Duarte galactosemia
Duarte galactosemia (also known as Duarte variant galactosemia, DG, or biochemical variant galactosemia) is an inherited condition associated with diminished ability to metabolize galactose due to a partial deficiency of the enzyme galactose-1-phosphate uridylyltransferase.[1] Duarte galactosemia (DG) is estimated to affect close to one in 4,000 infants born in the United States. DG Is considered by most healthcare professionals to be clinically mild.[1] It differs from classic galactosemia in that patients with Duarte galactosemia have partial GALT deficiency whereas patients with classic galactosemia have complete, or almost complete, GALT deficiency.[2]
DG, and the possible outcomes associated with this condition, are currently not well understood. Due to regional variations in newborn screening (NBS) protocols, some infants with DG are identified by NBS but others are not.[3] In addition, of the infants who are diagnosed, most are clinically healthy as babies and toddlers, resulting in early discharge from follow up.[4] Many healthcare professionals believe that DG does not negatively impact development. However, some reports have indicated that children with DG may be at increased risk for some developmental problems.[5][6]
Symptoms
Infants with DG show an impaired ability to metabolize galactose, a sugar found at high levels in breast milk, milk formula, and most dairy products.[7] Galactose is found at low levels in many fruits, vegetables, and other foods. Galactose is also produced at low levels by the human body. Infants with DG, who consume breast milk or formula containing the milk sugar, lactose, are usually, but not always, asymptomatic. Infants who do show symptoms, such as jaundice, typically recover quickly when switched to a low-lactose diet, such as soy formula.[1]
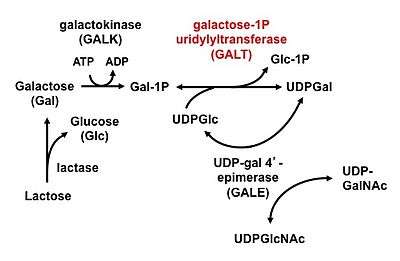
Mechanism
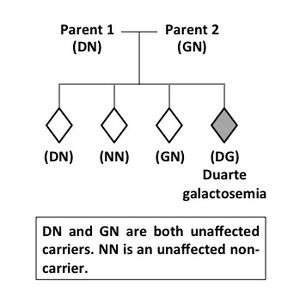
Duarte galactosemia is inherited as a Mendelian autosomal recessive trait. A child with DG carries two different types of GALT alleles, one inherited from each parent. One of these GALT alleles, the G allele, carries a mutation that severely inhibits the function of the encoded GALT enzyme. The other GALT allele, the D or D2 allele, carries mutations that partially compromise the expression and change some biochemical properties of the GALT enzyme. Together, the G and D alleles only produce about 25% of the normal level of GALT enzyme activity found in a person with two normal (N) GALT alleles.[1] Both parents of a child with DG are considered carriers for GALT variant alleles: one carries the G allele and the other carries the D allele. The genotypes of these parents would be written GN and DN, respectively. Without follow-up testing of the parents it is not possible to know which parent contributed which GALT allele to a child with DG. The recurrence risk for DG is 1 in 4, meaning that for each successive child born to parents who already have a child with DG there is a 1 in 4 chance the new baby will also have DG (Figure 2). In rare cases, one parent may actually have DG but not know it, while the other parent is a carrier for a G allele (GN). For these couples, there is a 1 in 4 recurrence risk for DG and also a 1 in 4 risk with each pregnancy that the new baby will have classic galactosemia. In extremely rare cases a GALT mutation may arise de novo, so that only one parent is a carrier; however, only one case of this has ever been reported.[8]
Diagnosis
Infants with DG who drink breast milk or lactose-containing formula may have elevated levels of galactose in their blood, tissues, and urine due to their impaired ability to process the galactose after it has been absorbed.[9] DG can be detected in dried blood spots by newborn screening on the basis of elevated galactose metabolite levels, low GALT enzyme activity, or both. DG can be diagnosed by genetic testing.[1]
Not all NBS tests for galactosemia are designed to detect DG so affected infants born in one location may be detected while those born in another may not.[3] For example, all states in the US screen for classic galactosemia in their NBS panel, but some states have lower GALT enzyme activity cut-off levels than others. NBS in states with a low GALT cut off level still detects classic galactosemia and helps to minimize false positives, but it can also result in "missed" DG diagnoses for those samples with partial GALT enzyme activity that is above the cut-off. In those states, a NBS result for galactosemia designated as "normal" may not be informative about an infant's DG status.
Most infants with DG who are detected by NBS have their diagnosis confirmed in a follow-up evaluation. The differential diagnosis of a positive newborn screen for galactosemia includes: classic galactosemia, clinical variant galactosemia, DG, GALE (epimerase) deficiency, GALK (galactokinase) deficiency, or an initial false positive result.[1] There are also other rare conditions, such as portosystemic venous shunting and hepatic arteriovenous malformations, or Fanconi-Bickel Syndrome (GSDXI) that can lead to elevated blood galactose or urinary galactitol, triggering an initial suspicion of galactosemia.[1][10]
Management
There is no broadly accepted standard of care for infants with DG.[4] Some healthcare providers recommend partial to complete dietary restriction of milk and other high galactose foods for infants or young children with DG; others do not. Because children with DG develop increased tolerance for dietary galactose as they grow, few healthcare providers recommend dietary restriction of lactose or galactose beyond early childhood.
