Contact lens

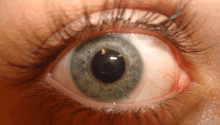
A contact lens, or simply contact or CL, is a thin lens placed directly on the surface of the eye. CLs are considered medical devices and can be worn to correct vision, or for cosmetic or therapeutic reasons.[1] In 2004, it was estimated that 125 million people (2%) use CLs worldwide, including 28 to 38 million in the United States.[2] In 2010, worldwide CL-market was estimated at $6.1 billion, while the U.S. soft lens market was estimated at $2.1 billion.[3] Multiple scientists estimated that the global market would reach $11.7 billion by 2015.[3] As of 2010, the average age of CL wearers globally was 31 years old, and two thirds of wearers were female.[4]
People choose to wear CLs for many reasons.[5] Aesthetics and cosmetics are the main motivating factors for people who want to avoid wearing glasses or to change the appearance of their eyes.[6] Others wear CLs for functional or optical reasons. When compared with spectacles, CLs typically provide better peripheral vision, and do not collect moisture (from rain, snow, condensation etc.) or perspiration; this makes them ideal for sports and other outdoor activities. CL wearers can also wear sunglasses, goggles, or other eyewear of their choice without having to fit them with prescription lenses or worry about compatibility with glasses. Additionally, there are conditions such as keratoconus and aniseikonia that are typically corrected better with CLs than with glasses.
Contact lenses market is likely to grow due to the increasing occurrence of eye related conditions such as astigmatism, hypermetropia and myopia. The other drivers of this market are increasing population, fashion statement and technological advancement. By the end of 2020, the market value is predicted to reach US$13.50 billion.[7]
History
Leonardo da Vinci is frequently credited with introducing the idea of CLs in his 1508 Codex of the eye, Manual D,[8] wherein he described a method of directly altering corneal power by either submerging the head in a bowl of water or wearing a water-filled glass hemisphere over the eye. Neither idea was practically implementable in da Vinci's time.[9]:9 He did not suggest his idea be used for correcting vision, as he was more interested in learning about the mechanisms of accommodation of the eye.[8]
Descartes proposed another idea in 1636: a glass tube filled with liquid placed in direct contact with the cornea. The protruding end was to be composed of clear glass, shaped to correct vision; however, the idea was impracticable since it rendered blinking impossible.
In 1801, Thomas Young made a basic pair of CLs based on Descartes' model. He used wax to affix water-filled lenses to his eyes, which neutralized its refractive power. He then corrected for it with another pair of lenses.[9]
However, like da Vinci's, Young's device was not intended to correct refraction errors. Sir John Herschel, in a footnote of the 1845 edition of the Encyclopedia Metropolitana, posed two ideas for the visual correction: the first "a spherical capsule of glass filled with animal jelly", and "a mould of the cornea" that could be impressed on "some sort of transparent medium".[10] Though Herschel reportedly never tested these ideas, they were both later advanced by several independent inventors such as Hungarian Dallos with István Komáromy (1929), who perfected a method of making molds from living eyes. This enabled the manufacture of lenses that, for the first time, conformed to the actual shape of the eye.

It was not until 1887 that German glassblower F. E. Muller produced the first eye covering to be seen through and tolerated.[11] In 1888, German ophthalmologist Adolf Gaston Eugen Fick constructed and fitted the first successful contact lens.[12] While working in Zürich, he described fabricating afocal scleral contact shells, which rested on the less sensitive rim of tissue around the cornea, and experimentally fitting them: initially on rabbits, then on himself, and lastly on a small group of volunteers. These lenses were made from heavy blown glass and were 18–21 mm in diameter. Fick filled the empty space between cornea/callosity and glass with a dextrose solution. He published his work, "Contactbrille", in the journal Archiv für Augenheilkunde in March 1888.
Fick's lens was large, unwieldy, and could only be worn for a couple of hours at a time. August Müller in Kiel, Germany, corrected his own severe myopia with a more convenient glass-blown scleral contact lens of his own manufacture in 1888.[13]
Also in 1887, Louis J. Girard invented a similar scleral form of contact lens.[14] Glass-blown scleral lenses remained the only form of contact lens until the 1930s when polymethyl methacrylate (PMMA or Perspex/Plexiglas) was developed, allowing plastic scleral lenses to be manufactured for the first time. In 1936, optometrist William Feinbloom introduced plastic lenses, making them lighter and more convenient.[15] These lenses were a combination of glass and plastic. In 1940, German optometrist Heinrich Wöhlk produced plastic lenses, based on experiments performed during the 1930s.
In 1949, the first "corneal" lenses were developed.[16][17][18][19] These were much smaller than the original scleral lenses, as they sat only on the cornea rather than across all of the visible ocular surface, and could be worn up to sixteen hours a day. PMMA corneal lenses became the first CLs to have mass appeal through the 1960s, as lens designs became more sophisticated with improving manufacturing (lathe) technology.
Early corneal lenses of the 1950s and ’60s were relatively expensive and fragile, resulting in the development of a market for CLs insurance. Replacement Lens Insurance, Inc. (now known as RLI Corp.) phased out its original flagship product in 1994 after contacts became more affordable and easier to replace.
One major disadvantage of PMMA lenses is that they allow no oxygen to get through to the conjunctiva and cornea, causing a number of adverse and potentially serious clinical effects. By the end of the 1970s, then through the ’80s and ’90s, a range of oxygen-permeable but rigid materials were developed to overcome this problem. Chemist Norman Gaylord played a prominent role in the development of these new, oxygen-permeable CLs.[20] Collectively, these polymers are referred to as "rigid gas permeable" or "RGP" materials or lenses. Though all the above CL types—sclerals, PMMAs and RGPs—could be correctly referred to as "rigid" or "hard", the latter term is now used to the original PMMAs, which are still occasionally fitted and worn, whereas "rigid" is a generic term for all these lens types; thus hard lenses (PMMAs) are a subset of rigid CLs. Occasionally, the term "gas permeable" is used to describe RGPs, which is somewhat misleading as soft CLs are also gas permeable in that they allow oxygen to get through to the ocular surface.

The principal breakthrough in soft lenses was made by Czech chemists Otto Wichterle and Drahoslav Lím who published their work "Hydrophilic gels for biological use" in the journal Nature in 1959.[21] In 1965 National Patent Development Corporation (NPDC) bought the American rights to produce the lenses and then sublicensed the rights to Bausch & Lomb which started to manufacture them in the United States.[22] The Czech scientists’ work led to the launch of the first soft (hydrogel) CLs in some countries in the 1960s and the first approval of the Soflens material by the U.S. Food and Drug Administration (FDA) in 1971. These softs were soon prescribed more often than rigids, due to the immediate and much greater comfort (rigids require a period of adaptation before full comfort, if any, is achieved). Polymers from which soft lenses are manufactured improved over the next 25 years, primarily in terms of increasing oxygen permeability, by varying the ingredients. In 1972, British optometrist Rishi Agarwal was the first to suggest disposable soft CLs.[23][24]
In 1998, an important development was the launch of the first silicone hydrogels onto the market by Ciba Vision in Mexico. These new materials encapsulated the benefits of silicone—which has extremely high oxygen permeability—with the comfort and clinical performance of the conventional hydrogels that had been used for the previous 30 years. These CLs were initially advocated primarily for extended (overnight) wear, although more recently, daily (no overnight) wear silicone hydrogels have been launched.
