Miscarriage
| Miscarriage | |
|---|---|
 | |
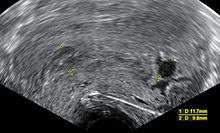
| An ultrasound showing an empty sac, a gestational sac containing a yolk sac but no embryo. This is a type of miscarriage. | |
| Classification and external resources | |
| Specialty | Obstetrics and gynecology |
| ICD-10 | O03 |
| ICD-9-CM | 634 |
| OMIM | 614389 |
| DiseasesDB | 29 |
| MedlinePlus | 001488 |
| eMedicine | topic list |
| Patient UK | Miscarriage |
| MeSH | D000022 |
Miscarriage, also known as spontaneous abortion and pregnancy loss, is the natural death of an embryo or fetus before it is able to survive independently.[1][2] Some use the cutoff of 20 weeks of gestation after which fetal death is known as a stillbirth.[2] The most common symptoms of a miscarriage is vaginal bleeding with or without pain.[1] Sadness, anxiety, and guilt may occur.[3] Tissue or clot like material may also come out of the vagina.[4]
Risk factors for miscarriage include an older parent, previous miscarriage, exposure to tobacco smoke, obesity, diabetes, and drug or alcohol use, among others.[5][6] In those under the age of 35 the risk is about 10% while it is about 45% in those over the age of 40.[1] Risk begins to increase around the age of 30.[5] About 80% of miscarriages occur in the first 12 weeks of pregnancy (the first trimester). The underlying cause in about half of cases involves chromosomal abnormalities. Other conditions that can produce similar symptoms include an ectopic pregnancy and implantation bleeding.[1] Diagnosis of a miscarriage may involve checking to see if the cervix is open or closed, testing blood levels of human chorionic gonadotropin (hCG), and an ultrasound.[7]
Prevention is occasionally possible with good prenatal care. Avoiding drugs and alcohol, infectious diseases, and radiation may prevent miscarriage.[8] No specific treatment is usually needed during the first 7 to 14 days.[6][9] Most miscarriage will complete without additional interventions.[6] Occasionally the medication misoprostol or a procedure such as vacuum aspiration is required to remove the failed pregnancy.[9][10] Women who are rhesus negative may require Rho(D) immune globulin.[6] Pain medication may be beneficial.[9] Emotional support may help with negative emotions.[9]
Miscarriage is the most common complication of early pregnancy.[11] Among females who know they are pregnant, the miscarriage rate is roughly 10% to 20% while rates among all fertilisation is around 30% to 50%.[1][5] About 5% of females have two miscarriages in a row.[12] Some recommend not using the term "abortion" in discussions with those experiencing a miscarriage in an effort to decrease distress.[13]
Signs and symptoms
The most common symptom of a miscarriage is vaginal bleeding.[14] This can vary from light spotting or brownish discharge to heavy bleeding and bright red blood. The bleeding may come and go over several days. However, light vaginal bleeding is relatively common during the first trimester of pregnancy (the first 12 weeks) and does not necessarily indicate a miscarriage.
Bleeding during pregnancy may be referred to as a threatened miscarriage. Of those who seek clinical treatment for bleeding during pregnancy, about half will miscarry.[15] Symptoms other than bleeding are not statistically related to miscarriage.[14]
Miscarriage may be detected during an ultrasound exam, or through serial human chorionic gonadotropin (HCG) testing. Those who became pregnant using assisted reproductive technology methods, and those with a history of miscarriage may be monitored closely, and may be diagnosed with miscarriage sooner.
Causes
Miscarriage may occur for many reasons, not all of which can be identified. Some of these causes include genetic, uterine, or hormonal abnormalities, reproductive tract infections, and tissue rejection. Miscarriage caused by invasive prenatal diagnosis (chorionic villus sampling (CVS) and amniocentesis) is rare (about 1%).[16][17]
First trimester
Most clinically apparent miscarriages (two-thirds to three-quarters in various studies) occur during the first trimester.[18][19][20] About 30% to 40% of all fertilized eggs miscarry, often before the pregnancy is known.[1] The embryo typically dies before the pregnancy is expelled; bleeding into the decidua basalis and tissue necrosis causes uterine contractions to expel the pregnancy.[20]
A chemical pregnancy refers to a pregnancy that was detected by testing but ends in miscarriage before or around the time of the next expected period.[21]
Chromosomal abnormalities are found in more than half of embryos miscarried in the first 13 weeks;[22] half of embryonic miscarriages (25% of all miscarriages) have an aneuploidy (abnormal number of chromosomes). Common aneuploidies found in miscarriages include autosomal trisomy (22-32%), monosomy X (5-20%), triploidy (6-8%), tetraploidy (2-4%), or other structural chromosomal abnormalities (2%).[20] Chromosomal problems due to a parent's genes may also cause miscarriage. This is more likely to have been the cause in the case of repeated miscarriages, or if one of the parents has a child or other relatives with birth defects.[23] Genetic problems are more likely to occur with older parents; this may account for the higher rates observed in older people.[24]
Progesterone deficiency may be another cause. Those diagnosed with low progesterone levels in the second half of their menstrual cycle (luteal phase) may be prescribed progesterone supplements, to be taken for the first trimester of pregnancy.[23] There is no evidence that progesterone given in the first trimester reduces the risk of miscarriage, and luteal phase progesterone deficiency may or may not be a contributing factor to miscarriage.[25][26]
Second trimester
Second trimester losses may be due to uterine malformation, growths in the uterus (fibroids), or cervical problems.[23] These conditions also may contribute to premature birth.[18]
One study found that 19% of second trimester losses were caused by problems with the umbilical cord. Problems with the placenta also may account for a significant number of later-term miscarriages.[27]
Unlike in first-trimester miscarriages, second-trimester miscarriages are less likely to be cause by a genetic abnormality; chromosomal aberrations are found in a third of cases.[20]
Induced miscarriage
If a pregnant person does not want to give birth, doctors may induce a therapeutic abortion.[28] In places where induced abortion is illegal or carries heavy social stigma, those who wish to end the pregnancy may attempt self-induced abortion, sometimes called "induced miscarriage" or "self-induced miscarriage".
