Amniotic band constriction
| Amniotic band syndrome | |
|---|---|
|
A baby's hand affected by amniotic band syndrome | |
| Classification and external resources | |
| Specialty | pediatrics |
| ICD-10 | P02.8 |
| ICD-9-CM | 762.8 |
| OMIM | 217100 |
| DiseasesDB | 32457 |
| MedlinePlus | 001579 |
| eMedicine | orthoped/561 |
| MeSH | D000652 |
Amniotic band constriction (also known as "amniotic band syndrome", "ADAM complex", "Amniotic band sequence", "Congenital constriction bands" and "Pseudoainhum"[1]) is a congenital disorder caused by entrapment of fetal parts (usually a limb or digits) in fibrous amniotic bands while in utero.
Signs and symptoms
The constriction of appendages by amniotic bands may result in:
- Constriction rings around the digits, arms and legs
- Swelling of the extremities distal to the point of constriction (congenital lymphedema)
- Amputation of digits, arms and legs (congenital amputation)
A strong relationship between ABS and clubfoot (also called "talipes") exists. A 31.5% of associated clubfoot deformity and ABS can be correlated with 20% occurring bilaterally. Other abnormalities found with ABS include: clubhands, cleft lip, and/or cleft palate, and hemangioma.
Decreased fetal movement could be a sign of a serious problem which may include ABS. It is rare but possible for the membrane to become wrapped around the placenta or the neck of the baby in the womb causing strangulation and death.
Cause
To explain the cause of ABS, there are two main theories.
The amniotic band theory is that ABS occurs due to a partial rupture of the amniotic sac. This rupture involves only the amnion; the chorion remains intact. Fibrous bands of the ruptured amnion float in the amniotic fluid and can encircle and trap some part of the fetus. Later, as the fetus grows but the bands do not, the bands become constricting. This constriction reduces blood circulation, hence causes congenital abnormalities. In some cases a complete "natural" amputation of a digit(s) or limb may occur before birth or the digit(s) or limbs may be necrotic (dead) and require surgical amputation following birth.
The vascular disruption theory: Because the constricting mechanism of the amniotic band theory does not explain the high incidence of cleft palate and other forms of cleft defects occurring together with ABS, this co-occurrence suggests an "intrinsic" defect of the blood circulation.
Diagnosis
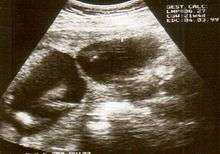
Amniotic band syndrome is often difficult to detect before birth as the individual strands are small and hard to see on ultrasound. Often the bands are detected indirectly because of the constrictions and swelling upon limbs, digits, etc. Misdiagnosis is also common, so if there are any signs of amniotic bands, further detailed ultrasound tests should be done to assess the severity. 3D ultrasound and MRI can be used for more detailed and accurate diagnosis of bands and the resulting damage/danger to the fetus.
Treatment
In rare cases, if diagnosed in utero, fetal surgery may be considered to save a limb which is in danger of amputation or other deformity. This typically would not be attempted if neither vital organs nor the umbilical cord were affected. This operation has been successfully performed on fetuses as young as 22 weeks.[2] The surgery took place at Melbourne's Monash Medical Centre in Australia and is believed to be the earliest surgery of its type, as surgeons usually hold off on operating until the woman is in week 28 of gestation. There are also several facilities in the United States that have performed successful amniotic band release surgery.
Treatment usually occurs after birth and where plastic and reconstructive surgery is considered to treat the resulting deformity.[3] Plastic surgery ranges from simple to complex depending on the extent of the deformity. Physical and occupational therapy may be needed long term.
Prosthetics may help some ABS sufferers to live more functional lives. The price and complexity of these prosthetics vary dramatically, but advances in 3-D printing have helped to increase the availability of artificial fingers while reducing their cost of production.[4]
Prognosis

The prognosis depends on the location and severity of the constricting bands. Every case is different and multiple bands may be entangled around the fetus.