In a slightly modified molecule, a polar group is added without changing the structure of the silicone hydrogel. This is referred to as the Tanaka monomer because it was invented and patented by Kyoichi Tanaka of Menicon Co. of Japan in 1979. Second-generation silicone hydrogels, such as galyfilcon A (Acuvue Advance, Vistakon) and senofilcon A (Acuvue Oasys, Vistakon), use the Tanaka monomer. Vistakon improved the Tanaka monomer even further and added other molecules, which serve as an internal wetting agent.[25]
Comfilcon A (Biofinity, CooperVision) was the first third-generation polymer. Its patent claims that the material uses two siloxy macromers of different sizes that, when used in combination, produce very high oxygen permeability (for a given water content). Enfilcon A (Avaira, CooperVision) is another third-generation material that is naturally wettable; its water content is 46%.[25]
Types
CLs are classified in many different ways: by their primary function, material, wear schedule (how long a lens can be worn), and replacement schedule (how long before a lens needs to be discarded).
Functions
Corrective contact lenses
Corrective CLs are designed to improve vision, most commonly by correcting refractive error. This is done by directly focusing light so it enters the eye with the proper power for clear vision. Recently, there has been renewed interest in orthokeratology, the correction of myopia by deliberate overnight flattening of the corneal epithelium, leaving the eye without a refractive error during the day.
A spherical CL bends light evenly in every direction (horizontally, vertically, etc.). They are typically used to correct myopia and hypermetropia. A toric CL has a different focusing power horizontally than vertically, and as a result can correct for astigmatism. Some spherical rigid lenses can also correct for astigmatism. (See below.) Because a toric lens must have the proper orientation to correct for a person's astigmatism, such a CL must have additional design characteristics to prevent it from rotating away from the ideal alignment. This can be done by weighting the bottom of the lens or by using other physical characteristics to rotate the lens back into position. Some toric CLs have marks or etchings that can assist the eye doctor or the user in fitting the lens. First disposable toric CLs were introduced in 2000 by Vistakon.
Correction of presbyopia (a need for a reading prescription different from the prescription needed for distance) presents an additional challenge in the fitting of CLs. Two main strategies exist: multifocal CLs and monovision.
Multifocal contact lenses (e.g. bifocals or progressives) are comparable to spectacles with bifocals or progressive lenses because they have multiple focal points. Multifocal CLs are typically designed for constant viewing through the center of the lens, but some designs do incorporate a shift in lens position to view through the reading power (similar to bifocal glasses).
Monovision[26] is the use of single vision lenses (one focal point per lens) to focus an eye (typically the dominant one) for distance vision and the other for near work. The brain then learns to use this setup to see clearly at all distances. A technique called modified monovision uses multifocal lenses and also specializes one eye for distance and the other for near, thus gaining the benefits of both systems. Alternatively, a person may simply wear reading glasses over their distance contact lenses. Care is advised for persons with a previous history of strabismus and those with significant phorias, who are at risk of eye misalignment under monovision.[27] Studies have shown no adverse affect to driving performance in adapted monovision contact lens wearers.[28]
Other types of vision correction
For those with certain color deficiencies, a red-tinted "X-Chrom" CL may be used. Although such a lens does not restore normal color vision, it allows some colorblind people to distinguish colors better.[29][30] Red-filtering CLs can also be an option for extreme light sensitivity in some visual deficiences such as achromatopsia.[31]
ChromaGen CLs have been used and shown to have some limitations with vision at night although otherwise producing significant improvements in color vision.[32] An earlier study showed very significant improvements in color vision and patient satisfaction.[33]
Later work that used these ChromaGen lenses with dyslexics in a randomised, double-blind, placebo controlled trial showed highly significant improvements in reading ability over reading without the lenses.[34] This system has been granted FDA approval for use in the U.S.
Magnification is another area being researched for future CL applications.[35] Embedding of telescopic lenses and electronic components suggests that future uses of CLs may become extremely diverse. However, there are still barriers that prevent transition of these technologies from research and development to practical application and commercial availability.
Cosmetic contact lenses

A cosmetic CL is designed to change the appearance of the eye. These lenses may, of course, also correct refractive error. Although many brands of CLs are lightly tinted to make them easier to handle, cosmetic lenses worn to change eye color are far less common, accounting for only 3% of CL fits in 2004.[36]
FDA in the U.S. frequently labels non-corrective cosmetic CLs as decorative contact lenses. Like any CLs, cosmetic lenses carry risks of mild to serious complications, including ocular redness, irritation and infection.[37]
Due to their medical nature, color contacts, similar to regular ones, are illegal to purchase in the U.S. without valid prescription. Those with perfect vision can buy color contacts for cosmetic reasons, but they still need their eyes to be measured for a "plano" prescription, meaning one with zero vision correction. This is for safety reasons so the lenses will fit the eye without causing irritation or redness.[38]
Some colored contact lenses completely cover the iris, thus dramatically changing eye colour. Other colored contact lenses merely tint the iris, highlighting and beautifying its natural colour.[39] A new trend in Japan, South Korea and China is the circle contact lens, which extend the appearance of the iris onto the sclera by having a dark tinted area all around. The result is an appearance of a bigger, wider iris, a look reminiscent of dolls' eyes.[40]
One of the drawbacks of cosmetic lenses is not knowing how they will look before physically trying them on. This has led to an industry where lens retailers are heavily influenced by cutting edge digital fashion technology, specifically the Virtual Dressing Room technology. Virtual Dressing Room technology offers users the option to upload a photo so they can virtually try-on different lenses and experience how they will look before committing to a purchase. Examples of retailers that currently offer this technology are Freshlook Color Studios and Colorful Eyes.[41] [42]
Cosmetic lenses can have more direct medical applications. For example, some CLs can restore the appearance and, to some extent the function, of a damaged or missing iris.