Risk factors
Multiple pregnancy
Pregnancies with more than one fetus are at increased risk for miscarriage. This risk increases with the number of fetuses in the pregnancy.[23]
Intercurrent diseases
Several intercurrent diseases in pregnancy can potentially increase the risk of miscarriage, including diabetes, polycystic ovarian syndrome (PCOS), hypothyroidism, certain infectious diseases, and autoimmune diseases. The risk of miscarriage is increased in those with poorly controlled insulin-dependent diabetes mellitus, but there is no significant increase in risk with well-controlled diabetes.[29] PCOS may increase the risk of miscarriage, but this is disputed.[30] Two studies suggested treatment with the drug metformin significantly lowers the rate of miscarriage in women with PCOS,[31][32] but the quality of these studies has been questioned.[33] A 2006 review of metformin treatment in pregnancy found insufficient evidence of safety, and did not recommend routine treatment with the drug.[34] In 2007 the Royal College of Obstetricians and Gynaecologists also recommended against use of the drug to prevent miscarriage.[33]
Severe cases of hypothyroidism increase the risk of miscarriage. The effect of milder cases of hypothyroidism on miscarriage rates has not been established. The presence of certain immune conditions such as autoimmune diseases is associated with a greatly increased risk.[23] The presence of anti-thyroid autoantibodies is associated with an increased risk with an odds ratio of 3.73 and 95% confidence interval 1.8–7.6.[35] Some research suggests autoimmunity in general as a possible cause of recurrent or late-term miscarriages. Autoimmune disease occurs when the body's own immune system acts against itself. Therefore, in the case of an autoimmune-induced miscarriages the woman's body attacks the growing fetus or prevents normal pregnancy progression.[36][37] Further research also has suggested that autoimmune disease may cause genetic abnormalities in embryos which in turn may lead to miscarriage.[38] As an example, Celiac disease increases the risk of miscarriage by an odds ratio of approximately 1.4.[39]
Diseases transmitted vertically (through the placenta to the fetus), such as rubella or chlamydia, can increase the risk of miscarriage.[23]Mycoplasma genitalium infection is associated with increased risk of preterm birth and miscarriage.[40]
Smoking
Tobacco (cigarette) smokers have an increased risk of miscarriage.[41] There is an increased risk regardless of which parent smokes, though the risk is higher when the gestational parent smokes. [42]
Age
The age of the pregnant person is a significant risk factor. Miscarriage rates increase steadily with age, with more substantial increases after age 35.[43]
Morning sickness
Nausea and vomiting of pregnancy (NVP, or morning sickness) are associated with a decreased risk. Several proximate causes have been proposed for this relationship, but none are widely agreed upon.[44] NVP is generally interpreted as a defense mechanism which discourages the mother's ingestion of foods that are harmful to the fetus; according to this model, a lower frequency of miscarriage would be an expected consequence of the different food choices made by a women experiencing NVP.
Exercise
A study of more than 92,000 pregnant people found that most types of exercise (with the exception of swimming) correlated with a higher risk of miscarrying prior to 18 weeks. Increasing time spent on exercise was associated with a greater risk: an approximately 10% increased risk was seen with up to 1.5 hours per week of exercise, and a 200% increased risk was seen with more than 7 hours per week of exercise. However, the study found none of these risks to be statistically significant. High-impact exercise was especially associated with the increased risk. No relationship was found between exercise rates after the 18th week of pregnancy. The majority of miscarriages had already occurred at the time pregnant people were recruited for the study, and no information on nausea during pregnancy or exercise habits prior to pregnancy was collected.[45]
Caffeine
Caffeine consumption also has been correlated to miscarriage rates, at least at higher levels of intake. However, such higher rates have been found to be statistically significant only in certain circumstances. A 2007 study of more than 1,000 pregnant people found that those who reported consuming 200 mg or more of caffeine per day experienced a 25% rate of miscarriage, compared to 13% among women who reported no caffeine consumption. 200 mg of caffeine is present in 10 oz (300 mL) of coffee or 25 oz (740 mL) of tea. This study controlled for pregnancy-associated nausea and vomiting (NVP or morning sickness): the increased rate for heavy caffeine users was seen regardless of how NVP affected the women. About half of the miscarriages had already occurred at the time women were recruited for the study.[46] A second 2007 study of approximately 2,400 pregnant women found that caffeine intake up to 200 mg per day was not associated with increased rates (the study did not include women who drank more than 200 mg per day past early pregnancy).[47] A prospective cohort study in 2009 found that light or moderate caffeine consumption (up to 300 mg per day) had no effect on pregnancy or miscarriage rates.[48]
Antidepressant medication
There is no significant association between antidepressant medication exposure and spontaneous abortion.[49] The risk of miscarriage is likely not to be modified by discontinuing SSRI prior to pregnancy.[50] Some available data suggest that there is a small increased risk of miscarriage for women taking any antidepressant,[51][52] though this risk becomes less statistically significant when excluding studies of poor quality.[49][53]
Other

Sexual intercourse during the first trimester has often been assumed by doctors to be a cause of miscarriage. However the association has never been proved or disproved.[54]
Cocaine use increases the rate of miscarriage.[41] Physical trauma, exposure to environmental toxins, and use of an intrauterine device at the time of fertilization have also been linked to increased risk.[55]
Loop electrosurgical excision procedure (LEEP) is one of the most commonly used approaches to treat high grade cervical dysplasia. A cohort study came to the result that those with a time interval from LEEP to pregnancy of less than 12 months compared with 12 months or more were at significantly increased risk for spontaneous abortion, with risk of spontaneous abortion of 18% compared with 4.6%, respectively.[56] On the other hand, no increased risk was identified for preterm birth after LEEP.[56]
Diagnosis
Bleeding during early pregnancy is the most common symptom of both impending miscarriage and of ectopic pregnancy. Pain does not strongly correlate with the former, but is a common symptom of ectopic pregnancy.[14] Typically, in the case of blood loss, pain, or both, transvaginal ultrasound is performed. If a viable intrauterine pregnancy is not found with ultrasound, serial βHCG tests should be performed to rule out ectopic pregnancy, which is a life-threatening situation.[57][58]
A miscarriage may be confirmed via obstetric ultrasound and by the examination of the passed tissue. When looking for microscopic pathologic symptoms, one looks for the products of conception. Microscopically, these include villi, trophoblast, fetal parts, and background gestational changes in the endometrium. When chromosomal abnormalities are found in more than one miscarriage, genetic testing of both parents may be done.[59]
Ultrasound criteria
A review article in The New England Journal of Medicine based on a consensus meeting of the Society of Radiologists in Ultrasound in America (SRU) has suggested that miscarriage should be diagnosed only if any of the following criteria are met upon ultrasonography visualization:[60]
- Crown-rump length of at least 7 mm and no heartbeat.
- Mean gestational sac diameter of at least 25 mm and no embryo.
- Absence of embryo with heartbeat at least 2 weeks after an ultrasound scan that showed a gestational sac without a yolk sac.