Bands which wrap around fingers and toes can result in syndactyly or amputations of the digits. In other instances, bands can wrap around limbs causing restriction of movement resulting in clubbed feet. In more severe cases, the bands can constrict the limb causing decreased blood supply and amputation. Amniotic bands can also sometimes attach to the face or neck causing deformities such as cleft lip and palate. If the bands become wrapped around the head or umbilical cord it can be life-threatening for the fetus.
The number of cases of miscarriage that can be attributed to ABS is unknown, although it has been reported that it may be the cause of 178 in 10,000 miscarriages.
Prevention
Amniotic band syndrome is considered an accidental event and it does not appear to be genetic or hereditary, so the likelihood of it occurring in another pregnancy is remote. The cause of amnion tearing is unknown and as such there are no known preventative measures.
Epidemiology
Amniotic banding affects approximately 1 in 1,200 live births. It is also believed to be the cause of 178 in 10,000 miscarriages. Up to 50% of cases have other congenital anomalies including cleft lip, cleft palate, and clubfoot deformity. Hand and finger anomalies occur in up to 80%.
People living with ABS
Among the more notable people living with ABS are:
- Sophie Wells, British member Paralympics dressage team [5]
- Gina Casillas, US volleyball player [6]
- Ian T. Jamison, US artist [7]
- Anna Johannes, US Paralympic swimmer[8]
- Jean-Jacques Machado, 7th degree red-and-black belt in Brazilian Jiu-Jitsu[9]
- Monica Price, - a case study of a young woman born with amniotic band syndrome [10]
- Kingsley McGowan, - U.S. Men's Rugby Player http://usarugby.org/mens-eagles
See also
References
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ↑ "Surgeons save unborn baby's legs". News Online. Australian Broadcasting Corporation. 2008-06-08.
- ↑ Gabos PG (2006). "Modified technique for the surgical treatment of congenital constriction bands of the arms and legs of infants and children". Orthopedics. 29 (5): 401–4. PMID 16729738.
- ↑ "3-D Printer Brings Dexterity To Children With No Fingers". News Online. 2013-06-18.
- ↑ Sophie Wells website http://www.sophiewells.com/
- ↑ Superhands http://www.superhands.us/pages/casillas.html
- ↑ Single-handed art "Archived copy". Archived from the original on 2013-02-19. Retrieved 2013-08-27.
- ↑ 'Despite setbacks, swimmer takes head-first approach to reaching Paralympic gold' http://www.local12.com/ara/hottopics/story/Despite-setbacks-swimmer-takes-head-first/VpNtHBpp0U2YTLDQu0TmSQ.cspx[]
- ↑ http://www.bjjheroes.com/bjj-fighters/jean-jacques-machado-bjj-fighter-wiki
- ↑ Monica Price website http://specialneedsfamilyfun.com/family/monica.htm
- Walter JH, Goss LR, Lazzara AT (1998). "Amniotic band syndrome". The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 37 (4): 325–33. doi:10.1016/s1067-2516(98)80070-7. PMID 9710786.
- Light TR, Ogden JA (1993). "Congenital constriction band syndrome. Pathophysiology and treatment". The Yale Journal of Biology and Medicine. 66 (3): 143–55. PMC 2588858
 . PMID 8209551.
. PMID 8209551.
External links
- Amniotic Band Syndrome Diagnosis and Treatment at SSM Health St. Louis Fetal Care Institute
- -Indian ABS Awareness
- amnioticbandsyndrome.com - Information, Photos, Personal Stories of ABS
- UCSF Fetal Treatment Center: Amniotic Band Syndrome
- SuperHands Kids and Heroes Support Group for parents of kids with upper limb differences
- Cincinnati Children's Hospital Fetal Care Center resources- one of the locations that has performed amniotic band release surgery
- Support and information for families dealing with fetal syndromes such as amniotic band syndrome
- Monica - a case study of a young woman born with amniotic band syndrome