Therapeutic scleral lenses

A scleral lens is a large, firm, oxygen permeable CL that rests on the sclera and creates a tear-filled vault over the cornea. The cause of this unique positioning is usually relevant to a specific patient whose cornea is too sensitive to support the lens directly. Scleral lenses may be used to improve vision and reduce pain and light sensitivity for people suffering from a growing number of disorders or injuries to the eye, such as severe dry eye syndrome (Kerotanconjuctivis sicca), microphthalmia, keratoconus, corneal ectasia, Stevens–Johnson syndrome, Sjögren's syndrome, aniridia, neurotrophic keratitis (aneasthetic corneas), complications post-LASIK, high order Aberrations of the eye, complications post-corneal transplant and pellucid degeneration. Injuries to the eye such as surgical complications, distorted corneal implants, as well as chemical and burn injuries also may be treated with scleral lenses. [43]
Therapeutic soft lenses
Soft lenses are often used in the treatment and management of non-refractive disorders of the eye. A bandage CL protects an injured or diseased cornea from the constant rubbing of blinking eyelids thereby allowing it to heal.[44] They are used in the treatment of conditions including bullous keratopathy, dry eyes, corneal abrasions and erosion, keratitis, corneal edema, descemetocele, corneal ectasis, Mooren's ulcer, anterior corneal dystrophy, and neurotrophic keratoconjunctivitis.[45] Contact lenses that deliver drugs to the eye have also been developed.[46]
Materials
Rigid lenses
Glass lenses were never comfortable enough to gain widespread popularity. The first lenses to do so were those made from polymethyl methacrylate (PMMA or Perspex/Plexiglas), now commonly referred to as "hard" lenses. Their main disadvantage is they do not allow oxygen to pass through to the cornea, which can cause a number of adverse and often serious clinical events.
Starting in the late 1970s, improved rigid materials which were oxygen-permeable were developed. CLs made from these materials are called rigid gas permeable lenses or 'RGPs'.
A rigid lens is able to replace the natural shape of the contact (cornea) with a new refracting surface. This means that a spherical rigid CL can correct for astigmatism. Rigids can also be made as a front-toric, back-toric, or bitoric. This is different from a spherical CL in that one or both surfaces of the lens deliver a toric correction. Rigids can also correct for corneal irregularities, such as keratoconus. In most cases, patients with keratoconus see better through rigids than through glasses. Rigids are more chemically inert, allowing them to be worn in more challenging environments than soft lenses.
Soft lenses
While rigid lenses have been around for about 120 years, soft lenses are a much more recent development. The principal breakthrough in soft CLs made by Otto Wichterle led to the launch of the first soft (hydrogel) lenses in some countries in the 1960s and the approval of the "Soflens" daily material (polymacon) by the FDA in the U.S. in 1971. Softs are usually comfortable right after insertion, while rigids require a period of adaptation before some comfort, if any, is achieved. Biggest improvements to soft-lens polymers have been increasing oxygen permeability, lens wetability, and overall comfort.
In 1998, silicone hydrogels became available. These materials have both the extremely high oxygen permeability of silicone and the comfort and clinical performance of the conventional hydrogels. Because silicone allows more oxygen permeability than water, oxygen permeability of silicone hydrogels is not tied to the CL’s water content. Lenses have now been developed with so much oxygen permeability that they are approved for overnight wear (extended wear). Lenses approved for daily wear are also available in silicone hydrogel materials.[47]
Disadvantages of silicone hydrogels are that they are slightly stiffer and the lens surface can be hydrophobic, thus less "wettable" – factors that influence comfort of lens use. New manufacturing techniques and changes to multipurpose solutions have minimized these effects. A surface modification process called plasma coating alters the lens surface’s hydrophobic nature. Another technique incorporates internal rewetting agents to make the lens surface hydrophilic. A third process uses longer backbone polymer chains that results in less cross linking and increased wetting without surface alterations or additive agents.
Hybrid
A small number of hybrid lenses exist. Typically these CLs consist of a rigid center and a soft "skirt". Similar technique is "piggybacking" of a smaller, rigid lens on the surface of a larger, soft lens. These techniques are often chosen to give the vision correction benefits of a rigid lens and the comfort of a soft lens. As of 2014, this is a new technology that only a few companies provide.[48]
Wear schedule
A "daily wear" (DW) CL is designed to be worn for one day and removed prior to sleeping. An "extended wear" (EW) CL is designed for continuous overnight wear, typically for up to 6 consecutive nights. Newer materials, such as silicone hydrogels, allow for even longer wear periods of up to 30 consecutive nights; these longer-wear CLs are often referred to as "continuous wear" (CW). EW and CW CLs can be worn overnight because of their high oxygen permeability. While awake, the eyes are mostly open, allowing oxygen from the air to dissolve into the tears and pass through the lens to the cornea. While asleep, oxygen is supplied from the blood vessels in the back of the eyelid. A lens hindering passage of oxygen to the cornea causes corneal hypoxia which can result in serious complications, such as corneal ulcer that, if left untreated, can permanently decrease vision. EW and CW CLs typically allow for a transfer of 5–6 times more oxygen than conventional softs, allowing the cornea to remain healthy, even with closed eyelids.
Wearing lenses designed for daily wear overnight has an increased risk for corneal infections, corneal ulcers and corneal neovascularization—this latter condition, once it sets in, cannot be reversed and will eventually spoil vision acuity through diminishing corneal transparency. The most common complication of extended wear is giant papillary conjunctivitis (GPC), sometimes associated with a poorly fitting contact lens.
Replacement schedule
CLs are often categorized by their replacement schedule. Single use lenses (called 1-day or daily disposables, such as Dailies Total One or One Day Acuvue Moist) are discarded after one use. Because they do not have to stand up to the wear and tear of repeated uses, these lenses can be made thinner and lighter, greatly improving their comfort. Lenses replaced frequently gather fewer deposits of allergens and germs, making these lenses preferable for patients with ocular allergies or for those who are prone to infection. Single-use lenses are also useful for people who wear CLs infrequently, or when losing a lens is likely or not easily replaced (such as when on vacation). They are also considered useful for children because cleaning or disinfecting is not needed, leading to improved compliance.
Other disposable CLs are designed for 2- or 4-week replacement. Quarterly or annual lenses, which used to be very common, have been discontinued. Rigid gas permeable lenses are very durable and may last for several years without the need for replacement. PMMA hards were very durable and were commonly worn for 5 to 10 years, but had several drawbacks.
Lenses with different replacement schedules can be made of the same material. Although the materials are alike, differences in the manufacturing processes determine if the resulting lens will be a "daily disposable" or one recommended for 2- or 4-week replacement.
In the U.S., CL manufacturers must prove to the FDA that a lens is safe before it can be sold to the public. Typically, the prescribing doctor instructs patients to follow the same limitations used during those studies. This included wear time and replacement schedule.
Manufacturing
Typically, soft CLs are mass-produced, while rigids are custom-made to exact specifications for the individual patient.
- Spin-cast lenses – A soft lens manufactured by whirling liquid silicone in a revolving mold at high speed.[49]
- Diamond turning – This type is cut and polished on a CNC lathe.[49] The lens starts out as a cylindrical disk held in the jaws of the lathe that is equipped with an industrial-grade diamond as the cutting tool. The CNC lathe may turn at nearly 6000 RPM as the cutter removes the desired amount of material from the inside of the lens. The concave (inner) surface of the lens is then polished with some fine abrasive paste, oil, and a small polyester cotton ball turned at high speeds. To hold the delicate lens in reverse manner, wax is used as an adhesive. The lens’ convex (outer) surface is thus cut and polished by the same process. This method can be used to shape rigid as well as soft lenses. In the case of softs, the lens is cut from a dehydrated polymer that is rigid until water is reintroduced.