- Absence of embryo with heartbeat at least 11 days after an ultrasound scan that showed a gestational sac with a yolk sac.
In addition, signs upon ultrasonography that are suggested to be suspicious for miscarriage, but not diagnostic of it, include:[60]
- Crown–rump length of less than 7 mm and no heartbeat.
- Mean gestational sac diameter of 16–24 mm and no embryo.
- Absence of embryo with heartbeat 7–13 days after an ultrasound scan that showed a gestational sac without a yolk sac.
- Absence of embryo with heartbeat 7–10 days after a scan that showed a gestational sac with a yolk sac.
- Absence of embryo at least 6 weeks after last menstrual period.
- Amniotic sac seen adjacent to yolk sac, and with no visible embryo.
- Yolk sac of more than 7 mm.
- Small gestational sac compared to embryo size (less than 5 mm difference between mean sac diameter and crown–rump length).
Classification
The clinical presentation of a "threatened miscarriage" describes any bleeding during pregnancy, prior to viability, that has yet to be assessed further. At investigation it may be found that the fetus remains viable and the pregnancy continues without further problems.
An anembryonic pregnancy (also called an "empty sac" or "blighted ovum") is a condition where the gestational sac develops normally, while the embryonic part of the pregnancy is either absent or stops growing very early. This accounts for approximately half of miscarriages. All other miscarriages are classified as embryonic miscarriages, meaning that there is an embryo present in the gestational sac. Half of embryonic miscarriages have aneuploidy (an abnormal number of chromosomes).[20]
An inevitable miscarriage occurs when the cervix has already dilated,[61] but the fetus has yet to be expelled. This usually will progress to a complete miscarriage. The fetus may or may not have cardiac activity.

A complete miscarriage is when all products of conception have been expelled; these may include the trophoblast, chorionic villi, gestational sac, yolk sac, and fetal pole (embryo); or later in pregnancy the fetus, umbilical cord, placenta, amniotic fluid, and amniotic membrane. The presence of a pregnancy test that is still positive as well as an empty uterus upon transvaginal ultrasonography does, however, fulfill the definition of pregnancy of unknown location. Therefore, there may be a need for e.g. follow-up pregnancy tests to ensure that there is no remaining pregnancy, including an ectopic pregnancy.
An incomplete miscarriage occurs when some products of conception have been passed, but some remains inside the uterus.[62] However, an increased distance between the uterine walls on transvaginal ultrasonography may also simply be an increased endometrial thickness and/or a polyp. The use of a Doppler ultrasound may be better in confirming the presence of significant retained products of conception in the uterine cavity.[63] In cases of uncertainty, ectopic pregnancy must be excluded using techniques like serial beta-hCG measurements.[63]

A missed miscarriage is when the embryo or fetus has died, but a miscarriage has not yet occurred. It is also referred to as delayed miscarriage or silent miscarriage.[64][65]
A septic miscarriage occurs when the tissue from a missed or incomplete miscarriage becomes infected, which carries the risk of spreading infection (septicaemia) and can be fatal.[20]
Recurrent pregnancy loss (RPL) or recurrent miscarriage is the occurrence of multiple consecutive miscarriages; the exact number used to diagnose recurrent miscarriage varies.[20] If the proportion of pregnancies ending in miscarriage is 15% and assuming that miscarriages are independent events,[66] then the probability of two consecutive miscarriages is 2.25% and the probability of three consecutive miscarriages is 0.34%. The occurrence of recurrent pregnancy loss is 1%.[66] A large majority (85%) of those who have had two miscarriages will conceive and carry normally afterward.
The physical symptoms of a miscarriage vary according to the length of pregnancy, though most miscarriages cause pain or cramping. The size of blood clots and pregnancy tissue that are passed become larger with longer gestations. After 13 weeks' gestation, there is a higher risk of placenta retention.[67]
Prevention
Prevention of miscarriage centers on decreasing risk factors.[8] This may include good prenatal care, avoiding drugs and alcohol, preventing infectious diseases, and avoiding radiation.[8] Identifying the cause of the miscarriage may help prevent future pregnancy loss, especially in cases of recurrent miscarriage. Often there is little a person can do to prevent a miscarriage.[8] Vitamin supplementation has not been found to be effective to prevent miscarriage.[68]
Management
It is estimated about half of early miscarriages will complete on their own; in other cases, medication treatment or aspiration of the products of conception can be used to remove remaining tissue.[69] Emergency care may become necessary in cases of very heavy bleeding or fever.
While bed rest has been advocated to prevent miscarriage, and in one study possibly helped when small subchorionic hematoma had been found on ultrasound scans,[70] the prevailing opinion is that this is of no proven benefit.[71]
There is not good evidence that the use of Rho(D) immune globulin after a spontaneous miscarriage is needed and a Cochrane review recommends that local practices be followed.[72] In the UK, Rho(D) immune globulin is recommended in Rh-negative people after 12 weeks gestational age and before 12 weeks gestational age in those who need surgery or medication to complete the miscarriage.[73]
Methods
No treatment is necessary for a diagnosis of complete miscarriage (so long as ectopic pregnancy is ruled out). In cases of an incomplete miscarriage, empty sac, or missed abortion there are three treatment options: watchful waiting, medical management, and surgical treatment. With no treatment (watchful waiting), most miscarriages (65–80%) will pass naturally within two to six weeks.[74] This treatment avoids the possible side effects and complications of medications and surgery,[75] but increases the risk of mild bleeding, need for unplanned surgical treatment, and incomplete miscarriage. Medical treatment usually consists of using misoprostol (a prostaglandin) to contract the uterus, pushing the products of conception out of the cervix. This works within a few days in 95% of cases.[74] Surgical treatment for a miscarriage can be used to complete the removal of pregnancy tissue, and shortens the duration and severity of bleeding and pain. Vacuum aspiration or sharp curettage can be used, though vacuum aspiration is lower-risk and more common.[74]
Delayed and incomplete miscarriage
In delayed or incomplete miscarriage, management depends on the amount of material left in the uterus as measured with ultrasonography. Treatment can include surgical removal of the retained pregnancy with vacuum aspiration or misoprostol.[76]
Prognosis
Psychological

Some people struggle emotionally following a miscarriage.[3] A questionnaire for those who had experienced a miscarriage showed that more than half (55%) presented with significant psychological distress immediately, while 25% did at 3 months; 18% showed psychological symptoms at 6 months, and 11% at 1 year after miscarriage.[77]
Besides the feeling of loss, a lack of understanding by others can be especially detrimental. People who have not experienced a miscarriage themselves may find it difficult to empathize, which can lead to unrealistic expectations of recovery. The pregnancy and the miscarriage may cease to be mentioned in conversations, often because the subject is too painful, causing feelings of isolation. Inappropriate or insensitive responses from medical professionals can add to the distress and trauma experienced, so in some cases attempts have been made to draw up a standard code of practice.[78]
Interaction with pregnant women and newborn children may understandably be painful for those who have experienced miscarriage. Sometimes this makes interaction with friends, acquaintances, and family very difficult.[79] People who have lost a desired pregnancy may find psychological comfort in memorializing their loss.[80]
Later cardiovascular disease
There is a significant association between miscarriage and later development of coronary artery disease, but not of cerebrovascular disease.[81] The association does not imply causation, but may be a result of an underlying factor that increases the risk of both.