The rationale for NOT restricting dietary galactose exposure of infants and/or young children with DG: Healthcare providers who do not recommend dietary restriction of galactose for infants with DG generally consider DG to be of no clinical significance—meaning most infants and children with DG seem to be doing clinically well. Further, these providers may be opposed to interrupting or reducing breastfeeding when there is no clear evidence it is contraindicated. These providers may argue that the recognized health benefits of breastfeeding outweigh the potential risks of as yet unknown negative effects of continued milk exposure for these infants.[4] For infants with DG who continue to drink milk, some doctors would recommend that blood galactose-1-phosphate (Gal-1P) or urinary galactitol be rechecked by age 12 months to ensure that these metabolite levels are normalizing.[1]
The rationale FOR restricting dietary galactose exposure of infants and/or young children with DG: Healthcare providers who recommend partial or complete dietary restriction of galactose for infants and/or young children with DG generally cite concern about the unknown long-term consequences of abnormally elevated galactose metabolites in a young child's blood and tissues. Infants with DG who continue to drink milk accumulate the same set of abnormal galactose metabolites seen in babies with classic galactosemia – e.g. galactose, Gal-1P, galactonate, and galactitol[9] – but to a lesser extent. While it remains unclear whether any of these metabolites contribute to the long-term developmental complications experienced by so many older children with classic galactosemia, the possibility that they might cause problems serves to motivate some healthcare providers to recommend dietary galactose restriction for infants with DG. Switching an infant with DG from milk or milk formula (high galactose) to soy formula (low galactose) rapidly normalizes their galactose metabolites. This approach is considered potentially preventative rather than responsive to acute symptoms.[4]
If dietary galactose restriction of any kind is followed, healthcare providers may recommend that the child have a galactose challenge to re-evaluate galactose tolerance before the restrictive diet is discontinued. Most infants or young children with DG who are followed by a metabolic specialist are discharged from follow up after a successful galactose challenge.Options for those choosing to restrict dietary galactose in infancy and/or early childhood: Dietary restriction practices for Duarte galactosemia vary widely. In the US, some healthcare providers recommend full dietary restriction of milk and all dairy products for the first 12 months of life, followed by a galactose challenge. Some providers recommend the galactose challenge before 12 months, others after. Some providers who recommend dietary intervention suggest a "compromise approach" if the parent wishes to breastfeed, such that the parent alternates feedings of breast milk and low galactose formula. Finally, some parents choose to continue some form of dietary galactose restriction for their child with DG beyond early childhood.
What is a galactose challenge? The goal of a galactose challenge is to learn whether a child is able to metabolize dietary galactose sufficiently to prevent the abnormal accumulation of galactose metabolites, generally measured as Gal-1P in the blood.[1] For infants with DG who showed elevated galactose metabolites at diagnosis, this test can be used to see if their ability to process galactose has improved enough to discontinue dietary galactose restriction.
To test galactose metabolism, a baseline Gal-1P level is measured while the child is on a galactose-restricted diet. If the level is within the normal range (e.g. <1.0 mg/dL), the parent/guardian is advised to "challenge" the child with dietary galactose—meaning feed the child a diet that includes normal levels of milk for 2–4 weeks. Immediately after that time, another blood sample is collected and analyzed for Gal-1P level. If this second result is still in the normal range, the child is said to have "passed" their galactose challenge, and dietary galactose restrictions are typically relaxed or discontinued. If the second test shows elevated Gal-1P levels, the parent/guardian may be advised to resume galactose restriction for the child, and the "challenge" may be repeated after a few months.[1]
Prognosis
Very little is known about outcomes in DG after early childhood. This is because many infants with DG are born in states where they are not diagnosed by NBS, and of those who are diagnosed, most are discharged from metabolic follow-up as toddlers. Because it is unclear whether DG has any long-term developmental impacts, or if diet modification would prevent or resolve any issues that may result from DG, any developmental or psychosocial problems experienced by a person with DG should be treated symptomatically and the possibility of other causes should be explored.[1] Of note, premature ovarian insufficiency, a common outcome among girls and women with classic galactosemia, has been checked by hormone studies and does not appear to occur at high prevalence among girls with DG.[11]
Prior Research Concerning Developmental Outcomes of Children with DG: Three studies of developmental outcomes of children with DG have been published.
- The first[12] looked at biochemical markers and developmental outcomes in a group of 28 toddlers and young children with DG, some of whom had drunk milk through infancy and some of whom had drunk soy formula. The authors found that galactose metabolites were significantly elevated in the infants drinking milk over those drinking soy.[9] However, all of the children scored within normal limits on standardized tests of child development.