- Molded – Molding is used to manufacture some brands of soft CLs. Rotating molds are used and the molten material is added and shaped by centripetal forces. Injection molding and computer control are also used to create nearly perfect lenses.[50] The CL is kept moist throughout the entire molding process and is never dried and rehydrated.
Many companies make CLs. In the U.S.. there are four major manufacturers:[51]
- Valeant Pharmaceuticals: through its Bausch & Lomb subsidiary.
- Novartis: through its Alcon subsidiary.
- The Cooper Companies: through its CooperVision subsidiary.
- Johnson & Johnson; maker of Acuvue lenses.
Prescriptions
The parameters specified in a CL-prescription may include:
- Material / Brand name
- Base curve radius (BC, BCR)
- Diameter (D, OAD)
- Power in diopters
- Center thickness (CT)
Prescriptions for CLs and glasses may be similar, but are not interchangeable. Prescribing of CLs is usually restricted to various combinations of ophthalmologists, optometrists and opticians. An eye examination is needed to determine an individual's suitability for CL wear. This typically includes a refraction to determine the proper power of the lens and an assessment of the health of the eye's anterior segment. Many eye diseases prohibits CL wear, such as active infections, allergies, and dry eye.[52] Keratometry is especially important in the fitting of rigid lenses.
United States
CLs are prescribed by ophthalmologists, optometrists, or specially licensed opticians under the supervision of an eye doctor. CLs can typically be ordered at the office that conducts the eye exam and fitting. The Fairness to Contact Lens Consumers Act[53] gives consumers the right to obtain a copy of their CL prescription, allowing them to fill it at the business of their choice, including online discount sites.
Complications

CLs are generally safe as long as they are used correctly. Complications from CL wear affect roughly 5% of wearers yearly.[54] Improper use of a CL may affect the eyelid, the conjunctiva, and, most of all, the whole structure of the cornea.[54] Poor lens care can lead to infections by various microorganisms including bacteria, fungi, and Acanthamoeba (Acanthamoeba keratitis).
Many complications arise when CLs are worn not as prescribed (improper wear schedule or lens replacement). Sleeping in lenses not designed or approved for extended wear is a common cause of complications. Many people go too long before replacing their contacts, wearing lenses designed for 1, 14, or 30 days of wear for multiple months or years. While this does save on the cost of lenses, it risks permanent damage to the eye and even loss of sight.
One of the major factors that causes CL complications is that the lens is an oxygen barrier. The cornea needs a constant supply of oxygen to remain completely transparent and function as it should; it normally gets that oxygen from the surrounding air while awake, and from the blood vessels in the back of the eyelid while asleep. The most prominent risks associated with long-term, chronic low oxygen to the cornea include corneal neovascularization, increased epithelial permeability, bacterial adherence, microcysts, corneal edema, endothelial polymegethism, dry eye and potential increase in myopia.[55] That is why much of the research into the latest soft and rigid CL-materials has centered on improving oxygen transmission through the lens.
Mishandling of CLs can also cause problems. Corneal abrasions can increase the chances of infection.[56] When combined with improper cleaning and disinfection of the lens, a risk of infection further increases. Decreased corneal sensitivity following extended CL wear may cause a patient to miss some of the earliest symptoms of such complications.[57]
The way CLs interact with the natural tear layer is a major factor in determining lens comfort and visual clarity. People suffering from dry eyes are particularly vulnerable to discomfort and episodes of brief blurry vision. Proper lens selection can minimize these effects.
Long-term wear (over 5 years) of CLs may "decrease the entire corneal thickness and increase the corneal curvature and surface irregularity."[58] Long-term wear of rigid contacts is associated with decreased corneal keratocyte density[59] and increased number of epithelial Langerhans cells.[60]
All CLs sold in the U.S. are studied and approved as safe by the FDA when specific handling and care procedures, wear schedules, and replacement schedules are followed.
Usage
Before touching the CL or the eye, it is important to wash hands thoroughly with soap and rinse well. Soaps containing moisturizers or allergens should be avoided as these can cause eye irritation.[61] Drying of hands using towels or tissues prior to handling CLs can transfer lint (fluff) to the hands and, subsequently, to the lenses, causing irritation upon insertion. Towels, unless freshly laundered on high temperature wash, are frequently contaminated with large quantities of bacteria and, as such, should be avoided when handling lenses. Dust, lint and other debris may collect on the outside of CLs. Again, hand contact with this material, prior to handling CLs, may transfer it to the lenses themselves. Rinsing the case under a source of clean running water, prior to opening it, can help alleviate this problem. Next the lens should be removed from its case and inspected for defects (e.g. splits, folds, lint). A 'gritty' or rough appearance to the lens surface may indicate that a considerable quantity of proteins, lipids and debris has built up on it and that additional cleaning is required; this is often accompanied and felt by unusually high irritation upon insertion.
Make sure the soft lens is not inserted inside-out. Edge of a lens turned inside out has a different appearance, especially when the lens is slightly folded. Insertion of an inside-out lens for a brief time (less than one minute) should not cause any damage to the eye, but a discomfort that won't go away will tell you the lens is not in the proper orientation. Some brands of lenses have markings (e.g. numbers) on the rim that make it easier to tell the front of the lens from the back.
The technique for removing or inserting a contact lens varies depending upon whether the lens is soft or rigid. There are many subtle variations to insertion and removal techniques. Because of differences in anatomy, manual dexterity, and visual limitations, every person must find the technique that works best for them. In all cases, the insertion and removal of lenses requires some training and practice on part of the user.
Insertion

CLs are typically inserted into the eye by placing them on the pad of the index or middle finger with the concave side upward and then using that finger to place the lens on the eye. Rigid lenses should be placed directly on the cornea. Soft lenses may be placed on the sclera (white of the eye) and then slid into place. The other hand is used to keep the eye wide open. Alternatively, the user may close their eyes and then look towards their nose, sliding the lens into place over the cornea.
Problems may arise if the lens folds, turns inside-out, slides off the finger prematurely, or adheres more tightly to the finger than the eye surface. A drop of solution may help the lens adhere to the eye.
When the lens first contacts the eye, it should be comfortable. A brief period of irritation may occur, caused by a difference in pH and/or salinity between that of the lens solution and the tear.[62][63] This discomfort fades quickly as the solution drains away and is replaced by the natural tears. However, if irritation persists, the cause could be a dirty, damaged, or inside-out lens. Removing and inspecting it for damage and proper orientation, and re-cleaning if necessary, should correct the problem. If discomfort continues, the lens should not be worn. In some cases, taking a break from lens wear for a day may correct the problem. In case of severe discomfort, or if it does not resolve by the next day, the person should be seen as soon as possible by an eye doctor to rule out potentially serious complications.
Removal

Removing CLs incorrectly could result in damage to the lens and injury to the eye so certain precautions must be taken. Rigid contacts can best be removed by pulling the eyelid tight and then blinking, whereupon the lens drops out. With one finger on the outer corner of the eyelids, or lateral canthus, the person stretches the eyelids towards the ear; the increased tension of the eyelid margins against the edge of lens allows the blink to break the capillary action that adheres the lens to the eye. The other hand is typically cupped underneath the eye to catch the lens as it drops out. For soft lenses, which have a stronger adherence to the eye surface, this technique is less suitable.