Epidemiology
Among those who know they are pregnant, the miscarriage rate is roughly 10% to 20%, while rates among all fertilized zygotes is around 30% to 50%.[1][5][20]
Determining the precise rate is not possible as a large number of miscarriages occur before pregnancies become established and before the person is aware they are pregnant.[82] In addition, those with bleeding in early pregnancy may seek medical care more often than those not experiencing bleeding.[82] Some studies have attempted to account for this by recruiting people who are planning pregnancies and testing for very early pregnancy, although these would also not be representative of the wider population.[82] A systematic review found that the cumulative risk of miscarriage between 5 and 20 weeks of gestation varied from 11% to 22% in studies assessing miscarriage rates.[82] Up to the 13th week of pregnancy, the risk of miscarriage each week was around 2%, dropping to 1% in week 14 and reducing slowly between 14 and 20 weeks.[82]
The prevalence of miscarriage increases with the age of both parents.[82][83][84][85] In a Danish register-based study where the prevalence of miscarriage was 11%, the prevalence rose from 9% at 22 years of age to 84% by 48 years of age.[83] Another study found that when either parent was over the age of 40, the rate of known miscarriages doubled.[20]
Terminology
While miscarriage is a term for early pregnancy loss, it is also frequently known in medical literature as "spontaneous abortion".[86] Those fetuses born before 24 weeks of gestation rarely survive.[87] However, the designation "fetal death" applies variably in different countries and contexts, sometimes incorporating weight, and gestational age from 16 weeks in Norway, 20 weeks in the US and Australia, 24 weeks in the UK to 26 weeks in Italy and Spain.[87][88][89] A fetus that died before birth after this gestational age may be referred to as a stillbirth.[87] Under UK law, all stillbirths should be registered,[90] although this does not apply to miscarriages.
The medical terminology applied to experiences during early pregnancy has changed over time.[91] Before the 1980s, health professionals used the phrase "spontaneous abortion" for a miscarriage and "induced abortion" for a termination of the pregnancy.[91][92] In places where induced abortion is illegal or carries heavy social stigma, suspicion may surround miscarriage, complicating an already sensitive language issue.[93] Research suggests that some dislike the term spontaneous abortion for miscarriage, some are indifferent and some prefer it.[94] These preferences may reflect cultural differences.[94]
In the late 1980s and 1990s, doctors became more conscious of their language in relation to early pregnancy loss. Some medical authors advocated change to use of "miscarriage" instead of "spontaneous abortion" because they argued this would more respectful and help ease a distressing experience.[95][96][97] The change was being recommended by some by the profession in Britain in the late 1990s.[98] In 2005 the European Society for Human Reproduction and Embryology (ESHRE) published a paper aiming to facilitate a revision of nomenclature used to describe early pregnancy events.[64]
Historical analysis of the medical terminology applied to early pregnancy loss in Britain has shown that the use of "miscarriage" (instead of "spontaneous abortion") by doctors only occurred after changes in legislation (in the 1960s) and developments in ultrasound technology (in the early 1980s) allowed them to identify miscarriages.[91] in countries where pregnancy termination remains illegal doctors may still not distinguish between "spontaneous" and "induced" abortions in clinical practice.
Other animals
Miscarriage occurs in all animals that experience pregnancy, though in such contexts it is more commonly referred to as a "spontaneous abortion" (the two terms are synonymous). There are a variety of known risk factors in non-human animals. For example, in sheep, miscarriage may be caused by crowding through doors, or being chased by dogs.[99] In cows, spontaneous abortion may be caused by contagious disease, such as brucellosis or Campylobacter, but often can be controlled by vaccination.[100] Other diseases are also known to make animals susceptible to miscarriage. Spontaneous abortion occurs in pregnant prairie voles when their mate is removed and they are exposed to a new male,[101] an example of the Bruce effect, although this effect is seen less in wild populations than in the laboratory.[102] Female mice who had spontaneous abortions showed a sharp rise in the amount of time spent with unfamiliar males preceding the abortion than those who did not.[103]
See also
References
- 1 2 3 4 5 6 7 The Johns Hopkins Manual of Gynecology and Obstetrics (4 ed.). Lippincott Williams & Wilkins. 2012. pp. 438–439. ISBN 9781451148015.
- 1 2 "What is pregnancy loss/miscarriage?". http://www.nichd.nih.gov/. 2013-07-15. Retrieved 14 March 2015. External link in
|website=(help) - 1 2 Robinson, GE (January 2014). "Pregnancy loss.". Best practice & research. Clinical obstetrics & gynaecology. 28 (1): 169–78. doi:10.1016/j.bpobgyn.2013.08.012. PMID 24047642.
- ↑ "What are the symptoms of pregnancy loss/miscarriage?". http://www.nichd.nih.gov/. 2013-07-15. Retrieved 14 March 2015. External link in
|website=(help) - 1 2 3 4 "How many people are affected by or at risk for pregnancy loss or miscarriage?". http://www.nichd.nih.gov. 2013-07-15. Retrieved 14 March 2015. External link in
|website=(help) - 1 2 3 4 Oliver, A; Overton, C (May 2014). "Diagnosis and management of miscarriage.". The Practitioner. 258 (1771): 25–8, 3. PMID 25055407.
- ↑ "How do health care providers diagnose pregnancy loss or miscarriage?". http://www.nichd.nih.gov/. 2013-07-15. Retrieved 14 March 2015. External link in
|website=(help) - 1 2 3 4 "Is there a cure for pregnancy loss/miscarriage?". http://www.nichd.nih.gov/. 2013-10-21. Retrieved 14 March 2015. External link in
|website=(help) - 1 2 3 4 "What are the treatments for pregnancy loss/miscarriage?". http://www.nichd.nih.gov. 2013-07-15. Retrieved 14 March 2015. External link in
|website=(help) - ↑ Tunçalp, O; Gülmezoglu, AM; Souza, JP (8 September 2010). "Surgical procedures for evacuating incomplete miscarriage.". The Cochrane database of systematic reviews (9): CD001993. doi:10.1002/14651858.CD001993.pub2. PMID 20824830.