- A second study of developmental outcomes in DG[5] looked at 3 to 10 year olds living in a large metropolitan area and asked whether children diagnosed as newborns with DG in this group were more likely than their unaffected peers to receive special educational services later in childhood. The answer was yes. Specifically, children with DG in this group were significantly more likely than other children to receive a diagnosis of, or special educational services for, a speech/language disorder.
- The final study reported that addressed developmental outcomes in DG was a pilot study involving direct assessments of 15 children, all ages 6–11 years old; 15 had DG and 5 did not.[6] Children in the DG group showed slower auditory processing than did the control group. The DG group also showed some slight differences in auditory memory, receptive language/ listening skills, social-emotional functioning, and balance and fine motor coordination.
Combined, these studies suggest that school age children with DG might be at increased risk for specific developmental difficulties compared with controls. All of the relevant studies were limited, however, leaving the question of whether children with DG are truly at increased risk for developmental difficulties unresolved. Current reports also leave open the question of whether dietary exposure to milk in infancy associates with developmental outcomes in DG. More research is needed to answer these questions.[1]
Epidemiology
The prevalence of DG in the United States (US) can only be estimated because there is no true population surveillance for this condition. Differences in NBS methods result in very different detection rates for DG in different states. For example, in some US states, DG is detected by NBS in up to 1 in 3500 infants screened, while in other states it is essentially not detected.[3] DG prevalence in the US Caucasian population is estimated to be approximately 1 in 4,000,[12] which is nearly 10 times the prevalence of classic galactosemia.[1][2]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Fridovich-Keil, J., et al., Duarte Variant Galactosemia, in GeneReviews, R. Pagon, et al., Editors. 2014, University of Washington, Seattle. Review. PMID 25473725
- 1 2 Berry, G., Classic Galactosemia and Clinical Variant Galactosemia, in GeneReviews, R. Pagon, et al., Editors. 2014, University of Washington, Seattle. Review.
- 1 2 3 Pyhtila, B.M., et al., Newborn screening for galactosemia in the United States: looking back, looking around, and looking ahead. JIMD Rep, 2015. 15: p. 79-93. Review. PMID 24718839
- 1 2 3 4 Fernhoff, P.M., Duarte galactosemia: how sweet is it? Clin Chem, 2010. 56(7): p. 1045-6.
- 1 2 Powell KK, Van Naarden Braun K, Singh RH, Shapira SK, Olney RS, Yeargin-Allsopp M. Long-term speech and language developmental issues among children with Duarte galactosemia. Genet Med. 2009 Dec;11(12):874-9. doi: 10.1097/GIM.0b013e3181c0c38d. PMID 19904210
- 1 2 Lynch ME, Potter NL, Coles CD, Fridovich-Keil JL. Developmental Outcomes of School-Age Children with Duarte Galactosemia: A Pilot Study. JIMD Rep. 2015;19:75-84. doi: 10.1007/8904_2014_370. Epub 2015 Feb 15.PMID 25681083
- ↑ Van Calcar SC, Bernstein LE, Rohr FJ, Scaman CH, Yannicelli S, Berry GT. A re-evaluation of life-long severe galactose restriction for the nutrition management of classic galactosemia. Mol Genet Metab. 2014 Jul;112(3):191-7. doi: 10.1016/j.ymgme.2014.04.004. Epub 2014 May 2. Review. PMID 24857409
- ↑ Tran, T.T., et al., A De Novo Variant in Galactose-1-P Uridylyltransferase (GALT) Leading to Classic Galactosemia. JIMD Rep, 2015. 19: p. 1-6
- 1 2 3 Ficicioglu, C., et al., Monitoring of biochemical status in children with Duarte galactosemia: utility of galactose, galactitol, galactonate, and galactose 1-phosphate. Clin Chem, 2010. 56(7): p. 1177-82. PMID 20489133
- ↑ Nishimura Y, Tajima G, Dwi Bahagia A, Sakamoto A, Ono H, Sakura N, Naito K, Hamakawa M, Yoshii C, Kubota M, Kobayashi K, Saheki T. Differential diagnosis of neonatal mild hypergalactosaemia detected by mass screening: clinical significance of portal vein imaging. J Inherit Metab Dis. 2004;27(1):11-8. PMID 14970742
- ↑ Badik, J.R., et al., Ovarian function in Duarte galactosemia. Fertil Steril, 2011. 96(2): p. 469-473 e1. PMID 21719007
- 1 2 Ficicioglu, C., et al., Duarte (DG) galactosemia: a pilot study of biochemical and neurodevelopmental assessment in children detected by newborn screening. Mol Genet Metab, 2008. 95(4): p. 206-12.
Further reading
- Fernandes, John; Saudubray, Jean-Marie; Berghe, Georges van den (2013-03-14). Inborn Metabolic Diseases: Diagnosis and Treatment. Springer Science & Business Media. ISBN 9783662031476.
- Leonard, Debra G. B. (2007-11-25). Molecular Pathology in Clinical Practice. Springer Science & Business Media. ISBN 9780387332277.
External links
- Duarte Galactosemia Website
- The Galactosemia Foundation website
- Duarte Variant Galactosemia article in GeneReviews
- Duarte Galactosemia Study summary on PCORI.org