A soft CL may be removed by pinching the edge between the thumb and index finger. Moving the lens off the cornea first can improve comfort during removal and reduce risk of scratching the cornea with a fingernail. Also possible—and for the experienced user generally much easier—to push or pull a soft lens far enough to the side or bottom of the eyeball to get it to fold then fall out, without pinching and thereby damaging it. Do not use these techniques on a rigid lens—it will likely scratch the cornea.
There are also small tools specifically for removing lenses. Usually made of flexible plastic, they resemble small tweezers, or plungers that suction onto the front of the lens. Typically these tools are only used with rigid lenses. Extreme care must be exercised when using mechanical tools or fingernails to insert or remove CLs. Long and/or fancy nails are a definite danger, as are those unclean or chipped. Scratching—let alone accidental gashing—the cornea is not only very painful but also poses serious hazards on eye health and vision acuity, not to mention how instantly it reddens the eye and spoils "the look".
Care

Lens care varies depending on material and wear schedule. Daily disposables are discarded after a single use and thus require no cleaning. Other lenses need regular cleaning and disinfecting to prevent surface coating and infections.
There are many ways to clean and care for contact lenses, typically called care systems or lens solutions:
- Multipurpose solutions
- Multipurpose solutions are the most common method for rinsing, disinfecting, cleaning, and storing soft lenses. In 2002, concerns were raised that multipurpose solutions are not effective at disinfecting Acanthamoeba from the lens.[64] In May 2007, one brand of multipurpose solution was recalled due to a cluster of Acanthamoeba infections.[65][66] Since then, studies showed that multipurpose solutions are ineffective against Acanthamoebae.[67][68][69] The latest multipurpose solutions also contain ingredients that improve the surface wetability and comfort of silicone hydrogel lenses.
- Hydrogen peroxide can be used to disinfect contact lenses.[70] Care should be taken not to get hydrogen peroxide in the eye because it is very painful and irritating. With "two-step" products, the hydrogen peroxide must be rinsed away with saline before the lenses may be worn. "One-step" systems allow the hydrogen peroxide to react completely, becoming pure water. Thus "one-step" hydrogen peroxide systems do not require the lenses to be rinsed prior to insertion, provided the solution has been given enough time to react. An exposure time of 2-3 hours to 3% H
2O
2 (non neutralized solution) is sufficient to kill bacteria, HIV, fungi, and Acanthamoeba.[71][72] This can be achieved by using a "two-step" product or a "one-step" tablet system if the catalytic tablet isn't added before 2-3 hours.[72] However, the "one-step" catalytic disk systems are not effective against Acanthamoeba.[72]
- Hydrogen peroxide can be used to disinfect contact lenses.[70] Care should be taken not to get hydrogen peroxide in the eye because it is very painful and irritating. With "two-step" products, the hydrogen peroxide must be rinsed away with saline before the lenses may be worn. "One-step" systems allow the hydrogen peroxide to react completely, becoming pure water. Thus "one-step" hydrogen peroxide systems do not require the lenses to be rinsed prior to insertion, provided the solution has been given enough time to react. An exposure time of 2-3 hours to 3% H
- Enzymatic cleaner – Used for cleaning protein deposits off lenses, usually weekly, if the daily cleaner is not sufficient. Typically, this cleaner is in tablet form.
- Ultraviolet, vibration, or ultrasonic devices – Used to both disinfect and clean CLs. The lenses are inserted inside the portable device (running on batteries and/or plug-in) for 2 to 6 minutes during which both the microorganisms and protein build-up are thoroughly cleaned. These devices are not usually available in optic retailers but are in some electro-domestic stores.[73][74][75]
- Saline solution
- Sterile saline is used for rinsing the lens after cleaning and preparing it for insertion. Saline solutions do not disinfect, so it must be used in conjunction with some type of disinfection system. One advantage to saline is that it cannot cause an allergic response, so it is well suited for individuals with sensitive eyes or strong allergies.
- Daily cleaner
- Used to clean lenses on a daily basis. A few drops of cleaner are applied to the lens while it rests in the palm of the hand; the lens is rubbed for about 20 seconds with a clean fingertip (depending on the product) on each side. Lens must then be rinsed. This system is commonly used to care for rigid lenses.
Aside from cleaning the CLs, it is highly advised to also clean the cases to avoid any possible infection. Replacing the case monthly, and storing it in a clean and safe environment is also recommended.[76]
CLs can be mechanically cleaned of more substantial protein, lipid and debris build up by rubbing them between the clean pad of a finger and the palm of a hand, using a small amount of cleaning fluid as a lubricant. However, this method does not sterilize the lenses and so should only be performed prior to a full sterilization cycle (e.g. when putting the CLs away the night before).
Some products must only be used with certain types of CLs. Water alone will not at all disinfect the lens, and can lead to lens contamination causing potentially irreparable harm to the eye.
CL solutions often contain preservatives such as benzalkonium chloride and benzyl alcohol. Preservative-free products usually have shorter shelf lives, but are better suited for individuals with an allergy or sensitivity to a preservative. In the past, thiomersal was used as a preservative. In 1989, thiomersal was responsible for about 10% of problems related to CLs.[77] As a result, most products no longer contain thiomersal.
Current research
A large segment of current CL-research is directed towards the treatment and prevention of conditions resulting from CL contamination and colonization by foreign organisms. Clinicians tend to agree that the most significant complication of CL wear is microbial keratitis and that the most predominant microbial pathogen is Pseudomonas aeruginosa.[78] Other organisms are also major causative factors in bacterial keratitis associated with CL wear, although their prevalence varies across different locations. These include both the Staphylococcus species (aureus and epidermidis) and the Streptococcus species, among others.[79][80] Microbial keratitis is a serious focal point of current research due to its potentially devastating effect on the eye, including severe vision loss.[81]
One specific research topic of interest is how microbes such as Pseudomonas aeruginosa invade the eye and cause infection. Although the pathogenesis of microbial keratitis is not well understood, many different factors have been investigated. One group of researchers showed that corneal hypoxia exacerbated Pseudomonas binding to the corneal epithelium, internalization of the microbes, and induction of the inflammatory response.[82] One way to alleviate hypoxia is to increase the amount of oxygen transmitted to the cornea. Although silicone-hydrogel lenses almost eliminate hypoxia in patients due to their very high levels of oxygen transmissibility,[83] they also seem to provide a more efficient platform for bacterial contamination and corneal infiltration than other conventional hydrogel soft CLs. A recent study showed that Pseudomonas aeruginosa and Staphylococcus epidermis adhere much more strongly to unworn silicone hydrogel CLs than conventional hydrogel lenses and that adhesion of Pseudomonas aeruginosa was 20 times stronger than that of Staphylococcus epidermidis.[84] This might partly explain why Pseudomonas infections are the most predominant. However, another study conducted with worn and unworn silicone and conventional hydrogel CLs showed that worn silicone CLs were less prone to Staphylococcus epidermidis colonization than conventional hydrogel lenses.[85]
Another important area of CL-research deals with patient compliance. Compliance is a major issue[86] pertaining to the use of contact lenses because patient noncompliance often leads to contamination of the lens, storage case, or both.[87][88][89] However, careful users can extend the wear of lenses through proper handling: there is, unfortunately, no disinterested research on the issue of "compliance" or the length of time a user can safely wear a lens beyond its stated use. The introduction of multipurpose solutions and daily disposable lenses have helped to alleviate some of the problems observed from inadequate cleaning but new methods of combating microbial contamination are currently being developed. A silver-impregnated lens case has been developed which helps to eradicate any potentially contaminating microbes that come in contact with the lens case.[90] Additionally, a number of antimicrobial agents are being developed that have been embedded into CLs themselves. CLs with covalently attached Selenium molecules have been shown to reduce bacterial colonization without adversely affecting the cornea of a rabbit eye[91] and octylglucoside used as a CL surfactant significantly decreases bacterial adhesion.[92] These compounds are of particular interest to CL manufacturers and prescribing optometrists because they do not require any patient compliance to effectively attenuate the effects of bacterial colonization.