- ↑ National Coordinating Centre for Women's and Children's Health (UK) (December 2012). "Ectopic Pregnancy and Miscarriage: Diagnosis and Initial Management in Early Pregnancy of Ectopic Pregnancy and Miscarriage". NICE Clinical Guidelines, No. 154. Royal College of Obstetricians and Gynaecologists. Retrieved 4 July 2013.
- ↑ Garrido-Gimenez, C; Alijotas-Reig, J (March 2015). "Recurrent miscarriage: causes, evaluation and management.". Postgraduate Medical Journal. 91 (1073): 151–162. doi:10.1136/postgradmedj-2014-132672. PMID 25681385.
- ↑ Greaves, Ian; Porter, Keith; Hodgetts, Tim J.; Woollard, Malcolm (2005). Emergency Care: A Textbook for Paramedics. London: Elsevier Health Sciences. p. 506. ISBN 0-7020-2586-0.
- 1 2 3 Gracia CR, Sammel MD, Chittams J, Hummel AC, Shaunik A, Barnhart KT (2005). "Risk Factors for Spontaneous Abortion in Early Symptomatic First-Trimester Pregnancies". Obstetrics & Gynecology. 106 (5, Part 1): 993–9. doi:10.1097/01.AOG.0000183604.09922.e0. PMID 16260517.
- ↑ Everett C (1997). "Incidence and outcome of bleeding before the 20th week of pregnancy: Prospective study from general practice". BMJ. 315 (7099): 32–4. doi:10.1136/bmj.315.7099.32. PMC 2127042
 . PMID 9233324.
. PMID 9233324. - ↑ Tabor A, Alfirevic Z (2010). "Update on procedure-related risks for prenatal diagnosis techniques.". Fetal diagnosis and therapy. 27 (1): 1–7. doi:10.1159/000271995. PMID 20051662.
- ↑ Agarwal K, Alfirevic Z (August 2012). "Pregnancy loss after chorionic villus sampling and genetic amniocentesis in twin pregnancies: a systematic review.". Ultrasound in Obstetrics & Gynecology. 40 (2): 128–34. doi:10.1002/uog.10152. PMID 22125091.
- 1 2 Rosenthal, M. Sara (1999). "The Second Trimester". The Gynecological Sourcebook. WebMD. Retrieved December 18, 2006.
- ↑ Francis O (1959). "An analysis of 1150 cases of abortions from the Government R.S.R.M. Lying-in Hospital, Madras". Journal of obstetrics and gynaecology of India. 10 (1): 62–70. PMID 12336441.
- 1 2 3 4 5 6 7 8 9 Cunningham, F, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, Casey BM, Sheffield JS (2013). "Abortion". Williams Obstetrics. McGraw-Hill.
- ↑ Condous, edited by Tom Bourne, George (2006). Handbook of early pregnancy care. London: Informa Healthcare. pp. 28–29. ISBN 9780203016213.
- ↑ Kajii T, Ferrier A, Niikawa N, Takahara H, Ohama K, Avirachan S (1980). "Anatomic and chromosomal anomalies in 639 spontaneous abortuses". Human Genetics. 55 (1): 87–98. doi:10.1007/BF00329132. PMID 7450760.
- 1 2 3 4 5 6 "Miscarriage: Causes of Miscarriage". HealthCentral.com. Retrieved July 26, 2012.taken word-for-word from pp. 347–9 of: "What To Do When Miscarriage Strikes". The PDR Family Guide to Women's Health and Prescription Drugs. Montvale, NJ: Medical Economics. 1994. pp. 345–50. ISBN 1-56363-086-9.
- ↑ "Pregnancy Over Age 30". MUSC Children's Hospital. Archived from the original on November 13, 2006. Retrieved December 18, 2006.
- ↑ Wahabi HA, Fayed AA, Esmaeil SA, Al Zeidan RA (2011). Wahabi, Hayfaa A, ed. "Progestogen for treating threatened miscarriage". Cochrane Database of Systematic Reviews (12): CD005943. doi:10.1002/14651858.CD005943.pub4. PMID 22161393.
- ↑ Bukulmez O, Arici A (2004). "Luteal phase defect: Myth or reality". Obstetrics and Gynecology Clinics of North America. 31 (4): 727–44, ix. doi:10.1016/j.ogc.2004.08.007. PMID 15550332.
- ↑ Peng HQ, Levitin-Smith M, Rochelson B, Kahn E (2006). "Umbilical Cord Stricture and Overcoiling Are Common Causes of Fetal Demise". Pediatric and Developmental Pathology. 9 (1): 14–9. doi:10.2350/05-05-0051.1. PMID 16808633.
- ↑ Borgatta, L (December 2014). "Labor Induction Termination of Pregnancy". Global Library of Women's Medicine. GLOWM.10444. doi:10.3843/GLOWM.10444. Retrieved 25 September 2015.
- ↑ Mills JL, Simpson JL, Driscoll SG, Jovanovic-Peterson L, Van Allen M, Aarons JH, Metzger B, Bieber FR, Knopp RH, Holmes LB (1988). "Incidence of Spontaneous Abortion among Normal Women and Insulin-Dependent Diabetic Women Whose Pregnancies Were Identified within 21 Days of Conception". New England Journal of Medicine. 319 (25): 1617–23. doi:10.1056/NEJM198812223192501. PMID 3200277.
- ↑ Boomsma CM, Fauser BC, Macklon NS (January 2008). "Pregnancy complications in women with polycystic ovary syndrome.". Seminars in reproductive medicine. 26 (1): 72–84. doi:10.1055/s-2007-992927. PMID 18181085.
- ↑ Jakubowicz DJ, Iuorno MJ, Jakubowicz S, Roberts KA, Nestler JE (2002). "Effects of Metformin on Early Pregnancy Loss in the Polycystic Ovary Syndrome". Journal of Clinical Endocrinology & Metabolism. 87 (2): 524–9. doi:10.1210/jc.87.2.524. PMID 11836280.
- ↑ Khattab S, Mohsen IA, Foutouh IA, Ramadan A, Moaz M, Al-Inany H (2006). "Metformin reduces abortion in pregnant women with polycystic ovary syndrome". Gynecological Endocrinology. 22 (12): 680–4. doi:10.1080/09513590601010508. PMID 17162710.
