, can also appear as clear vacuoles, therefore it becomes necessary to use stains to better decide what is accumulating.
Grossly, steatosis causes organ enlargement and lightening in colour.[6] This is due to the high lipid content increasing the organ's volume and becoming visible to the unaided eye. In severe cases, the organ may become vastly enlarged, greasy, and yellow in appearance.
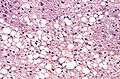 Histological section of a mouse's liver showing severe steatosis. The clear vacuoles contained lipid in life; however, histological fixation caused it to be dissolved and hence only empty/clear spaces are seen.
Histological section of a mouse's liver showing severe steatosis. The clear vacuoles contained lipid in life; however, histological fixation caused it to be dissolved and hence only empty/clear spaces are seen.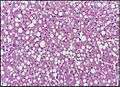 Micrograph of fatty liver showing lipid steatosis. H&E stain.
Micrograph of fatty liver showing lipid steatosis. H&E stain.
Radiography
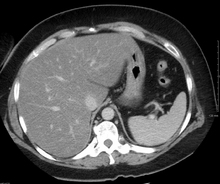
On X-ray computed tomography (CT), the increased fat component will decrease the density of the liver tissue, making the image less bright. Typically the density of the spleen and liver are roughly equivalent. In steatosis, there is a difference between the density and brightness of the two organs, with the liver appearing darker.[12] On ultrasound, fat is more echogenic (capable of reflecting sound waves). The combination of liver steatosis being dark on CT and bright on ultrasound is sometimes known as the flip flop sign.
See also
References
- ↑ Araya Q AV, et al. (2006). "Glucose tolerance alterations and frequency of metabolic syndrome among patients with non alcoholic fatty liver disease". Rev Med Chil. 134 (9): 1092–1098. PMID 17167710.
- ↑ Ali ES, Hua J, Wilson CH, Tallis GA, Zhou FH, Rychkov GY, Barritt GJ. "The glucagon-like peptide-1 analogue exendin-4 reverses impaired intracellular Ca2+ signalling in steatotic hepatocytes". BBA-Molecular Cell Research. doi:10.1016/j.bbamcr.2016.05.006.
- ↑ Conde Martel A, et al. (1993). "Liver changes in protein malnutrition. An experimental study in rats". Nutr Hosp. 8 (6): 358–363. PMID 8373879.
- ↑ MJ Brookes; BT Cooper (2007). "Hypertension and fatty liver: guilty by association?". J Hum Hypertens. 21 (4): 264–270. doi:10.1038/sj.jhh.1002148. PMID 17273155.
- ↑ S Saadeh (2007). "Nonalcoholic Fatty liver disease and obesity". Nutr Clin Pract. 22 (1): 1–10. doi:10.1177/011542650702200101. PMID 17242448.
- 1 2 3 4 Cotran; Kumar, Collins (1998). Robbins Pathologic Basis of Disease. Philadelphia: W.B Saunders Company. ISBN 0-7216-7335-X.
- ↑ MH Ahmed; CD Byrne (2010). "Obstructive sleep apnea syndrome and fatty liver: association or causal link?". World J Gastroenterol. 16 (34): 4243–52. doi:10.3748/wjg.v16.i34.4243. PMC 2937104
 . PMID 20818807.
. PMID 20818807. - ↑ H Singh; R Pollock; J Uhanova; M Kryger; K Hawkins; GY Minuk (2005). "Symptoms of Obstructive Sleep Apnea in Patients with Nonalcoholic Fatty Liver Disease". Digestive Diseases and Sciences. 50 (12): 2338–2343. doi:10.1007/s10620-005-3058-y.
- ↑ F Tanne; F Gagnadoux; O Chazouilleres; B Fleury; D Wendum; E Lasnier; B Labeau; R Poupon; L Serfaty (2005). "Chronic Liver Injury During Obstructive Sleep Apnea". Hepatology. 41 (6): 1290–1296. doi:10.1002/hep.20725.
- ↑ Wilson CH, Ali ES, Scrimgeour N, Martin AM, Hua J, Tallis GA, Rychkov GY, Barritt GJ (2015). "Steatosis inhibits liver cell store-operated Ca2+ entry and reduces ER Ca2+ through a protein kinase C-dependent mechanism". The Biochemical Journal. 466 (2): 379–90. doi:10.1042/BJ20140881. PMID 25422863.
- ↑ Bhattacharjee R, Gozal D (2010). "Metabolic disease in sleep disordered breathing: puberty! puberty!". Sleep. 33: 1133–4. PMC 2938852
 . PMID 20857857.
. PMID 20857857. - ↑ Helms, Clyde A.; Brant, William E. (2007). Fundamentals of diagnostic radiology. Phila: Lippincott, Williams & Wilkins. ISBN 0-7817-6135-2.