A recent area of research is in the field of bionic lenses. These are visual displays that include built-in electric circuits and light-emitting diodes and can harvest radio waves for their electric power. Bionic lenses can display information beamed from a mobile device overcoming the small display size problem. The technology involves embedding nano and microscale electronic devices in lenses. These lenses will also need to have an array of microlenses to focus the image so that it appears suspended in front of the wearer’s eyes. The lens could also serve as a head-up display for pilots or gamers.[93]
Drug administration through CLs is also becoming an area of research. One application is a CL that releases anesthesia to the eye for post-surgery pain relief, especially after PRK (photorefractive keratectomy) in which the healing process takes several painful days. One experiment shows that silicone CLs that contain vitamin E deliver pain medication for up to 7 days compared with less than 2 hours in usual lenses.[93]
A prototype of the much-awaited telescopic CLs was recently unveiled at a meeting of the AAAS - the American Association for the Advancement of Science in San Jose. Giving wearers the ability to zoom in and out with the wink of an eye, this revolutionary CL identifies and differentiates winks from blinks, aiding wearers to shuffle between normal and magnified vision.
See also
References
- ↑ NM Farandos; AK Yetisen; MJ Monteiro; CR Lowe; SH Yun (2014). "Contact Lens Sensors in Ocular Diagnostics.". Advanced Healthcare Materials. doi:10.1002/adhm.201400504.
- ↑ Barr, J. "2004 Annual Report". Contact Lens Spectrum. January 2005.
- 1 2 Nichols, Jason J., et al "ANNUAL REPORT: Contact Lenses 2010". January 2011.
- ↑ Morgan, Philip B., et al. "International Contact Lens Prescribing in 2010". Contact Lens Spectrum. October 2011.
- ↑ Agarwal, R. K. (1969), Contact Lens Notes, Some factors concerning patients' motivation, The Optician, 10 January, pages 32-33 (published in London, England).
- ↑ Sokol, JL; Mier, MG; Bloom, S; Asbell, PA (1990). "A study of patient compliance in a contact lens-wearing population". The CLAO journal : official publication of the Contact Lens Association of Ophthalmologists, Inc. 16 (3): 209–13. PMID 2379308.
- ↑ Contact Lens Market Research and Industry Analysis
- 1 2 Heitz, RF and Enoch, J. M. (1987) "Leonardo da Vinci: An assessment on his discourses on image formation in the eye." Advances in Diagnostic Visual Optics 19—26, Springer-Verlag.
- 1 2 Leonard G. Schifrin and William J. Rich (December 1984). The Contact Lens Industry: Structure, Competition, and Public Policy. United States Office of Technology Assessment.
- ↑ "The History of Contact Lenses." eyeTopics.com. Accessed 18 October 2006.
- ↑ "Contact Lenses - A Consumer Guide from AllAboutVision.com". All About Vision. Retrieved 26 March 2015.
- ↑ "Adolf Eugen Fick (1852-1937)". Retrieved 26 March 2015.
- ↑ Pearson, RM; Efron, N (1989). "Hundredth anniversary of August Müller's inaugural dissertation on contact lenses". Survey of ophthalmology. 34 (2): 133–41. doi:10.1016/0039-6257(89)90041-6. PMID 2686057.
- ↑ Hellemans, Alexander; Bunch, Bryan (1988). The Timetables of Science. Simon & Schuster. p. 367. ISBN 0671621300.
- ↑ Robert B. Mandell. Contact Lens Practice, 4th Edition. Charles C. Thomas, Springfield, IL, 1988.
- ↑ U.S. Patent No. 2,510,438, filed 28 February 1948.
- ↑ "The Corneal Lens", The Optician, 2 September 1949, pp. 141–144.
- ↑ "Corneal Contact Lenses", The Optician, 9 September 1949, p. 185.
- ↑ "New Contact Lens Fits Pupil Only", The New York Times, 11 February 1952, p. 27.
- ↑ Pearce, Jeremy (23 September 2007). "Norman Gaylord, 84; helped develop type of contact lens". (New York Times News Service). The Boston Globe. Retrieved 6 October 2007.
- ↑ Wichterle O, Lim D (1960). "Hydrophilic gels for biological use". Nature. 185 (4706): 117–118. doi:10.1038/185117a0.
- ↑ "CONTACT LENS HISTORY - Otto Wichterle". Retrieved 26 March 2015.
- ↑ Agarwal Rishi K (1972). "Some Thoughts on Soft Lenses". The Contact Lens. 4 (1): 28.
- ↑ "Editorial note". American Journal of Optometry and Physiological Optics. 65 (9): 744. 1988.
- 1 2 "Looking at Silicone Hydrogels Across Generations". Optometric Management. Retrieved 5 April 2009.
- ↑ Lebow, KA; Goldberg, JB (1975). "Characteristic of binocular vision found for presbyopic patients wearing single vision contact lenses". Journal of the American Optometric Association. 46 (11): 1116–23. PMID 802938.
- ↑ Zane F. Pollard; Marc F. Greenberg; Mark Bordenca; Joshua Elliott; Victoria Hsu (September 2011). "Strabismus Precipitated by Monovision". American Journal of Ophthalmology. 152 (3): 479–482. doi:10.1016/j.ajo.2011.02.008.
- ↑ Wood, Joanne M.; Wick, Kristan; Shuley, Vicki; Pearce, Brendon; Evans, Dean (1998-06-01). "The effect of monovision contact lens wear on driving performance". Clinical & Experimental Optometry. 81 (3): 100–103. ISSN 1444-0938. PMID 12482258.
- ↑ Hartenbaum, NP; Stack, CM (1997). "Color vision deficiency and the X-Chrom lens". Occupational Health & Safety. 66 (9): 36–40, 42. PMID 9314196.