- 1 2 Royal College of Obstetricians and Gynaecologists (December 2007). "Long-term consequences of polycystic ovarian syndrome" (PDF). Green-top Guideline No. 27. Royal College of Obstetricians and Gynaecologists. Retrieved 2 July 2013.
- ↑ Lilja AE, Mathiesen ER (2006). "Polycystic ovary syndrome and metformin in pregnancy". Acta Obstetricia et Gynecologica Scandinavica. 85 (7): 861–8. doi:10.1080/00016340600780441. PMID 16817087.
- ↑ van den Boogaard E, Vissenberg R, Land JA, van Wely M, van der Post JA, Goddijn M, Bisschop PH (2011). "Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy: A systematic review". Human Reproduction Update. 17 (5): 605–19. doi:10.1093/humupd/dmr024. PMID 21622978.
- ↑ Gleicher N, Weghofer A, Barad D (2007). "Female infertility due to abnormal autoimmunity: Frequently overlooked and greatly underappreciated. Part II". Expert Review of Obstetrics & Gynecology. 2 (4): 465–75. doi:10.1586/17474108.2.4.465.
- ↑ Gleicher N, Weiner R, Vietzke M (2006). "The impact of abnormal autoimmune function on reproduction: Maternal and fetal consequences". Journal of Autoimmunity. 27 (3): 161–5. doi:10.1016/j.jaut.2006.08.003. PMID 17029731.
- ↑ Gleicher N, Weghofer A, Barad DH (2011). "Do chromosomally abnormal pregnancies really preclude autoimmune etiologies of spontaneous miscarriages?". Autoimmunity Reviews. 10 (6): 361–3. doi:10.1016/j.autrev.2010.12.004. PMID 21195806.
- ↑ Tersigni, C.; Castellani, R.; de Waure, C.; Fattorossi, A.; De Spirito, M.; Gasbarrini, A.; Scambia, G.; Di Simone, N. (2014). "Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms". Human Reproduction Update. 20 (4): 582–593. doi:10.1093/humupd/dmu007. ISSN 1355-4786. PMID 24619876.
- ↑ Lis, R.; Rowhani-Rahbar, A.; Manhart, L. E. (2015). "Mycoplasma genitalium Infection and Female Reproductive Tract Disease: A Meta-Analysis". Clinical Infectious Diseases. 61: 418–26. doi:10.1093/cid/civ312. ISSN 1058-4838. PMID 25900174.
- 1 2 Ness RB, Grisso JA, Hirschinger N, Markovic N, Shaw LM, Day NL, Kline J (1999). "Cocaine and Tobacco Use and the Risk of Spontaneous Abortion". New England Journal of Medicine. 340 (5): 333–9. doi:10.1056/NEJM199902043400501. PMID 9929522.
- ↑ Venners SA, Wang X, Chen C, Wang L, Chen D, Guang W, Huang A, Ryan L, O'Connor J, Lasley B, Overstreet J, Wilcox A, Xu X (2004). "Paternal Smoking and Pregnancy Loss: A Prospective Study Using a Biomarker of Pregnancy". American Journal of Epidemiology. 159 (10): 993–1001. doi:10.1093/aje/kwh128. PMID 15128612.
- ↑ Bray I, Gunnell D, Davey Smith G (2006). "Advanced paternal age: How old is too old?". Journal of Epidemiology & Community Health. 60 (10): 851–3. doi:10.1136/jech.2005.045179. PMC 2566050
 . PMID 16973530.
. PMID 16973530. - ↑ Furneaux EC, Langley-Evans AJ, Langley-Evans SC (2001). "Nausea and Vomiting of Pregnancy: Endocrine Basis and Contribution to Pregnancy Outcome". Obstetrical and Gynecological Survey. 56 (12): 775–82. doi:10.1097/00006254-200112000-00004. PMID 11753180.
- ↑ Madsen M, Jørgensen T, Jensen ML, Juhl M, Olsen J, Andersen PK, Nybo Andersen AM (2007). "Leisure time physical exercise during pregnancy and the risk of miscarriage: A study within the Danish National Birth Cohort". BJOG. 114 (11): 1419–26. doi:10.1111/j.1471-0528.2007.01496.x. PMC 2366024
 . PMID 17877774.
. PMID 17877774. - ↑ Weng X, Odouli R, Li DK (2008). "Maternal caffeine consumption during pregnancy and the risk of miscarriage: a prospective cohort study". Am. J. Obstet. Gynecol. 198 (3): 279.e1–8. doi:10.1016/j.ajog.2007.10.803. PMID 18221932. Lay summary – The New York Times (January 20, 2008).
- ↑ Savitz DA, Chan RL, Herring AH, Howards PP, Hartmann KE (2008). "Caffeine and Miscarriage Risk". Epidemiology. 19 (1): 55–62. doi:10.1097/EDE.0b013e31815c09b9. PMID 18091004. Lay summary – Medical News Today (January 23, 2008).
- ↑ Pollack AZ, Buck Louis GM, Sundaram R, Lum KJ (2010). "Caffeine consumption and miscarriage: A prospective cohort study". Fertility and Sterility. 93 (1): 304–6. doi:10.1016/j.fertnstert.2009.07.992. PMC 2812592
 . PMID 19732873.
. PMID 19732873. - 1 2 Ross LE; Grigoriadis S; Mamisashvili L; et al. (2013-04-01). "Selected pregnancy and delivery outcomes after exposure to antidepressant medication: A systematic review and meta-analysis". JAMA Psychiatry. 70 (4): 436–443. doi:10.1001/jamapsychiatry.2013.684. ISSN 2168-622X.
- ↑ Dalke, Katharine Baratz; Wenzel, Amy; Kim, Deborah R. (2016-04-19). "Depression and Anxiety During Pregnancy: Evaluating the Literature in Support of Clinical Risk-Benefit Decision-Making". Current Psychiatry Reports. 18 (6): 1–12. doi:10.1007/s11920-016-0698-x. ISSN 1523-3812.
- ↑ Broy P, Bérard A (2010). "Gestational exposure to antidepressants and the risk of spontaneous abortion: A review". Current drug delivery. 7 (1): 76–92. doi:10.2174/156720110790396508. PMID 19863482.
- ↑ Nakhai-Pour HR, Broy P, Bérard A (2010). "Use of antidepressants during pregnancy and the risk of spontaneous abortion". Canadian Medical Association Journal. 182 (10): 1031–7. doi:10.1503/cmaj.091208. PMC 2900326
 . PMID 20513781.