- ↑ Siegel, IM (1981). "The X-Chrom lens. On seeing red". Survey of ophthalmology. 25 (5): 312–24. PMID 6971497.
- ↑ http://www.achromatopsia.info/red-contact-lenses/ Red contact lenses for achromats
- ↑ Swarbrick, HA; Nguyen, P; Nguyen, T; Pham, P (2001). "The ChromaGen contact lens system: Colour vision test results and subjective responses". Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 21 (3): 182–96. doi:10.1046/j.1475-1313.2001.00583.x. PMID 11396392.
- ↑ Harris D "Colouring Sight: A study of CL fittings with colour enhancing lenses" 'Optician' 8 June 1997
- ↑ Harris DA, MacRow-Hill SJ "Application of ChromaGen haploscopic lenses to patients with dyslexia: a double masked placebo controlled trial" Journal of the American Optometric Association 25/10/99.
- ↑ "Telescopic contact lens magnifies vision by 2.8 times on demand". Wired UK. Retrieved 26 March 2015.
- ↑ Morgan PB et al."International Contact Lens Prescribing in 2004: An analysis of more than 17,000 contact lens fits from 14 countries in 2004 reveals the diversity of contact lens practice worldwide." Contact Lens Spectrum. January 2005.
- ↑ Vanderbilt University Medical Center - Vanderbilt Eye Doctors Warn of the Dangers of Cosmetic Contact Lenses. Mc.vanderbilt.edu (19 April 2010). Retrieved on 2013-07-21.
- ↑ "Color Contacts". colorfuleyes.org. February 2016.
- ↑ "Coloured Contact Lenses". lenses-contact.co.uk.
- ↑ "How Do You Find the Right Circle Lens?". EyeCandy's. Retrieved 26 March 2015.
- ↑ "Freshlook Color Studio". Freshlook. Retrieved 28 September 2016.
- ↑ "Eye Color Changer". Colorful Eyes. Retrieved 28 September 2016.
- ↑ Caceres, Vanessa (June 2009). "Taking a second look at scleral lenses". ASCRS EyeWorld. Retrieved 18 May 2014.
- ↑ "Eye Health Guide - Eye Diseases, Eye Problems and Eye Conditions". All About Vision. Retrieved 26 March 2015.
- ↑ "45 COVERAGE ISSUES – SUPPLIES – DRUGS 11–91 45" (PDF). Centers for Medicare and Medicaid Services. Retrieved 1 March 2006.
- ↑ "Qmed is the world's only directory of pre-qualified suppliers to the medical device and in vitro diagnostics industry. - Qmed". Retrieved 26 March 2015.
- ↑ FDA Premarket Notification for "new silicone hydrogel lens for daily wear" 'July 2008.
- ↑ Hashemi E, Shaygan N, Asqari , Asqari S, Rezvan F (2014 March;). "ClearKone-SynergEyes or Rigid Gas Permeable Contact Lenses in Keratoconic Patients: A Clinical Decision". Eye & Contact Lens. 40 (2): 95–8. doi:10.1097/icl.0000000000000016. Check date values in:
|date=(help) - 1 2 Cassin, B. and Solomon, S. Dictionary of Eye Terminology. Gainesville, Florida: Triad Publishing Company, 1990.
- ↑ Manufacture of soft contact lenses. "Manufacture of soft contact lenses".
- ↑ Federal Trade Commission. "The Strength of Competition in the Sale of Rx Contact Lenses: An FTC Study". February 2005.
- ↑ Agarwal, R.K. (1970), Some reasons for not fitting contact lenses, The Optician, 4 December, page 623 (published in London, England).
- ↑ "Fairness to Contact Lens Consumers Act". 15 October 2003.
- 1 2 John Stamler. "Contact Lens Complications." eMedicine.com. 1 September 2004.
- ↑ "What's the Best Prescription for Healthy Contact Lens Wear?". Contact Lens Spectrum.
- ↑ "Corneal Abrasion in Emergency Medicine". Medscape Reference.
- ↑ Liu, Z.; Pflugfelder, S. (January 2000). "The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity". Ophthalmology. 107 (1): 105–111. doi:10.1016/S0161-6420(99)00027-5. PMID 10647727.
- ↑ Liu Z, Pflugfelder SC (January 2000). "The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity". Ophthalmology. 107 (1): 105–11. doi:10.1016/S0161-6420(99)00027-5. PMID 10647727.
- ↑ Hollingsworth JG, Efron N (June 2004). "Confocal microscopy of the corneas of long-term rigid contact lens wearers". Cont Lens Anterior Eye. 27 (2): 57–64. doi:10.1016/j.clae.2004.02.002. PMID 16303530.
- ↑ Zhivov A, Stave J, Vollmar B, Guthoff R (January 2007). "In vivo confocal microscopic evaluation of langerhans cell density and distribution in the corneal epithelium of healthy volunteers and contact lens wearers". Cornea. 26 (1): 47–54. doi:10.1097/ICO.0b013e31802e3b55. PMID 17198013.
- ↑ "How to Put Contacts in Your Eyes". CooperVision. Retrieved 20 November 2014.
use plain soap without any heavy moisturizers or perfumes. Rinse well and dry your hands. Again, this is to prevent transmitting anything unwanted to your eyes.
- ↑ "pH consistency and stability of contact lens solutions.". Retrieved 20 November 2014.
The pH of contact lens solutions has been implicated in the comfort of contact lenses on insertion.
- ↑ "Eye Care". CLH. Retrieved 20 November 2014.
- ↑ Hiti, K; Walochnik, J; Haller-Schober, E M; Faschinger, C; Aspöck, H (February 2002). "Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems". British Journal of Ophthalmology. 86 (2): 144–6. doi:10.1136/bjo.86.2.144. PMC 1771011
 . PMID 11815336.
. PMID 11815336. - ↑ Early Report of Serious Eye Infections Associated with Soft Contact Lens Solution. CDC health advisory. 25 May 2007. CDCHAN-00260-2007-05-25-ADV-N
- ↑ Acanthamoeba Keratitis --- Multiple States, 2005–2007. Center for Disease Control MMWR dispatch. 26 May 2007 / 56(Dispatch);1–3
- ↑ Johnston, S. P.; R. Sriram; Y. Qvarnstrom; S. Roy; J. Verani; J. Yoder; S. Lorick; J. Roberts; M. J. Beach; G. Visvesvara (2009). "Resistance of Acanthamoeba Cysts to Disinfection in Multiple Contact Lens Solutions". Journal of Clinical Microbiology. 47 (7): 2040–2045. doi:10.1128/JCM.00575-09. ISSN 0095-1137. PMC 2708465
 . PMID 19403771.
. PMID 19403771. - ↑ Padzik, Marcin; Lidia Chomicz; Jacek P. Szaflik; Agnieszka Chruścikowska; Konrad Perkowski; Jerzy Szaflik (2014). "In vitro effects of selected contact lens care solutions on Acanthamoeba castellanii strains in Poland". Experimental Parasitology. doi:10.1016/j.exppara.2014.06.014. ISSN 0014-4894.