. PMID 20513781. - ↑ Yonkers, Kimberly A.; Blackwell, Katherine A.; Glover, Janis; Forray, Ariadna (2014-01-01). "Antidepressant Use in Pregnant and Postpartum Women". Annual Review of Clinical Psychology. 10 (1): 369–392. doi:10.1146/annurev-clinpsy-032813-153626. PMC 4138492
 . PMID 24313569.
. PMID 24313569. - ↑ Moscrop A (Apr 2012). "Can sex during pregnancy cause a miscarriage? A concise history of not knowing". Br J Gen Pract. 62 (597): e308–10. doi:10.3399/bjgp12X636164. PMC 3310038
 . PMID 22520919.
. PMID 22520919. - ↑ "Miscarriage: An Overview". Armenian Medical Network. 2005. Retrieved September 19, 2007.
- 1 2 Conner SN, Cahill AG, Tuuli MG, Stamilio DM, Odibo AO, Roehl KA, Macones GA (2013). "Interval from loop electrosurgical excision procedure to pregnancy and pregnancy outcomes". Obstet Gynecol. 122 (6): 1154–9. doi:10.1097/01.AOG.0000435454.31850.79. PMC 3908542
 . PMID 24201682.
. PMID 24201682. - ↑ Yip SK, Sahota D, Cheung LP, Lam P, Haines CJ, Chung TK (2003). "Accuracy of Clinical Diagnostic Methods of Threatened Abortion". Gynecologic and Obstetric Investigation. 56 (1): 38–42. doi:10.1159/000072482. PMID 12876423.
- ↑ Condous G, Okaro E, Khalid A, Bourne T (2005). "Do we need to follow up complete miscarriages with serum human chorionic gonadotrophin levels?". BJOG. 112 (6): 827–9. doi:10.1111/j.1471-0528.2004.00542.x. PMID 15924545.
- ↑ Royal College of Obstetricians and Gynaecologists (RCOG) (April 2011). "The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage" (PDF). Green-top Guideline No. 17. Royal College of Obstetricians and Gynaecologists (RCOG). Retrieved 2 July 2013.
- 1 2 Doubilet PM, Benson CB, Bourne T, Blaivas M, Barnhart KT, Benacerraf BR, Brown DL, Filly RA, Fox JC, Goldstein SR, Kendall JL, Lyons EA, Porter MB, Pretorius DH, Timor-Tritsch IE (2013). "Diagnostic Criteria for Nonviable Pregnancy Early in the First Trimester". New England Journal of Medicine. 369 (15): 1443–1451. doi:10.1056/NEJMra1302417. PMID 24106937.
- ↑ Stead, Latha; Stead, S. Matthew; Kaufman, Matthew; Suarez, Luis (2006). First Aid for The Obstetrics and Gynecology Clerkship. New York: McGraw-Hill. p. 138. ISBN 978-0-07-144874-1.
- ↑ MedlinePlus (October 25, 2004). "Abortion – incomplete". Medical Encyclopedia. Archived from the original on April 25, 2006. Retrieved May 24, 2006.
- 1 2 Kirk E, Bottomley C, Bourne T (2013). "Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location". Human Reproduction Update. 20 (2): 250–61. doi:10.1093/humupd/dmt047. PMID 24101604.
- 1 2 Farquharson RG, Jauniaux E, Exalto N (2005). "Updated and revised nomenclature for description of early pregnancy events". Human Reproduction. 20 (11): 3008–11. doi:10.1093/humrep/dei167. PMID 16006453.
- ↑ Hutchon DJ (June 1997). "Missed abortion versus delayed miscarriage.". British journal of obstetrics and gynaecology. 104 (6): 753. doi:10.1111/j.1471-0528.1997.tb11994.x. PMID 9197887.
- 1 2 Royal College of Obstetricians and Gynaecologists (May 2003). "The investigation and treatment of couples with recurrent miscarriage". Green-top Guideline No. 17. Retrieved October 20, 2010.
- ↑ www.birth.com.au (October 2004). "miscarriage". Retrieved 3 January 2014.
- ↑ Rumbold A, Middleton P, Pan N, Crowther CA (Jan 19, 2011). "Vitamin supplementation for preventing miscarriage.". Cochrane database of systematic reviews (Online) (1): CD004073. doi:10.1002/14651858.CD004073.pub3. PMID 21249660.
- ↑ http://www.babycentre.co.uk/a1039515/understanding-early-miscarriage#ixzz2x52G1IYu
- ↑ Ben-Haroush A, Yogev Y, Mashiach R, Meizner I (2003). "Pregnancy outcome of threatened abortion with subchorionic hematoma: Possible benefit of bed-rest?". The Israel Medical Association journal. 5 (6): 422–4. PMID 12841015.
- ↑ Tien JC, Tan TY (2007). "Non-surgical interventions for threatened and recurrent miscarriages". Singapore medical journal. 48 (12): 1074–90; quiz 1090. PMID 18043834.
- ↑ Karanth, L; Jaafar, SH; Kanagasabai, S; Nair, NS; Barua, A (Mar 28, 2013). "Anti-D administration after spontaneous miscarriage for preventing Rhesus alloimmunisation.". The Cochrane database of systematic reviews. 3: CD009617. doi:10.1002/14651858.CD009617.pub2. PMID 23543581.
- ↑ Royal College of Obstetric and Gynecologists (March 2011). "The Use of Anti-D Immunoglobulin for Rhesus D Prophylaxis" (PDF). p. 5. Retrieved 25 September 2014.
- 1 2 3 Kripke C (2006). "Expectant management vs. surgical treatment for miscarriage". American Family Physician. 74 (7): 1125–6. PMID 17039747.
- ↑ Tang OS, Ho PC (2006). "The use of misoprostol for early pregnancy failure". Current Opinion in Obstetrics and Gynecology. 18 (6): 581–6. doi:10.1097/GCO.0b013e32800feedb. PMID 17099326.
- ↑ Babigumira, Joseph B.; Vlassoff, Michael; Ahimbisibwe, Asa; Stergachis, Andy (2015-01-01). Debas, Haile T.; Donkor, Peter; Gawande, Atul; Jamison, Dean T.; Kruk, Margaret E.; Mock, Charles N., eds. Surgery for Family Planning, Abortion, and Postabortion Care. Washington (DC): The International Bank for Reconstruction and Development / The World Bank. ISBN 9781464803468. PMID 26741012.
- ↑ Lok IH, Yip AS, Lee DT, Sahota D, Chung TK (2010). "A 1-year longitudinal study of psychological morbidity after miscarriage". Fertility and Sterility. 93 (6): 1966–75. doi:10.1016/j.fertnstert.2008.12.048. PMID 19185858.
- ↑ Miscarriage Standard Code of Practice
- ↑ David Vernon (2005). "Having a Great Birth in Australia". Archived from the original on February 12, 2008.
- ↑ Robinson, Gail Erlick (2014-01-01). "Pregnancy loss". Best Practice & Research. Clinical Obstetrics & Gynaecology. 28 (1): 169–178. doi:10.1016/j.bpobgyn.2013.08.012. ISSN 1532-1932. PMID 24047642.
- ↑ Oliver-Williams CT, Heydon EE, Smith GC, Wood AM (2013). "Miscarriage and future maternal cardiovascular disease: A systematic review and meta-analysis". Heart. 99 (22): 1636–1644. doi:10.1136/heartjnl-2012-303237. PMC 3812894
 . PMID 23539554.
. PMID 23539554. - 1 2 3 4 5 6 Ammon Avalos L, Galindo C, Li DK (June 2012). "A systematic review to calculate background miscarriage rates using life table analysis.". Birth defects research. Part A, Clinical and molecular teratology. 94 (6): 417–23. doi:10.1002/bdra.23014. PMID 22511535.
- 1 2 Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M (2000). "Maternal age and fetal loss: Population based register linkage study". BMJ. 320 (7251): 1708–12. doi:10.1136/bmj.320.7251.1708. PMC 27416
 . PMID 10864550.
. PMID 10864550. - ↑ Kleinhaus K, Perrin M, Friedlander Y, Paltiel O, Malaspina D, Harlap S (2006). "Paternal Age and Spontaneous Abortion". Obstetrics & Gynecology. 108 (2): 369–77. doi:10.1097/01.AOG.0000224606.26514.3a. PMID 16880308.
- ↑ Slama R, Bouyer J, Windham G, Fenster L, Werwatz A, Swan SH (2005). "Influence of Paternal Age on the Risk of Spontaneous Abortion". American Journal of Epidemiology. 161 (9): 816–23. doi:10.1093/aje/kwi097. PMID 15840613.
- ↑ Farquharson RG, Jauniaux E, Exalto N (November 2005). "Updated and revised nomenclature for description of early pregnancy events.". Human reproduction (Oxford, England). 20 (11): 3008–11. doi:10.1093/humrep/dei167. PMID 16006453.
- 1 2 3 Mohangoo AD, Blondel B, Gissler M, Velebil P, Macfarlane A, Zeitlin J (2013). "International comparisons of fetal and neonatal mortality rates in high-income countries: should exclusion thresholds be based on birth weight or gestational age?". PLoS ONE. 8 (5): e64869. Bibcode:2013PLoSO...864869M. doi:10.1371/journal.pone.0064869. PMC 3658983
 . PMID 23700489.
. PMID 23700489. - ↑ Li, Z; Zeki, R; Hilder, L; Sullivan, EA (2012). "Australia's Mothers and Babies 2010". Perinatal statistics series no. 27. Cat. no. PER 57. Australian Institute of Health and Welfare National Perinatal Statistics Unit, Australian Government. Retrieved 4 July 2013.
- ↑ Royal College of Obstetricians & Gynaecologists UK (April 2001). "Further Issues Relating to Late Abortion, Fetal Viability and Registration of Births and Deaths". Royal College of Obstetricians and Gynaecologists UK. Retrieved 4 July 2013.
- ↑ https://www.gov.uk/register-stillbirth | date=May 2013
- 1 2 3 Moscrop A (2013). "'Miscarriage or abortion?' Understanding the medical language of pregnancy loss in Britain; a historical perspective". Medical Humanities. 39 (2): 98–104. doi:10.1136/medhum-2012-010284. PMC 3841747
 . PMID 23429567.
. PMID 23429567. - ↑ "Standard terminology for reporting of reproductive health statistics in the United States.". Public Health Reports. 103 (5): 464–71. 1988. PMC 1478116
 . PMID 3140271.
. PMID 3140271. - ↑ Gardner RF (Jul 1, 1972). "Abortion and miscarriage". British Medical Journal. 3 (5817): 51. doi:10.1136/bmj.3.5817.51. PMC 1788537
 . PMID 5039574.
. PMID 5039574. - 1 2 Chalmers B (May 1992). "Terminology used in early pregnancy loss.". British journal of obstetrics and gynaecology. 99 (5): 357–8. doi:10.1111/j.1471-0528.1992.tb13746.x. PMID 1622902.
- ↑ Beard RW, Mowbray JF, Pinker GD (1985). "Miscarriage or abortion". Lancet. 2 (8464): 1122–3. doi:10.1016/S0140-6736(85)90709-3. PMID 2865589.
- ↑ Hutchon DJ, Cooper S (1998). "Terminology for early pregnancy loss must be changed". BMJ. 317 (7165): 1081. doi:10.1136/bmj.317.7165.1081. PMC 1114078
 . PMID 9774309.
. PMID 9774309. - ↑ Hutchon DJ (1998). "Understanding miscarriage or insensitive abortion: Time for more defined terminology?". American Journal of Obstetrics and Gynecology. 179 (2): 397–8. doi:10.1016/S0002-9378(98)70370-9. PMID 9731844.
- ↑ Hutchon DJ, Cooper S (Oct 17, 1998). "Terminology for early pregnancy loss must be changed.". BMJ (Clinical research ed.). 317 (7165): 1081. doi:10.1136/bmj.317.7165.1081. PMC 1114078
 . PMID 9774309.
. PMID 9774309. - ↑ Spencer, James. Sheep Husbandry in Canada, page 124 (1911).
- ↑ "Beef cattle and Beef production: Management and Husbandry of Beef Cattle", Encyclopaedia of New Zealand (1966).
- ↑ Fraser-Smith AC (1975). "Male-induced pregnancy termination in the prairie vole, Microtus ochrogaster". Science. 187 (4182): 1211–3. doi:10.1126/science.1114340. PMID 1114340.
- ↑ Mahady, Scott; Wolff, Jerry (2002). "A field test of the Bruce effect in the monogamous prairie vole (Microtus ochrogaster)". Behavioral Ecology and Sociobiology. 52 (1): 31–7. doi:10.1007/s00265-002-0484-0. JSTOR 4602102.
- ↑ Becker SD, Hurst JL (2009). "Female behaviour plays a critical role in controlling murine pregnancy block". Proceedings of the Royal Society B. 276 (1662): 1723–9. doi:10.1098/rspb.2008.1780. JSTOR 30245000. PMC 2660991
 . PMID 19324836.
. PMID 19324836.