- ↑ de Aguiar, Ana Paula Costa; Caroline de Oliveira Silveira; Mari Aline Todero Winck; Marilise Brittes Rott (2013). "Susceptibility of Acanthamoeba to multipurpose lens-cleaning solutions". Acta Parasitologica. 58 (3): 304–308. doi:10.2478/s11686-013-0143-9. ISSN 1230-2821.
- ↑ Hughes, Reanne; Kilvington, Simon (July 2001). "Comparison of Hydrogen Peroxide Contact Lens Disinfection Systems and Solutions against Acanthamoeba polyphaga". Antimicrobial Agents and Chemotherapy. 45 (7): 2038–43. doi:10.1128/AAC.45.7.2038-2043.2001. PMC 90597
 . PMID 11408220.
. PMID 11408220. - ↑ Hiti, K (2002). "Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems". British Journal of Ophthalmology. 86 (2): 144–146. doi:10.1136/bjo.86.2.144. ISSN 0007-1161. PMC 1771011
 . PMID 11815336.
. PMID 11815336. - 1 2 3 Hiti, K; J Walochnik; C Faschinger; E-M Haller-Schober; H Aspöck (2004). "One- and two-step hydrogen peroxide contact lens disinfection solutions against Acanthamoeba: How effective are they?". Eye. 19 (12): 1301–1305. doi:10.1038/sj.eye.6701752. ISSN 0950-222X.
- ↑ "How Optical Ultrasonic Cleaners Work".
- ↑ White, Gina. "Caring for Soft Contact Lenses".
- ↑ Ward, Michael. "Soft Contact Lens Care Products".
- ↑ www.feelgoodcontacts.com. "Caring For Contact Lenses - Feel Good Contact Lenses". www.feelgoodcontacts.com. Retrieved 2016-09-05.
- ↑ Wilson-Holt, N; Dart, JK (1989). "Thiomersal keratoconjunctivitis, frequency, clinical spectrum and diagnosis". Eye (London, England). 3 (5): 581–7. doi:10.1038/eye.1989.91. PMID 2630335.
- ↑ Robertson, DM, Petroll, WM, Jester, JV & Cavanagh, HD: Current concepts: contact lens related Pseudomonas keratitis. Cont Lens Anterior Eye, 30: 94–107, 2007.
- ↑ Sharma, S, Kunimoto, D, Rao, N, Garg, P & Rao, G: Trends in antibiotic resistance of corneal pathogens: Part II. An analysis of leading bacterial keratitis isolates, 1999.
- ↑ Verhelst D, Koppen C, Looveren JV, Meheus A, Tassignon M (2005). "Clinical, epidemiological and cost aspects of contact lens related infectious keratitis in Belgium: results of a seven-year retrospective study". Bull Soc Belge Ophtalmol. 297: 7–15.
- ↑ Burd EM, Ogawa GSH, Hyndiuk RA. Bacterial keratitis and conjunctivitis. In: Smolin G, Thoft RA, editors. The Cornea. Scientific Foundations and Clinical Practice. 3rd ed. Boston: Little, Brown, & Co, 1994. p 115–67.
- ↑ Zaidi T, Mowrey-McKee M, Pier GB (2004). "Hypoxia increases corneal cell expression of CFTR leading to increased Pseudomonas aeruginosa binding, internalization, and initiation of inflammation". Invest Ophthalmol Vis Sci. 45: 4066–74. doi:10.1167/iovs.04-0627.
- ↑ Sweeney DF, Keay L, Jalbert I. Clinical performance of silicone hydrogel lenses. In Sweeney DF, ed. Silicone Hydrogels: The Rebirth of Continuous Wear Contact Lenses. Woburn, Ma: Butterworth Heinemann; 2000.
- ↑ Kodjikian L, Casoli-Bergeron E, Malet F, Janin-Manificat H, Freney J, Burillon C, Colin J, Steghens JP (2008). "Bacterial adhesion to conventional hydrogel and new silicone hydrogel contact lens materials". Graefes Arch Clin Exp Ophthalmol. 246: 267–73. doi:10.1007/s00417-007-0703-5.
- ↑ Santos, Lívia; Diana Rodrigues; Madalena Lira; M Elisabete C. D. Real Oliveira; Rosário Oliveira; Eva Yebra-Pimente Vilar; Joana Azeredo (2008). "Bacterial Adhesion to Worn Silicone Hydrogel Contact Lenses". Optometry and Vision Science. 85 (7): 520–525. doi:10.1097/OPX.0b013e31817c92f3. ISSN 1040-5488.
- ↑ Agarwal R.K. (1971). "A legally problematical but clinically interesting contact lens case". The Contact Lens. 3 (3): 13.
- ↑ Yung MS, Boost M, Cho P, Yap M (2007). "Microbial contamination of contact lenses and lens care accessories of soft contact lens wearers (university students) in Hong Kong". Ophthalmic and Physiological Optics. 27 (1): 11–21. doi:10.1111/j.1475-1313.2006.00427.x.
- ↑ Midelfart J.; Midelfart A.; Bevanger L. (1996). "Microbial contamination of contact lens cases among medical students". CLAO J. 22 (1): 21–24.
- ↑ Gray T.B.; Cursons R.T.; Sherwan J.F.; Rose P.R. (1995). "Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases". Br J Ophthalmol. 79: 601–605. doi:10.1136/bjo.79.6.601.
- ↑ Amos CF, George MD (2006). "Clinical and laboratory testing of a silver-impregnated lens case". Cont Lens Anterior Eye. 29: 247–55. doi:10.1016/j.clae.2006.09.007.
- ↑ Mathews SM, Spallholz JE, Grimson MJ, Dubielzig RR, Gray T, Reid TW (2006). "Prevention of bacterial colonization of contact lenses with covalently attached selenium and effects on the rabbit cornea". Cornea. 25: 806–14. doi:10.1097/01.ico.0000224636.57062.90.
- ↑ Santos L; Rodrigues D; Lira M; Oliveira R; Oliveira Real, ME; Vilar EY; Azeredo J (2007). "The effect of octylglucoside and sodium cholate in Staphylococcus epidermidis and Pseudomonas aeruginosa adhesion to soft contact lenses". Optom Vis Sci. 84: 429–34. doi:10.1097/opx.0b013e318058a0cc.
- 1 2 "Contacts Release Anesthesia to Eyes of Post-Surgery Patients". Retrieved 4 April 2013.
Further reading
- Efron, Nathan (2002). Contact Lens Practice. Elsevier Health Sciences. 0-7506-4690-X.
Heitz, Robert (2003, 2005 & 2014) The History of Contact Lenses in: Julius Hirschberg, History of Ophthalmology, vols.11/3a; 11/3b & 11/3c. Wayenborgh Publishing Ostend/Belgium & Piribebuy/Paraguay ISBN 978-90-6299-463-2
External links
| Wikimedia Commons has media related to Contact lens. |
- Contact lens and anterior eye journal
- "Glass Disks Under Eyelids Replace Spectacles" Popular Mechanics Monthly, July 1930, left-bottom pg 31